Webinar
Climate Changes Health: Moving Towards Environmental Health Equity
Part of "Climate Changes Health"
Time & Location
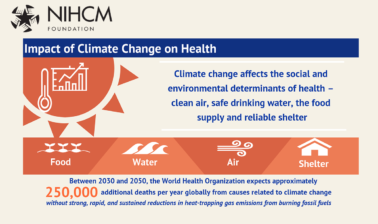
Over the last 50 years, human activities, particularly the burning of fossil fuels, have released sufficient quantities of carbon dioxide and other greenhouse gases to trap heat in the lower atmosphere and affect the global climate. Each of the last three decades has been successively warmer than any preceding decade since 1850. Sea levels are rising, glaciers are melting and precipitation patterns are changing. Extreme weather events are becoming more intense and frequent. The overall health effects of a changing climate are overwhelmingly negative. Climate change damages many of the resources that are social and environmental determinants of health - clean air, safe drinking water, sufficient food and secure shelter.
This webinar explored the interconnectedness of climate change and health, environmental injustice, and what can be done to combat these issues. The expert speakers will talk about solutions that can improve health outcomes. Speakers will discuss:
Priorities for the newly formed Office of Climate Change and Health Equity at HHS
How climate change is creating new inequities and exacerbating those that already existed, and what can be done to protect populations on the frontlines
A health plan’s efforts to combat climate change and prioritize health resilience for its members and community
0:04
Hello, everyone, and welcome to today's webinar.
0:08
Climate Changes Health: Moving Towards Environmental Health Equity.
0:14
Before we get started, I would like to go over a few items, so you know how to participate in today's event.
0:22
We've taken a screenshot of an example of the attendee interface.
0:26
You should see something that looks like this on your own computer desktop in the upper right corner.
0:33
When you joined today's webinar, you selected to either joined by phone, call, or computer audio.
0:40
If for any reason you would like to change your selection, you can do so by accessing your audio pane and your control panel.
0:49
You will have the opportunity to submit text questions to today's presenters by typing your questions into the questions pane of the control panel.
0:59
You may send in your questions at any time.
1:02
We will collect these and address them during the Q&A session at the end of today's presentation.
1:10
I would now like to introduce Kathryn Santoro, Director of Programming at the National Institute for Health Care Management.
1:21
Thank you, and good afternoon, I'm Kathryn Santoro, Director of Programming at the NIHCM Foundation. On behalf of NIHCM, thank you for joining us today for this important discussion.
1:33
Climate change is the single biggest health threat facing humanity. And the World Health Organization expects approximately 250,000 more deaths per year, globally from causes related to climate change.
1:47
Today, we will hear from a prestigious panel of experts to discuss the impacts of climate change on health and solutions to improve health outcomes.
1:57
Before we hear from them, I want to thank NIHCM president and CEO, Nancy Chockley and the NIHCM team who helped to convene today's event.
2:06
You can find full biographies for our speakers along with today's agenda and copies of their slides on our website.
2:14
We also invite you to join the conversation today on Twitter using the hashtag climate change us house.
2:21
I'm pleased to introduce our first speaker, Dr. John Balbus, the interim director of the new Office of Climate Change and Health Equity within the Office of the Assistant Secretary for Health, a physician and public health professional with over 25 years of experience working on the health implications of climate change, including roles in the federal government since 2009.
2:46
We're so honored to have him with us today to share an update on the priorities of the new Office of Climate Change and health equity.
2:55
Great. Thank you so much, Kathryn, and to the NIHCM team for holding this webinar. And for the honor of being able to speak to all of you.
3:04
It's, it's really a delight to be able to share what's going on with our Office of Climate Change and Health Equity and also to share this webinar with, with our wonderful panel.
3:17
The first slide, please.
3:18
So, I've been asked to give a bit of an overview of the impacts of climate change on health, and I'm going to, that onto health systems, as well. And think of it in terms of not just the people, but also the health care delivery systems that serve those people.
3:31
I'm going to say a little bit, and show, actually some images to help.
