Webinar
Achieving Health Equity for People with Disabilities During the Pandemic and Beyond
Time & Location
In the United States, one in four adults has a disability and the pandemic has disproportionately impacted this community and made it more difficult to access care. Some people with disabilities were more likely to become infected with or have a severe illness from COVID-19 due to underlying medical conditions or living situations. The pandemic also affected their psychological and financial health, with people with disabilities experiencing higher rates of unemployment than the general population. While individuals with disabilities were often given higher priority status for receiving the vaccine, many of the COVID-19 vaccine websites violated disability rights, hindering access.
This webinar explored these challenges and showcase strategies to address the diverse needs of people living with disabilities and work toward health equity. Expert panelists discussed:
The pandemic’s impact on individuals with disabilities and Johns Hopkins’ partnership to create a database on the prioritization of the disability community in COVID-19 vaccine distribution
A health plan’s response to support people with disabilities during the pandemic, expanding telehealth and increased care options, and addressing comorbidities and the needs of COVID-19 longhaulers
Addressing the intersection of disability, race, and ethnicity and the importance of cultural and linguistic competency in supporting individuals with developmental disabilities
Caitlin Ellis - Program Manager, NIHCM
Good afternoon. I'm Cait Ellis, Program Manager at the National Institute for Health Care Management Foundation. On behalf of NIHCM, thank you for joining us today. Our goal today is to share information on the impact of the COVID-19 pandemic on people with disabilities, and to discuss actionable strategies to address challenges and barriers to care, including vaccine access.
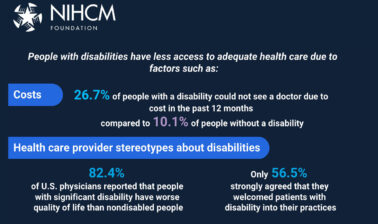
According to the CDC, one in four adults in the United States has a disability. People with disabilities are a diverse group with wide ranging needs. There are many types of disabilities such as those that affect vision, movement, cognition, and hearing, where people with disabilities barriers around communication, physical access, attitudes and social determinants of health can have a tremendous impact on their health and well being and their ability to access critical care and services. This expert panel will provide insights into how the pandemic exacerbated existing challenges and how this community was uniquely impacted. And they’ll outline some lessons learned and best practices that can advance health equity, and help support individuals with disabilities going forward.
Before we hear from them, I’d like to thank NIHCM’s President and CEO, Nancy Chockley and the NIHCM team who helped to convene this event. You can find biographical information for all of our speakers on our website, along with today's agenda and copies of slides. Additionally, please use the Q&A tab to submit any questions during the webinar and we’ll return to those after we hear from our three panelists. I’m now pleased to introduce our first speaker, Dr. Bonnielin Swenor. Dr. Swenor is an Epidemiologist and Associate Professor at the Johns Hopkins Wilmer Eye Institute, and the Epidemiology Department at The Johns Hopkins Bloomberg School of Public Health.
She's the Founder and Director of The Johns Hopkins Disability Health Research Center, which addresses health inequities for people with disabilities, and aims to shift the paradigm from living with a disability to thriving with a disability. We’re pleased to have Dr. Swenor with us today to share her work and expertise. Dr. Swenor?
Bonnielin Swenor - Director, Johns Hopkins Disability Health Research Center
Thank you so much. I'm really grateful for the opportunity to be a part of this esteemed panel and talk about COVID-19 and the impact it's had on the disability community. Thank you so much for that wonderful introduction, what I'm showing on this slide is some of my contact information and I'll go back over it at the end in case anyone in the audience wants to connect.
So my interest in the impact of COVID-19 on the disability community really started early in the pandemic and it stems quite honestly directly from my personal experience, in March 2020, I began feeling unwell after being exposed to two people who were confirmed positive COVID-19. And when I called my provider to get information on how I could get a COVID-19 test, I was told to go to a drive through testing site that had been propped up near my home. But as a person with a visual disability myself, I have a degenerative retinal disease that's led me to lose my vision over the past 15 years and I no longer drive. That suggestion honestly was laughable, drive through test site is completely inaccessible to me.
So what I'm showing on this slide is an image of an article that I wrote for STAT news about that experience and the ways in which that personal experience early on in the pandemic made me think about my work and pivot really towards the unique ways that the disability community was being impacted by the pandemic.
So, as I steered my Disability Health Research Center towards looking at the implications of the pandemic on the disability community, it became really clear early that one of the main ways the community was being impacted was around gaps in accessibility.
There were clear gaps in access to critical public health information early on, which included lack of ASL interpreters during public health press conferences or not including alternative text images or descriptions of figures and images, including those pandemic curves which held really valuable information, those gaps in information, access created inequities for the disability community which quite honestly persisted throughout the pandemic and are persisting today. Additionally, there are in many ways still remain barriers to accessing COVID-19 tests and vaccines for people with many types of disabilities.
My story is just one example. But these gaps have ranged from inaccessible testing and vaccine sites for people who are wheelchair users, lack of options to ensure communication and even consent for people who have hearing loss or that, or who have low vision or blind in vaccine testing and testing sites.