3:36
Can they, why it's important to link health equity to climate change, and what those linkages look like.
3:43
Then, lastly, I'll have the opportunity to describe our office a little bit in the role that we're trying to take in helping hostesses prepare for climate change. Next slide, please.
3:54
So, this is a slide that I've borrowed from my colleague George Luber at the CDC, that links up from that center ring, the manifestations of climate change that we see physically, the rising temperatures, the increasing frequency and severity of weather extremes, the rising sea level, and the actual increase in carbon dioxide concentrations Which have their own impacts.
4:17
And then the next ring is showing that there are many different ways that those primary changes in climate and impact our health.
4:25
And I think, as managers of health systems, as people who are caring for public health, the message here is that there are a lot of different things that we have to think about and they operate on very different timescales.
4:38
So, some of the impacts of climate change are related to extremes and anomalies and weather, severe heatwaves, extreme precipitation events that can lead to flooding.
4:48
Storms that stay over one area and lead to devastation from wind and flooding, and are really in the realm of emergency preparedness and disaster management.
4:59
Whereas, other kinds of manifestations of climate change, things like warmer winters than we used to have earlier Spring's changes in precipitation patterns on a seasonal basis can change vector ecology or can change the productivity of agricultural systems and lead to much longer-term kinds of changes.
5:17
and where we see certain kinds of vector borne diseases. For example, the spread of Lyme disease northward up into Canada, or malaria, and dengue climbing the slopes of the Himalayas, because warming temperatures there.
5:31
And then, lastly, there are a lot of impacts that are complex and societal in nature.
5:37
And some of these are because relate to the mental health impacts that populations experience, especially populations tied to the land like Native Americans in person, or person First Nations, folks in this hemisphere who are witnessing, you know, massive changes in their natural environments.
5:58
That that change the way that they live and really have massive impacts on where they can live.
6:03
And they're their entire cultural well-being.
6:07
All the way through to some of the things that we're seeing in different parts of the world.
6:11
Whether it's from inundation of low-lying habitat or the drying up of water supplies and forced migration that has really profound and existential kinds of threats to living in certain places.
6:25
So again, a wide range of health impacts that outer ring is a subset of the diseases that are affected.
6:32
So, you know, from a clinical standpoint, there's a lot of different types of medicine, a lot of different practices, a lot of different types of facilities, and systems that are impacted.
6:44
Next slide, please.
6:47
And what I want to convey is that, not quite well.
6:53
Everybody is, to some extent, exposed to the changes in heat to the extreme weather events.
6:59
Not everybody bears the same burden, and, as we see with coven, the people who are most at risk from climate change impacts are the people who are already saddled with health disparities.
7:10
And the burden of degradation of the basic social determinants of health, Including both those that are related to economic opportunity, but also to the natural and built environments.
7:21
People who are living in urban heat islands, people who are living in neighborhoods where the infrastructure has not been maintained, as well as others, they'll see pictures of what this really looks like.
7:33
But the point is that the social determinants of health, that covert has certainly brought to the fore as being something that all health systems need to be thinking about.
7:43
Um, pertains also to these exposure pathways and to who's put in harm's way, and then who has the greatest risk from being exposed to heat, to wildfire smoke, to changes in allergens, to mold exposures from flooded homes.
8:02
And, again, As with coven, people and populations who have higher rates of underlying chronic conditions.
8:09
This could be hypertension, diabetes, obesity, uh, anxiety and depression are the people who are going to be most at risk from these climate change related exposures.
8:20
Next slide, please.
8:23
So, what does this mean for health care systems?
8:25
This is just a quick cross code of what we were just talking about.
8:30
So, their specific populations that are at greater risk, This may be because of life stage, like the elderly or children, it may be because of racial and social discrimination and other factors conditions. Recent immigration that may lead to people having less resources, low income.
8:51
It may be people who have, living with disabilities, from either accidents, or conditions of birth, et cetera, um, but for each of these populations that our health care systems are ensuring quality care for.
9:07
There are specific health outcomes that the health care systems need to be aware of and need to be aware of.
9:15
Trends that that are increasing exposures over time.
9:18
It needs to be also aware that we're seeing, you know, multiple threats at the same time.
9:24
So, the way that we have seen the vaccination and testing, uh, tense and, and, and, you know, makeshift facilities, sometimes they're temporary facilities for coven be Threatened by heatwaves and Hurricanes and Floods.
9:39
We have to be thinking in a more flexible manner about the delivery of health care systems, in a setting where there are both threats to the people, and also breadth to that, to operations, into the continuity of operations.
9:53
Next slide, please.
9:55
I just wanted to share a resource; this is a dynamic, interactive resource on the web pages of the New England Journal of Medicine.
10:06
But I just thought it's, it's, it's one of the few places where you can see a really well thought out framework or how climate change interacts.
10:17
Not just with Human health, which is the left box, there, at the top, but with health systems and healthcare delivery.
10:23
So, you can see their impacts of climate change on everything from, you know, the costs to services.
10:28
The cost of utilities, to the utility utilization of those delivery systems, because of, you know, either heat stress or other factors that are causing people to seek care in emergency rooms to the disruptions of the systems.
10:43
Because of power outages or flooding, as well as to the stresses on public Health in general.
10:49
And then on the bottom there, you can see the different modalities of how health systems can make themselves more resilient in the face of climate change related threats.
10:59
Next slide, please.
11:02
So, just to go back and to show some of the ways in which health equity and climate change intersect.
11:11
What I'm going to show now are a series of maps and pictures that are highlighting some of the recent research that is linking, systemic and longstanding racial discrimination.
11:24
As manifest by the creation of maps by the Homeowners Loan Corporation and the National Association of Real Estate Boards in which neighborhoods were characterized according to their financial risk.
11:40
And, there was a four-color code where green was the lowest risk red was the highest risk.
11:46
And, any neighborhoods that were demarcated in red would be in general deprived of access to low interest loans and sometimes to finance on loans at all.
11:58
And, historically, those areas that, of cities that were already segregated, that already had the highest proportion of African Americans, people of color, recent immigrants, were uniformly those, those neighborhoods, But those people were found, were in the red zone.
12:18
And recent research has, is demonstrating that that has profound implications for the social determinants of health, health disparities.
12:26
So, this is just a side-by-side of one of those homeowner’s loan corporation maps of the fertile crescent of New Orleans dating, back to the 19 thirties.
12:35
Next, to the satellite image, after the Levy's Broke, just showing how the deprivation of Financial Resources is associated with the risk of inadequate infrastructure in this case, from flooding.
12:50
Next slide, please.
12:52
This is just a sequence of several maps and I'll go through them pretty quickly.
12:55
This is one of the early maps from 1923, even before this was systematized into the nation's financial system of a Richmond residential security map.
13:08
And you can see that up to the, to the north-west, to the left side that's the green and blue zones, and off to the east and to the south. Those are the red zones. Next slide, please.
13:19
And this is a map showing that those zones are associated with the built environment, so this is a map of tree cover, and you can see on the left side, there, the western side there, neighborhoods are greener, on the right outline those red line neighborhoods. And of course, now the center district is, doesn't have trees. Because that's off skyscrapers.
13:41
But even to the East, you can see those Eastern red line neighborhoods, that much less green space, tree cover in this case, compared to the west side. Next slide.
13:52
This is also of course related to impervious surface. This is a map of impervious surface.
13:56
On the left you see that the zones look wider.
14:01
That's because they have less impervious surface, the darker gray on the right, more impervious surface, which means cement, which means trapping of heat and trapping of runoff and greater risk of flooding.
14:14
Next slide, please.
14:15
So, if you have less tree cover, more concrete, you have higher summer temperatures, and that's what this map shows.
14:21
The upper left Western districts are blue on their cooler.
14:25
The red line districts are orange. And 10, they are hotter.
14:30
And so, redlining that was put in place in 19 23 is manifesting now in 20 22 as urban heat island, and greater exposure to heat.
14:41
And you can imagine greater exposure to transportation related air pollution and other kinds of health threats as well. Next slide, please.