Limited spaces in vaccine sites that are inclusive are considering the needs of people with intellectual and developmental disabilities. There's also been gaps in transportation options to even guest testing and vaccine for people with disabilities.
There's also important implications of the social measures that have been put in place during the pandemic such as limitations in transit options, which I just described, and changes in how we have obtained food, medication, access healthcare, which in some cases have created unintended and insurmountable barriers for people with disabilities during the pandemic. So, for example, someone who's blind cannot tell if others around them are wearing a mask or not, or if they're maintaining the suggested social distancing during the height of the pandemic, that certainly has impacted individuals ability to stay safe while they're getting food or opportunities to interact with healthcare during the pandemic.
These gaps in accessibility have magnified inequities generated by our virtual, physical and social environments that we live in. But honestly, those inequities have been there before the pandemic.
Additionally, there is limitations and disability data that have affected the pandemic response. So at the outset of the pandemic, most of the data on COVID-19 mortality and infection for people with disabilities was coming from nursing homes, which by definition, everyone in those settings has a disability, or from other congregate care settings where people with disabilities might be living. So in the fall of 2020, approximately 40% of all COVID-19 related mortality was occurring in those settings, in those congregate care nursing home settings, which is staggering data, it’s really important though to consider that for the disability community, people in those settings is really just a fraction of the disability population.
As was just discussed, there are 61 million or one in four Americans who live, who have a disability and that does not include people living in those congregate care settings and so while there was clear and real greater risk of COVID-19 severe outcomes for people in congregate care settings, the question was what about people with disabilities in the community?
Well, it turns out, we don't do a great job of collecting disability data in a way that's allowed us to robustly track COVID-19 testing, infection and vaccine rates. To do so what we really need is disability data collected at each healthcare interaction, and healthcare settings, we routinely collect information on people's age, gender identity, race ethnicity, but information on disability is usually not collected. There were really very many important calls for better COVID-19 data transparencies from minority groups. But for the disability community, this is not an issue of transparency, it's one of inclusion, we’re not a part of core data collection to begin with.
What that has led to is inability to track outcomes, collecting disability data and healthcare interactions really is critical for more than just COVID-19. It's important to move the needle on policy for healthcare quality, safety, costs, interactions, much as we've done for other groups, this is going to transcend the pandemic this call for data.
Additionally, there's been unequalled COVID-19 data collected and reported on from across disability groups and categories. So as was just described the disability, people with disabilities are heterogeneous group. There has been better opportunities for data collection and reporting for certain groups, for example, individuals with intellectual and developmental disabilities during the pandemic, which in part has to do with funding structures put in place before the pandemic to support research for those individuals.
The number of people with intellectual developmental disabilities that are living in congregate care settings and group home settings where COVID-19 data could be collected and the ability to leverage things like ICD codes and service utilization, information from health records which isn't always possible for people from other disability groups. So while this information from people with intellectual and developmental disabilities really has been critical and I know other panelists are going to talk about this, it's been so important to advancing our understanding of the impact of COVID-19 for the disability community, we also have to remember it's just a fraction of the picture.
We need to think about the ways in which the pandemic has impacted people across the community of people with disabilities. So these gaps in accessibility and disability data, as I indicated are not unique to the COVID-19 pandemic, but instead are a reflection of deeper societal inequities that predate the pandemic.
The pandemic has taught us a really important lesson that we’re all connected, the health of each of us is intricately connected to the people and the community and the environment that we live in. But because of the gaps in accessibility and data, the COVID-19 response has often missed the mark for many people in our population. What that means is that the exclusion of people with disabilities in the pandemic response has important ramifications for all of us.
So although these inequities became evident early on in the pandemic, as the vaccine rollout began, we realize those gaps really were persisting. So my center, the Johns Hopkins Disability Health Research Center, launched a COVID-19 vaccine dashboard for people with disabilities to track state prioritization of vaccine allocation, as well as the accessibility of vaccine information on state websites, in an effort to understand these inequities.
This project was in part inspired by one of our amazing students, Sabrina Epstein, who had noted that there was variation in vaccine prioritization across states for people with disabilities. And even though this project is now no longer collecting data, snapshots from this work can be found on our website, disabilityhealth.jhu.edu/vaccinedashboard, we're working to compile summary data, and we're now conducting deeper analyses which we'll be sharing on this site.
So what this dashboard did is we collected information from all 50 states, the District of Columbia and five U.S. territories. We updated this content weekly, and we prioritized the accessibility of our information on our dashboard, because it’s so critical to share back this information and make it accessible to the disability community that we serve.
We first launched the COVID-19 prioritization dashboard, the first part of our dashboard, focusing on vaccine prioritization in February 2021 and we worked with The Center for Dignity in Healthcare for People with Disabilities as our collaborators who were supporting the backend effort and abstracting data.
We collected data on the prioritization of four groups, long-term care nursing home residents, people living in other congregate care settings, people with chronic conditions, and a group referred to as additional disability groups, that included people receiving direct support care, and live in the community.