14:49
So, with that, let me pivot and discuss our office.
14:52
Of course, our office was part of the mandate, provided to the Administration by the incoming President of Joseph Biden.
15:03
There were three mandates given to the Department of Health and Human Services by Executive Order 1408, tackling climate crisis at home and abroad.
15:12
In addition to creating our office, we are also mandated to set up a new inter-agency working group to co-ordinate the federal agencies in protecting that was most at risk from climate change and bringing a health equity lens to it as well as a biennial health care System Readiness Advisory Council of relevance to health systems managers.
15:33
Next slide, please.
15:35
Um, I'm sharing these quotes that were, uh, released at the launch of our office, which just took place a few months ago, August 31st, because they convey kind of the different dimensions of why I think this is a new day for climate change and health.
15:52
Secretary Becerra talked about the kind of the moral imperative, and his quote, his history will judge us for the actions we take to protect our world and our health from climate change.
16:03
Admiral Levine, this HHS Assistant Secretary for Health, where the office is situated in her, her office, highlighted the health equity aspects of this.
16:14
And the, the relationship between the lessons learned from Code 19, and the, the inequities faced throughout our nation by COVID-19, How these are the same group struggling the most with the effects of climate change on our health.
16:28
And then Regina McCarthy, former Administrator of the EPA, and now the national climate Advisor.
16:34
That's something very important, which is recognizing that America's world-class medical community.
16:39
In other words, our health sector, and bringing the health sector into the fight against climate change, it is a very significant event, and the next slide will talk about what's going on in that space.
16:53
So, the picture in this slide is a picture of Admiral Levine at the conference of parties, that 26 Conference of parties meeting in Glasgow, the big international UN sponsored climate change meeting, where the new, the Paris Climate Change Protocol was, was derived from the Kyoto Protocol, et cetera.
17:16
This COP26, I think, will go down as one of the most important events in the history of climate change and health.
17:24
In part because of the event that was captured here, which was the creation of a cop 26 Health program, which, for the first time, health ministries around the world came to the cop and made commitments to, that are highlighted on the bottom there, to resilient health systems and low carbon health systems.
17:42
And, no, this was the first time the US had an official delegation from the Department, Human Services.
17:50
I do think that this elevation of the health sector in the space of a global climate policy will be transformative in mobilizing people's opinions and actions to, to address the climate crisis.
18:03
And so, I won't read them, but you can see the language that we put to what we were doing as the United States for resilience, health systems and low carbon health systems.
18:14
Uh, in particular, in the low carbon health systems.
18:17
Pulling together the federal health systems.
18:21
Which already had a mandate, you know, from the, by the administration's targets, to, to reduce, to, to account for greenhouse gasses, and set and plans in place reduction plants.
18:33
And also, to partnership with the private health sector in the United States to share best practices and to bring the levers of the federal government, to bear the incentives, financing.
18:44
And ultimately, as secretary of this, they're made clear, use of regulatory authorities, if needed and as needed in the future, 2 to two, harmonize the health sector of the United States in these goals.
18:57
We divide our work into those three priorities that you see there. The first being, protecting the most vulnerable from the health impacts.
19:05
The second, recognizing what we've been discussing in terms of social determinants of health, and the power of climate actions to address the transportation infrastructure, the green space in our neighborhoods.
19:16
And so, to work with those sectors to address quality of life, social determinants of health, and address some of those root causes of health disparities to make people more resilient.
19:27
And then the third priority area, the Health Sector Resilience. Next slide, please.
19:33
And to codify that federal health system decarbonization after the cop in early December, a new executive order with this title catalyzing America's clean energy economy through federal sustainability. Said very specific targets for buildings, for fleets, for energy supplies, for the federal health system for the federal government, which includes the federal health systems of the Department of Defense of the Veterans Administration.
20:01
And the Indian Health Service.
20:04
Community Health Centers at HRSA, medical centers, at NIH, et cetera, all need to comply with this executive order, and so this is the federal government really walking the walk, as we try to nation towards these decarbonization goals.
20:19
Next slide, please.