People with intellectual and developmental disabilities were often prioritized separately, so we pulled them out and included them in that category as we did recipients of certain Medicaid programs.
On this slide, I'm showing a snapshot of our vaccine prioritization dashboard. Please note, this data is updated. It's from April 21. For each state, we listed the current phase of a vaccine rollout or who is eligible to get a shot in their arm, prioritization tier for each of the four groups we were tracking, as well as how each category was defined by that date, and the URL or the website address of the COVID vaccine site we were collecting data from.
So from this information, we also created visualizations to summarize this data, we use both maps and bar graphs to enhance accessibility and we included text summaries of these results to include what states were currently vaccinating each of the four groups we were tracking. Note again, this is all data. This is from March 31, hopefully everyone in attendance now knows that the opportunity for vaccine is wide open for adults, which we were tracking.
Our second dashboard focused on accessibility of COVID information with vaccine information. So we collected data from COVID-19 vaccine information state websites, as well as state vaccine registration website. For this part of the dashboard, we worked with WebAIM out of University of Utah, who are experts in website accessibility and developers of a tool called WAVE. WAVE is used to score website accessibility based on the content.
So working with WebAIM, we assessed the number and type of accessibility errors. We also use an additional algorithm to account for differences across websites, such as the length and the density of the web page, so we can compare across websites. We then use those scores to rank states by their accessibility score. Our dashboard compiled this data, and we share the URLs of the websites that we were using.
Similar to our other dashboard, we visualize this accessibility data and to do this, we categorize those accessibility scores into tertiles or three groups and created maps of that data. We additionally included tech summaries of our results to enhance the accessibility of our content on this dashboard.
So what was the impact of all this? Well, we launched our prioritization dashboard on February 8, we ended it on April 21 and we wrapped up our accessibility dashboard on May 19. Less than 24 hours after launching our prioritization dashboard, The National Council on Disability cited that dashboard in a letter to the National Governors Association, asking people or asking the Governors to reprioritize people with disabilities in the vaccine rollout.
Since then, our dashboard has been cited by local, state and national advocacy groups and policymakers as well as federal agencies. This project has been included in articles in the New York Times, Washington Post's Political, NBC and most recently in a Time magazine article, Dr. Kara Ayers, from The Center for Dignity in Healthcare for People with and I both discussed this project at a Biden Harris COVID-19 Health Equity Task Force Meeting. And at its peak, we had about well, we had over 2,000 unique visits per day.
I'm honestly astounded by this response. We really didn't anticipate much use at all to be honest. But it's a clear reflection for the need for this type of data, data focused on health equity for people with disabilities. And I'll also add that the majority of people working on this project identified as having a disability myself included, we certainly valued and we're focused on starting with the community and ending by giving back to the community and I think that's also part of the success.
So we're now moving to analyze the data we collected in deeper ways, as I indicated, but some best practices and lessons learned have become clear. As we've learned from other minority and marginalized groups, disability research, as I just indicated, should always start by partnering with the communities served, with the disability community. Far too often, disability research moves ahead without ensuring its focus on addressing the most pressing and important issues that that community is facing.
Disability is the only minority group that anyone can join at any time and this group intersects all gender, racial, ethnic, economic, and geographic groups, meaning disability is part of all our communities. This project has shown us the need for disability to be included in all efforts to advance health and health equity of our communities.
We must also prioritize accessibility. We've learned this lesson many times over but the pandemic has shown us the implications of neglecting accessibility. It's not just about the disability community, accessible information spaces, healthcare and other aspects of society impact everyone. Think of the broad implications of curb cuts and sidewalks and how the benefit goes far beyond the disability community.
As a data scientist, I cannot ignore the urgent need to close disability data gap. As we say at my center, who counts depends on who is counted. Without disability data, inequities will persist for the disability community. Data is necessary to identify disparities, track change and advocate for policy, and when we say that includes both quantitative and qualitative data, we truly do need both. We need data that allows us to examine the experiences of people with intersecting identities, such as disabled people from racial and ethnic and gender minority groups and from people across disability groups and categories.
I want to thank my collaborators on this work, The Center for Dignity in Healthcare for People with Disabilities, WebAIM and special thanks to our funder, without whom none of this work would have been possible, The American Association of People with Disabilities, I'm showing on the slide away, you can contact me, can go to our website disabilityhealth.jhu.edu, can follow us on Twitter at jhudisability. Thank you.
Caitlin Ellis - Program Manager, NIHCM
Great, thank you so much, Dr. Swenor for highlighting how the pandemic impacted people with disabilities including gaps in accessibility and data collection and how that affected the pandemic response and for sharing your own personal experience and how that impacted your work.
Under the leadership of Gail Boudreaux, Anthem has been investing in communities and working to support at risk populations that have been most impacted by COVID-19. To share more about their efforts, we'll hear from Merrill Friedman, Anthem’s Senior Director of Disability Policy Engagement, Merrill outlined some of the challenges that they have seen, including the digital divide and access to Telehealth and how vaccine information is accessed and vaccines distributed. Merrill brings extensive experience to our panel discussion, she has served on numerous national boards and commissions, and was appointed by President Barack Obama to the President's Committee for People with Intellectual Disabilities. We’re so fortunate that she can be with us today to share her expertise and Anthem’s work on this critical issue, Merrill.
Merrill Friedman - Senior Director, Disability Policy Engagement at Anthem, Inc.
Thank you so much. Can you hear me, okay?
Caitlin Ellis - Program Manager, NIHCM
Yes.
Merrill Friedman - Senior Director, Disability Policy Engagement at Anthem, Inc.
Perfect, thank you. So good afternoon everybody. Thanks for joining us today. I'm going to jump around a little on slides anyway. But I am going to jump around a little bit, because so much of this really was teed up earlier. So if I'm not completely aligned with my slides, please forgive me. But hopefully we'll have a fabulous discussion anyway.
I think when we look, generally speaking right across the board, and talk about health equity for people with disabilities, during the pandemic and beyond, we're all looking to the future, right, we want to know what the future is going to look like, as we're in this, some people feel we're in a transition phase of reengaging, but I don't think we can lose sight of all of the things that have occurred throughout the pandemic, because really, these disparities existed before, the pandemic really shone a light on them that was, I will hit quite astonishing.
And so I think we have to take all that into consideration as we look at reengaging, but also realize as many people are out and about, and seemingly going back to activities like where they were prior to the pandemic, that many people with disabilities, many older adults and many new people who have joined the disability community as a result of COVID do not feel like we’re coming out of the pandemic at all and so it is very much something that we need to address collectively and not lose sight of what's happened.
I’ll also talk a little bit about vaccine hesitancy, vaccine acts supporting people in this new era and how the disability community and this is already teed up, right we are, you can join the disability community at any time and throughout COVID, we have many people join the disability community. So it’s a great time to be really talking about disability advocacy, and all of the resources that exist for people with disabilities. There are long lasting effects for people with chronic conditions, as well as a swell of people experiencing mental health conditions. And then if we start to really talk about intersectionality, and the impact on people of color, people identify as LGBTQ, we need to be very collective, very inclusive at who's within these -- joining us within the conversations.
I'm going to see, if I can figure out this. Okay, there's a little bit of delay on the slide movement. So please forgive any clunkiness there. So why the disproportionate impact, people with disabilities and chronic health conditions really do rely on a lot of people for support and care and services across the board. So not every single person relies on a lot of people, but we do have a lot of folks coming in and out of people's homes, right which during the pandemic was very frightening for people. So we talked about delayed healthcare, as a country right now, really looking at some of the people disabilities and chronic health conditions that were not able to delay healthcare and so we really had to focus our work on ensuring that people who were going into people's homes were supportive, and that people were able to feel comfortable throughout that.
When we get to some of the Telehealth stuff, I always talk, work through the early, very early on in a pandemic, by about March, April, we did about three years, or five years worth of changes and advancements in Telehealth in about three weeks. And it was tough, there were some bumps and hurdles, but it really did for those people who were able to access technology, and were able to utilize the services of Telehealth, it really did help a lot of people in that process, part of the disproportionate impact relies on accessible communications and information and I probably should say lack of accessible communications and information. There are a lot of people that did not, lot of reporters, a lot of state government officials that didn't have ASL interpreting.
In announcements early on, we did not have information in plain language, information was changing rapidly and accessible formats were not keeping up. So I think this movement of saying we're going to be thoughtful, potential, agile, responsive, really has to include people with disabilities in this discussion and how we do that.
We’re disproportionately impacted, and therefore we need to be, if you want things to go right, or at least as right as they can, for people with disabilities, it really helps to have us involved at the very beginning, I thought when we started to win in Anthem, look at okay, what are we going to do, we have to change our service coordination model, we can't go into people's homes, we have to use different platforms like Zoo, and create ways for people to sign and DocuSign. And we need to engage people more frequently.
We reached out to community leaders within the disability community as well as Anthem’s National Advisory Board on Improving Health Care Services for Older Adults and People with Disabilities, we said, here are some ideas and we have but my gosh, give us your ideas, right, talk to us what works, what doesn't, I got very involved, we all did talking to our members, getting ideas from our members, because we didn't want to just find ways to try to engage with people with disabilities throughout this pandemic without asking what would even work. So I think it really just seems so fundamental. But for some reason collectively, we have a very hard time doing that. We don't do it enough.
So I'll say like on every single slide and every single bullet, please engage people with disabilities in the conversations as we prepare and work on emergency preparedness, or as we talk about how to access services, or if we're talking about what accessible communication should look like, are they in plain language, easy, read large print Braille, constantly be talking to people with disabilities to make sure that you're making things accessible and practical. Okay, I'll get off my soapbox.