20:23
I will go quickly through these, but just some of the details in terms of the steps that we're taking in our early life, with just a few months old.
20:33
On our Priority one, we are working with items that are actually part of the Justice 40 agenda, like, two, efforts to make the low-income Household Energy Assistance Program, and also some of the Medicaid flexibility, more available to people to be able to address heat stress and be able to help low-income populations with energy costs. with purchase of air conditioning units. As you know, work with people who are most at risk.
21:04
And we're also working, as an office to convene the power of all the agencies across the federal family to address extreme heat. We've still been working there and then we have that inter-agency working group on vulnerable populations more broadly. We've been mandated to create.
21:23
Next slide, please.
21:26
In terms of the actions to reduce to reduce health disparities, we're engaged in a lot of conversations with, with CMS, with HRSA, with other parts of HHS, about ways that the current efforts to really start to identify deficiencies in the social determinants of health, whoops, sorry, deficiencies in the social determinants of health.
21:52
And their role in health disparities. Through things like zip codes. To bringing them into the role of health systems.
21:58
To address the upstream social determinants, to make sure that those social determinants associated with climate change, with built environments, with housing, energy, security, as well as food security, can, start to get incorporated. And then ultimately to help build capacity to look at the health implications of infrastructure, projects working across the sectors and those agencies dealing with transportation housing, etcetera. Next slide, please.
22:26
Then in the area of health sector, resilience and decarbonization, our cop 26 commitments were really the big move so far.
22:34
And then, as mentioned, we're working with our Federal Health System Partners, too, too.
22:40
Identify those early steps. The key levers we can take to move all of the health systems to the federal government.
22:47
And then bringing our federal partners together with the private health sector, especially through a National Academy of Medicine initiative that's going on to identify the best practices and try to harmonize practices in the right with the private health sector, as well.
23:02
Next slide, please.
23:05
And, as a piece of this, we are starting to work with our colleagues at CMS on gaining, you know, walking down that path that, that, that it takes to get change in the policies, practices, support, and, and, and reimbursement the policies of CMS.
23:29
Starting with, with this Request for Information, so this is a quote from a proposed notice of proposed rulemaking.
23:36
I think it's closing tomorrow, so, if you have not yet seen it, and had an opportunity to weigh in, please do.
23:44
But we have language in there saying that HHS wants to explore how exchanges in their constituent organizations can more fully prepared for the harmful impacts of climate change on their enrollees, and there's a lot of specifics you find that. Next slide, please.
24:01
And, next slide.
24:05
So, in summing up, I've listed some of the possible policy areas for exploration with those of you who are listening in.
24:16
Um, there's areas that we can shore up the resilience of health systems and communities.
24:22
There are many different entities across the federal government that work on regional networks of hospitals and public health systems for preparedness.
24:30
There's the preparedness of health systems and the policies through the Emergency Preparedness Rule. We're looking at all of those things to make sure that there are gaps that people are falling through.
24:42
We're looking at the flexibilities and innovation programs for supports to, to vulnerable beneficiaries, too, for housing, for energy security, looking at climate sensitive indicators into the measurement updates.
24:54
We started with that RFI, and then looking in ways that we cannot just say, Well, these are the things you need to do, but to actually make it easy to do them, buy it by finding the financing buy in.
25:06
Resources that we can, especially for those.
25:09
Hospitals already strapped, especially for those systems, caring for the most vulnerable, which tend to have the thinnest margins to start with.
25:17
And also, to find ways to give that technical assistance, to make it easier for health systems. to look at some of the decarbonization resilience steps.
25:28
On the decarbonization side, we're looking at evidence-based actions.
25:32
Scope's wanted to, or what, uh, the hospitals have the most control over one being direct emissions of greenhouse gasses to be those associated with Energy Supplies.
25:43
Its Scope three, that's the bulk. Scope three are those associated with supply chains.
25:48
And we're working very hard in a number of different ways to identify ways to, to bring our suppliers into the path of decarbonization and end resilience as well.
26:02
Many of which many corporations, many leaders in that sector, are already walking down that path very far.
26:09
We're looking to come up with easy ways to do the greenhouse gas accounting, and to be able to publicly share that through tracking tools, to increase the technical assistance in. Looking at those ways that we can work on the financial incentives.
26:23
Again, to remove as many barriers as we can to the progress that we know we have to take to make the health sector one of the partners in addressing the climate crisis.
26:35
Next slide, please.
26:38
So, with that, I'll close, I look forward to the discussion we're going to have, especially look forward to the next couple of presentations, bringing, bringing you, I know the real-world perspective, and making all this real.
26:51
Please do visit us online at our web, at our website. We are going to be building that out over the coming months.
26:56
We will, and be sure to sign up for our listserv there, because that'll be our primary way of communicating what's going on, sending updates, alerts, and helping to build the resources for the local community.
27:09
Thank you very much, and I'll close that.
27:12
Thank you, Dr. Balbus, for your leadership on this issue. We look forward to continuing to hear about your work, and exploring partnerships with the leaders on this webinar today.
27:23
Next, we will hear from Heather McTeer Toney, Vice President of Community Engagement, at the Environmental Defense Fund. In 20 14, she was appointed by President Barack Obama as Regional Administrator for the Environmental Protection Agency south-east Region. Known for her energetic and genuine commitment to people, all her work has made her a national figure in the area of public service, environmental justice, and community engagement. And we're so honored to have her with us today.
27:55
Heather?
27:57
Hello and thanks so much. And thanks to all of you all for joining us. Today I'm coming to you from the land of the Chickasaw and Choctaw people in what we know as the State of Mississippi, Oxford, Mississippi. This is my home and I'm very glad to be sharing with you today, will move to the next slide. I know slide, actually, I'm not going to use slides, so let's turn the slides off for a moment. Because we want to have a conversation and talk through what are some of the elements to actually implementing the things that John just talked about. It's important that we know the what needs to be, what needs to be done. But more attuned to what I'm working on is the, how do we do it, how do we practically apply?
28:42
And encourage communities to embrace and be empowered to take control of what their public health will be. And so, there are a few elements that I want to walk through with you, And I look forward to the conversation about how do we actually get these solutions really embedded into communities, such that we can see strong climate actions take place, and that there are true equitable solutions that are available to all of us. When we think about the elements of equity, and the elements that we need to apply in order to make climate solutions, really stick in our communities. There are four elements that I want to share with you, and I tried to make this easy so that they're all ease. And we can all remember them, and repeat them, quite frankly, amongst one another. And really share. The first one, is dealing with ethics, in and of itself, ethics, and remembering, and understanding that, come into this place. We have to, in a number of ways, share power.
29:40
And really dig into how we are showing up as public health officials, as government officials, but also the importance of the health impacts that people experience each and every day as a result of climate change.
29:56
I love the title of this series. Climate change is health, because climate change really is a driver to how we are adapting, how we're experiencing and how we're becoming more resilient each and every day. We see it in, though, our public health means, in communities, all around the country. And so, understanding the ethics of showing up, how we show up is an important element to ensuring that we are implementing these factors each and every day in the same way. We have to show up transparently, authentically.
30:28
And understanding the diverse communities, which really have to, that we have to focus on, because they are the first hit, as well as the ones that are recovering quite often from the climate impacts as they are increasing each and every single year. So, it is number one and keeping that at the forefront of how we go into these communities. The second one is experience, and this is so important, it is respecting the lived experience of community members. It's also a place that we see a lot of intersections. And when we are talking about public health climate change and how we go into these communities, there are a few things that came from David's presentation I really want to bring into light with respect to how practically apply things.
31:17
one is the history of communities, and what we have to overcome, in terms of our own experience in these spaces. The presence that local, federal, and state governments have play into how we got here in the first place.