There are also a lot of people with disabilities, or lower wage earners may not be able to afford some of the conveniences that other people started to afford, like Instacart. And if you've looked at Instacart, and some of these other delivery services, the prices were going up due to worker shortages, due to supply and demand. We all recalled very early on, you couldn't get toilet paper, right, you couldn't get sanitizer. So as all those prices went up, plus you had service charges that made that very inaccessible to people who is unaffordable. We talked about technology and setting up for people who were working from home and people whose jobs didn't allow for them to work from home, people were also at greater risk of contracting the virus because they may have been using public transportation.
So it's not just people coming in and out of your home, are you using public transportation, are you out about, do you need dialysis, right, do you need to get to work. So I think we have to really consider going forward preparing, and I hope not in the near future, for any other crisis like this, that we're starting to take those things into consideration and making sure that there are accommodations that exist.
I think when we talk about not even specific to COVID, there will be other opportunities for us to do better and to take the lessons learned that we have gathered throughout this last 18 months, because our system needed help before. So we need to ensure that personal care attendants of direct support professionals are considered essential health workers. They’re the ones who are saving lives on a daily basis. They're helping support people from home, we want more people to be living at home and living independently and living in their communities and engaging so we need to develop that in-home health worker and attendant care versus personal assistance services, direct service professionals, that workforce needs to grow, gain and have a trajectory of professionalism and support, should have had access ready access immediately to PPE, we move PPE to attendance and direct support professionals very quickly and have health workers, because we knew the risks both for the workers and for the individuals who are receiving care. And so I think next time we go about this, but that shouldn't even be on the table for discussion should be an automatic. That's my opinion.
But I do think, our direct care workers are saving lives and should be supported as such. Incentive payments should be included, right. We talked about all these things. We move quickly to try to get them included, but they should be part of an infrastructure. People with mental health disabilities that were experiencing exacerbations throughout the pandemic, some people were experiencing mental health condition for the first time, our mental health conservative starting to navigate not just the mental health experience, but mental health services. So we've been -- we are very closely of course with NAMI and Mental Health America to look at screenings and outreach and resources and peer platforms to help people through this time. We even had a few opportunities to test out a virtual peer support program so people can stay connected.
Let's see if I can get us to the next slide my multi-tasking today. Here we go. So we cover a lot of this right, but things need to be accessible for people. We need to get access to technology and internet, we sent lots of laptops and iPads and iPhones and different technology out to people. Chromebooks to get for young people who were trying to learn in school were other people who were given an opportunity to potentially work from home, but didn't have the access to it. And then they access to the technology for any healthcare access services.
Social and community resources, and supports my gosh, we talk about social isolation so much. And at a time, when people were encouraged to physically distance social isolation became more and more prevalent, and I remember doing a consumer’s what they called it, it was a consumer webinar early on. It was April, May, and people were saying, even just pull up in my driveway and talk to me just drive by and talk to me, people were so incredibly lonely, older adults, people with intellectual developmental disabilities, others who are not comfortable with the technology and didn't feel like that was a connecting.
We know that loneliness kills more people than smoking cigarettes. We have to find ways to help people stay connected in a virtual world, but help people feel comfortable and use the know-how right the information to be connected. And then of course, broadband is going to be one of those things we are going to be talking about for a long time. We have to extend broadband, so people have the opportunity to dial in, if you will, to do that physical access barriers have existed for forever. Clearly, people weren't seeing there, physicians and their service providers as much during that time, but I still think as we prepare more for other disasters, physical access, barriers need to be addressed.
And then attitudinal barriers for providers and others. Implicit and explicit bias have misconceptions about people with disabilities, and not acknowledging, people's ability to self-direct their care and services and live independently with the supports required to do so. And really changing the attitudes and the resources that we have formed providers with the more that we inform providers of the independent resources or the resources that help to support independence out there. The easier it will be for providers to more naturally talk about those versus other segregating care and resource opportunities. So I think we have to take all of these into consideration moving forward.
Let's see, here we got the Digital Divide. I know we've talked about it. So I'm not going to spend a lot of time on it to kind of speed up this piece here. But just remember, you met it's not a “one-size fits all,” and we need to be able to accommodate people throughout the technology wave that we all live in. My computer crashed four times already this morning. I was like praying, it wasn't going to crash during this. It is just not. It's not the be all and end all. But it certainly is a game changer that we want to rely on. And that people are asking for us.
So I'll kind of begin to close out here and say, as we look at addressing disparities for people with disabilities. We can do and provide resources all day long, but we have to be intentional. We have to talk to people with disabilities and have them in the conversation saying that I am a person who self identifies with a disability, ADHD, but having people engaged at the table. When we're talking about public health planning, this is emergencies and disasters, whether they be tornadoes or power grid outages or another pandemic, or even working through the pandemic that we continue to exist with today with COVID-19.
So I think everything starts there for me. And then finally, talk a little bit about we did form at the beginning of 2020. I think 2021, the vaccine information collaborative for people with disabilities and older adults, and we just kind of gathered lots of disability and aging leaders and said what can we do, we don't want to reinvent the wheel, we don't want to duplicate other people's work. But we want to get accessible information out to people on the easiest way. So we put a resource together, it is on the console, really talking about vaccine advocacy, and it covered a lot of things that I was talking about before. So I'm not going to go through it here, but our resources up, and we are always happy to engage and I'm happy to take questions when we get to them. I'll turn it back to Cait Ellis [ph].