31:33
So, one of the slides that was shared was redlining maps that came as a result of discriminatory redlining practices in the United States. And I'm so excited that that was one of the slides that was used because it respects and understands the intersection of housing, intersection of education, of permitting laws, of pollution, and how they came to be in these communities. And if we ignore that past history, that past lived experience, we take away from people who are living the experience today, what they had to go through, just to get to where they are right now. So, when you go to the doctor, you usually give a Medical History of your family. Your doctor asks you to fill out a form that says, whether or not you have a family history of asthma, health, chronic health diseases. Cancer at ash, if you had any surgeries.
32:27
When you think of lived experience, when it comes to climate change and public health, think of what is that medical history or that experience history from public health perspective, for that particular community. As we're going in and talking about solutions, does that community have a history, a public health history that is disparate and different from other areas because understanding the history makes it so that we are deeply seeding, really the solution, that people, what they need and that they're trying to recover from.
32:59
We have seen through the experience of COVID, that public health impacts and climate change impacts hit communities differently.
33:09
And so, a community that has been on the forefront of climate change, that is a low-income community. Oftentimes, communities of color, oftentimes communities that have been underserved, underutilize are the first ones to not only experienced climate change in terms of being on the front line, but have the least resources. And they had had those historically. So, understanding that lived experience can make a difference in terms of how and when we're able to really implement kind of policy and pollution.
33:42
Kind of policies and regulations that will stick, and that communities can move forward.
33:48
The next place is expectations.
33:51
There's the saying.
33:53
Communities move at the speed of trust.
33:57
The rest of the world tries to move, at the speed of light, environmental movements, speed of light, but communities really move at the speed of trust, and that is so true.
34:06
We all understand, and know that climate change really is an existential crisis that is impacting global populations in ways that we cannot even imagine. And we're living it each and every single day.
34:21
At the same time, when we rush these solutions, it often comes at the sacrifice and the detriment of those who are hardest hit, who are first hit, and are more likely to suffer extraordinary traumatic responses as a result.
34:39
And so, sometimes, moving slower is moving faster.
34:43
And we have to understand and really think through how we're coming into communities, and with expectations are, with respect to our timing and the community's timing of what they want to receive. How they're looking to receive it.
34:59
And, really, how we are deeply interest sets in climate solutions that, again, empower communities, engage them, and that they can carry on.
35:10
The last fourth area, is economics, and I want to spend a little time here, because all too often, we think about environmental justice and climate change in communities of color and those who are hardest hit.
35:25
In terms of victimization.
35:27
People need to, and are recovering from environmental injustices that have plagued our communities for so long.
35:37
But let's think about the opportunity.
35:40
Climate change, green technology, clean energy jobs, is putting us in a position to really transform wealth and health in communities all across the country. And this is a really special moment.
35:55
I spent time. I will. I live in the south-east, but I spend a lot of time in and around communities that are often considered environmental justice, and one thing that I hear more often than. not, is, where's the conversation about what the future is going to be?
36:10
So many people come to communities and say, we want to help reduce pollution.
36:15
We want to help improve the disparate health impacts their experience by these communities, but what are my kids going to do in the next 15 years?
36:25
What kind of jobs can we link to this recovery that also provide a regeneration for these communities?
36:34
Thinking about the innovative ways that through health and climate, we can create not just salaried jobs, that really, truly, I'm sorry, Not just hourly desk, but really, truly sort of salary. Long-term benefits in the health sector that create opportunities, that we're expanding and improving the health and well-being for a community. As well as reducing the disparate health impacts.
37:04
All of these things intersect.
37:07
We cannot have one without the other.
37:09
So, as we are talking about and thinking through an amazing set of policies that we now have an opportunity to implore, we know what to do. How to do it has to come in line with President Biden's administration has put forth an all of government approach.
37:28
They have really been forefront at the forefront of, of talking about environmental justice in a way that we have not really seen. But the all of government approach cannot exist by itself.
37:42
There has to be an all of community approach, which includes local leaders, public health care leaders, academia, philanthropy, faith-based community. There has to be an all of community approach that helps the policy development to be implemented and really embrace and carry forward, so that we're building one upon the other and really getting to efficient climate change solutions that are helpful and helpful for us all.
38:14
That's why climate changing health is such an impactful way to say that we have this opportunity right now to dig into the how and accompanying it with the what we need to do.