Caitlin Ellis - Program Manager, NIHCM
Thank you so much, Merrill for breaking down how COVID-19 exposed existing disparities for people with disabilities and outlining. Some clear intentional steps that can be taken to advance health inequity for this community.
Our final presentation will be from Tawara Goode, the Director of the National Center for Cultural Competence at Georgetown University. She is also the Director of the Georgetown University Center for Excellence and Developmental Disabilities, and an Assistant Professor in the Department of Pediatrics at Georgetown University Medical Center. Tamara is a recognized thought leader in the areas of cultural and linguistic competence. And we were so pleased to have her with us today to discuss her work looking at the pandemics impact on people with disabilities, and how frameworks can be used to improve how we’ve approach these critical issues. Tamara? Tawara, it looks like you're still on mute.
Tawara Goode - Director, National Center for Cultural Competence at Georgetown University
All right, I found my way off mute. Thank you very much. Today my remarks will be looking at the multiple perspectives of the impact of COVID-19 of persons with disabilities have lived experience with the emphasis on data and policy. I will do my best not to repeat what has already been said by co presenters.
I am going back on slides. Previous slide and so what is it that we know about the impact of COVID-19 on persons with disabilities? So I can say that, regardless of all of the data that's been collected, we still don't know enough. And data are still indeed being collected. And as we look at some things that we do know, I won't repeat what has already been said but esteemed colleague at Ted Kennedy at Johns Hopkins. But what we do know is that people with disabilities had delayed access to care, they had poor quality of healthcare and mental healthcare. They experienced discrimination and biases by healthcare professionals, including life-saving on therapies, they experienced increased isolation, job loss, disruption and supports and services.
We also know from this literature, there's extensive deficits in the nation's current data collection system what was alluded to earlier, particularly looking at examining COVID-19. And its impact by disability, race, ethnicity, language spoken across the United States territories, and in tribal communities.
Given that we hear a lot around statistics. I thought it was really important to bring up this particular quote, I find it very powerful, and it actually drove some of the work that we have done in our publishing about the COVID experience. So that it's basically saying that statistics are people with the tears wiped away, that is a very, I find a powerful statement.
And so if we go back and we have that lens of people with the tears wiped away, during the early stages of pandemic, we at the Georgetown University Center for Excellence and Developmental Disabilities, we went about collecting just stories and experiences from a range of people they had intellectual developmental and other disabilities. And this happened between April and May of 2020. Again, just a 11 people. These individuals were from diverse racial, ethnic, and cultural backgrounds. And getting these stories, it really gave us a chance to look at the statistics before the tears could be wiped away. So in other words, we're able to look at the social cultural context of the lives of individuals living in the District of Columbia during COVID-19.
I want to share with you a framework that we use to analyze these -- just these 11 stories that they were on, they were indeed powerful. This is a framework you can access on our website. We call it disabilities disparities framework. And if we look at public policy and resources, and think about that, during a time of COVID, we know that those public policy resources, both in the public and private sector had a significant impact on the level above, meaning, the availability of supports and services including healthcare, the accessibility, the acceptability, the quality, and the utilization.
And as we think about the accessibility, the acceptability, and in particularly the acceptability, I think, what around the cultural implications of what that is. Sometimes services were indeed available, but they certainly were not acceptable to the individuals who need that. And again, as we think about people with disabilities during this COVID pandemic, and in every aspect of their life, it really has a significant impact. So we use this framework to analyze data.
And so among the 11 people that we saw, that had intellectual developmental on other disabilities, we found that nine of the 11 had issues around accessibility. Eight of the 11 it around availability, acceptability, as indicated in slides that you see, quality is one of the 11. We know that each person experienced disruption and utilization of services due to widespread impact of the pandemic. And they had major limitations on aspect of their lives as it many others across the country.
All of the persons who were interviewed reported disparities and supports and services that included health and mental healthcare, and home supports, physical and other therapies, public transportation, employment, and again, the days that they were able to work performing independent activities of daily living, and the facility-based services and closures.
We also knew in terms of access to the capacity to use technology, which has been referenced repeatedly, what we did see is that many people could not indeed access what was needed, because everything, almost everything was web based. And then finally, when we look at the mental health impact, we saw fear, vulnerability, anxiety, frustration and isolation that really impacted at least these individuals that we heard their stories.
All right. Another effort in which we were engaged during this period of time, was an outside of the report grant that we have reconcile in the past and changing the future. And we're looking at engaging young adults with intellectual and development disabilities, who also have mental health needs and researchers and research.
In this project, we were able to get additional funding to use an analytical framework and an existing database to identify service experiences, outcomes across diverse populations. And we did this in real time.
My partners in this are the University of Florida, Jessica Kramer, and Joan Beasley, the Center for START Services at the University of New Hampshire that has a focus specifically on individuals with intellectual developmental disabilities who also have mental health needs. We were engaged in this research together.
We use this framework that I created called the Convergence of Cultural Contexts. And as you can see, in the middle, there's a child, youth, and adult and this is really looking at the multiple cultural identities and the cultural context that that child, youth, and adult may bring to the table. In this instance, a personal disability. In the next circle, we see the family and so that we look at the impact of the family, they again, the cultural context in which the child family and adult are living. And then we've looked at that child family adult again within a cultural context of the communities in which they live across the country.
And lastly looking at the socio-economic, political and demographic environment, and that was impacted significantly by COVID. So we use this framework that we use in many ways to analyze that an existing data set. In the outer ring that you will see are the many, many different services to persons with intellectual developmental and other disabilities may need to access and so from the healthcare system, to early intervention, to mental health care system, et cetera. But what was the impact of COVID for this particular population.
And so again, the sheer -- these are things that we were able to glean from the data so that the Center for START Services administered a tool, a survey for caregivers of persons with intellectual development, disabilities of mental health needs. There are about 1,455 surveys that you indicate, as you see there. So this was during March and July of 2020, collecting these data. And so things that we learned just using this convergence of cultural context framework was the sheer number of systems and sectors that family caregivers needed to navigate in order to meet the needs of their children, or adults during this time period.
We found that there were disparities and service systems needs and use based on race, ethnicity, language spoken, and other cultural factors, which we're able to glean from using this framework. And we also looked at the extent to which telehealth and virtual services were available, accessible, acceptable and utilized by the caregivers, and that vary significantly, given this specific population. So looking at telehealth as a “one-size fits all,” that was not always a good piece of that.
And lastly, the impact of the pandemic on the person with intellectual and development disabilities, the caregiver, and the family unit as a whole. But we were able to do that using this framework to examine the social cultural environment and the communities in which they live. And so again, as we think about an answering the question, like what do we know about what impacts people with intellectual and development disabilities during the time of COVID, using different ways to examine that's really very important.
The last one I'd like to share with you is a conference or a symposium that was convened in May, entitled eliminating compounded disparities for people with disabilities and a year COVID-19. It really looked at the experiences in New York city, however, the persons who contribute to this were perspectives from across the country. And these are the panels that were offered. I had a large role in planning this symposium, but understanding the political determinants of health than their impact on persons with disabilities, the lived experience, specifically communities of color, disability in the physical and mental health impact of COVID-19, which you've heard alluded to already, public policy and government response and a pandemic, the lessons learn. And lastly, the way forward.
And so as we think about not only what we should be looking at a systematic way of being able to do that, in addition to data collection, as this this symposium shared to engage members, diverse members across the country, and in specific geographic locales. These were the partners, as you see here on Pace University, HRC, New York, the Mayor's office, their Department of Social Services, and Trinity Church, Wall Street, again, engaged in the faith community in these efforts.
So I'd like to be able to summarize. My closing thoughts are that COVID-19 is still with us. And it probably is going to be with us for many years to come. And we have to continue this learning about the impact on persons with disabilities. One particular area that's a huge deficit has been alluded to by both my co presenters is that we have to collect, analyze and report data that's inclusive of the cultural context, including race, ethnicity and primary language but to go deeper for that, looking at a socio-economic status and other cultural factors. These eight things are key and critical when we think about how we are looking at prevention, treatment and other supports for persons with intellectual developmental and other disabilities for future public health emergencies.
And lastly, it really is essential that our knowledge about the impact on persons with disabilities that is not simply limited to quantitative data. Again, I can't emphasize that enough, we have an obligation to really collect data in many, many different ways in which we can gain insight. This has impact on how policies inform, our resource allocation, the needed supports and services, in order to advance equity.
Lastly, I want to end on the work of Daniel Dawes, who was a keynote for that conference. And he's placed a lot of emphasis on policy. And I think that we talk about the social determinants of health a lot. However, in his wisdom, for every social determinants of health, there was some proceeding legal, legislative, regulatory, or other policy decision that resulted in the social determinants of health. And those are the political determinants of health. So as we continue to look at the experiences of persons with intellectual, developmental, and other disabilities across the lifespan, and during our COVID pandemic that we cannot ignore the political determinants.
And with that said, I will stop I know that we need time for questions.
Caitlin Ellis - Program Manager, NIHCM
Great, thank you so much Tawara for sharing those powerful narratives and the value of using frameworks to better understand the issues and inform the response. And for sharing information about the symposium. We would like to use the remaining time to engage in a Q&A session with our audience. Please continue to submit your questions in the Q&A tab. I'll ask our panelists to come off of mute. We have had several questions come in around the impact of the pandemic on children with disabilities and their families. And I was wondering if anyone could speak to what you have seen, perhaps around the loss of school-based services, and how you're thinking about families with children with disabilities. As you're looking at your efforts, if there's any partnerships or resources or information that you think would be valuable to the audience.
Tawara Goode - Director, National Center for Cultural Competence at Georgetown University
This is Tawara. There was a sizable number of children and the data that was collected from the Center for START Services. And one huge thing that I can say is that that was around education. And the fact that the online and virtual options for education did not work very well with many of the families, particularly families or children with autism, and other disabilities. But they had great degree of difficulty. So I will share that also think that we don't have a lot of data that's been collected and reported on the impact of the education in particular, perhaps in the area of healthcare, overall, in terms of the impact of children with disabilities, and their families.
Bonnielin Swenor - Director, Johns Hopkins Disability Health Research Center
All right. This is Bonnie talking a second that comment. I think we do need much more data to look at this really important issue. I'll also add that I do think that there were some kids with certain types of disabilities that maybe did benefit from a virtual learning environment. And this is what data would help us dig into and understand more and to doctor had excellent ending of we need both quantitative and qualitative data to really know more about that. Also add another layer here.
I know that the question was, perhaps specifically about children with disabilities. As a parent with a disability with two kids in virtual learning, we also have to think about it from that angle, right. So parents with disabilities, sometimes the content for their kids where they had to engage their children, who may or may not have disabilities themselves was not always equitably accessible.
Caitlin Ellis - Program Manager, NIHCM
Great. Thank you so much for those responses. A few of our speakers have noted that many people joined the disability community during the pandemic due to COVID-19 and long haul COVID. Is anyone able to expand on what is needed to support this emerging and growing population? And are there resources or best practices specific to their needs?
Merrill Friedman - Senior Director, Disability Policy Engagement at Anthem, Inc.
So I can jump in here a minute here. I think it's many of the same resources that we use to inform people who newly encounter disability as they age, right at any age, and so it is really a lot of provider education, ensuring that we are socializing the services, whether it be at University Center for Excellence on Disability or an Independent Living Center, or the Autistic Self Advocacy Networks putting people with IDD or the National Council of DD Councils, right, or the AAA's are just really making sure that we're elevating those resources that exist in the community for people. And that when we look at peer support, and we start to look at people who may experience limb difference now or chronic lung and respiratory diseases, mental health conditions are all lots of different disabilities that are sticking with people at this particular point, that probably wasn't the most articulate way to say that.
We really do need to make sure that we are informing people of those resources that are out there for them, like we would for anybody else. And then part of that, that is also building the capacity of communities to continue to support people with disabilities, because the number of people with disabilities continues to grow anyway. So adding the number of people who were considered long haulers right now and experiencing disabilities or in chronic health conditions would be supported through those processes. And I think data has been mentioned so many times that we really do need to collect the data on what people are experiencing. So we know where to really build our capacity and our resources.
Caitlin Ellis - Program Manager, NIHCM
I’d like to comment just a little bit on that, especially, I guess the phrasing and the question about resources and best practices like to really separate resources from best practices. I don't think we know enough to really say this is a best practice, it is way too early on. And then as we think about on this notion of then moving to evidence-based practice, I would say evidence-based for home. So in absence of comprehensive, multi-faceted way in which we're looking at data, using a cultural lens, that I would say that perhaps some of the resources work for some of the people. And I would say that perhaps some of the resources do not work for other people, and that we just simply don't have enough data to say what is a promising practice at this point in time.
Bonnielin Swenor - Director, Johns Hopkins Disability Health Research Center
Yes, I also. This is Bonnie, want to add. I think that is such an important and often missed nuance, right. And that's really been elevated in the time of COVID. Not just for the long haulers. But for the disability community in general, in the absence of data, and the pursuit of equity. How do you move forward when the focus is on evidence? And I think that's just such an important question we need to think more about. I also just want to add that, Merrill commented about community and I think that's important in such a critical challenge for this group of individuals who are in new community within our community of disability.
So many people from various areas of the disability community will contact me or my center because they want to know people like them. And that's such an important part of the experience in navigating life. And I sometimes think we can overlook that. People with disabilities are the experts have their own lives. And so I think sometimes having autonomy and confidence in that expertise comes from getting to know other people like them. So my point is, is I don't think this community is growing. There's some strength there, but how do we support that community as well as addressing the inequities and maximizing health for this group to be determined.
Caitlin Ellis - Program Manager, NIHCM
Great, thank you all. Unfortunately, we are out of time. Today, I would like to thank all of our excellent speakers for being with us and sharing their valuable work and perspectives. Thank you to Barry Samuels who provided our ASL interpretation during this event. And thank you to our audience for joining us for this important discussion.
Your feedback is important, please take a moment to complete a brief survey which can be found at the bottom of your screen. We do have other resources available on our website that may be of interest, including additional materials from our speakers, and NIHCM’s ongoing work on COVID-19 and racial equity. We will also be releasing an infographic on disability. So please stay tuned. Thank you so much for joining us again today.
Speaker Presentations

Bonnielin Swenor, MPH, PhD
Director, Johns Hopkins Disability Health Research Center

Merrill Friedman
Senior Director, Disability Policy Engagement at Anthem, Inc.

Tawara D. Goode, MA
Director, National Center for Cultural Competence at Georgetown University
Closed captioning and an ASL interpreter is available
More Related Content
See More on: Health Equity | Coronavirus