38:28
Let's go back to those again, and I look forward to the conversation.
38:33
Thinking through the ethics, making sure that we're coming into communities, in a way that is respectful. That understands the importance of sharing this power, where we've had in some spaces, majority power that really needs to be shared with community, so that they can implement the policy in the way that they know best in their own communities. The experience lived experience and intersections of public health, education, climate, change, violence, the number of different ways that there are health indicators as well as opportunities to understand the intersections and the experience of the Command Z such that they can really implore climate solutions.
39:14
The expectations, which is the timing, and how communities move at a speed of trust, ethics helps us build that, build that trust, but we have to move in a way that sometimes slower, means faster, but it gets us there at the end point.
39:28
And then finally, the economics: ensuring that we're not just talking to communities about how to improve their health.
39:35
Because that mother who has three kids and two of them had asthma, she still has to go to work. She has still had to put food on the table, and heart timing might be different than ours. When we talk about what emissions are and how they're impacting her family, we have to think through the timing and make sure that it's suitable and achievable for all of us and those economics.
39:57
That is critical. Those are the opportunities that are wide open for all of us to jump into by putting the policy together with how we do it and how we enter these spaces. Will go to the last next slide. This is my information, contact information. I'm really looking forward to digging into this and getting some really good questions about the, how the practical nature of putting these into place is one of the things that I'm excited about us doing at the Environmental Defense Fund. I'm a former mayor. I come from the Federal Government so this is a happy space for me to see us actually implementing these climate policies that have taken so long for us to really be in a position to implore. I look forward to the conversation.
40:44
Thank you so much, Heather. Next. We will hear from Dr. Lindsay Butler, an environmental epidemiologist science, communicator, and thought leader specializing in the intersection of climate change and human health. She serves as the Director of Climate and Health Resilience at Blue Cross Blue Shield of Massachusetts, and we're so pleased she's with us today, Lindsay
41:07
Thank you so much, Kathryn. Thanks for having us today, And thanks so much to Dr.Balbus and Heather for what they've shared. I'm going to talk a little bit about how we are trying to address some of the challenges and opportunities that have been shared so far and really look beyond corporate sustainability at how we as a health insurer are combating climate change in trying to advance health equity.
41:34
Next slide, please.
41:36
So, we're really trying to take an integrated approach. We've heard about how the Biden Administration is taking an All of Government approach at Bluegrass. We really want to take an olive organization approach to our environmental stewardship. So, really trying to prevent sustainability from being sort of siloed thing that exists in one part of our company, but really integrating environmental sustainability and climate and health resilience to the ethos of our organization across everything we do. And we see that as sort of having three elements. You know, this is an evolving strategy as we try to stand up to the climate and health crises that we're seeing. But right now, we sort of see three key components to the work.
42:20
one is our own responsibility, recognizing that this isn't about personal and individual blame and shame, like many fossils fuel. Contributors have tried to get us to believe. But it's really about organizational and institutional change to address the climate crisis. So, first, recognizing our own environmental footprint, our own environmental responsibility, and having our own ducks in a row. And like Dr. Balbus said, walking the walk.
42:48
The second is the work that we do to advance environmental justice, and our health equity work through our corporate citizenship team. And the third is our role as a trusted communicator. Heather talked about the importance of moving a community at the speed of trust. And we recognize that the Crossing Shield Blue Cross as an organization is a trusted communicator of health information. So, we want to step up and we want to share information about the intersection of climate and health and how addressing the climate crisis is going to lead to healthier environments and healthier individuals. Next slide, please.
43:29
Next slide.
43:32
So, just to highlight our work in our corporate sustainability and really sort of getting our own ducks in a row, on the one side, you'll see that we have made significant progress in reducing our environmental footprint at Blue Cross. Since 2010, we've reduced our electricity usage by almost 60%. We've made significant waste reductions. We're very intentional about the packaging and products that we allow into our buildings. We've reduced our use of paper. We've really become paper free across the majority of our organization. So, we've made progress. We have robust corporate sustainability program, but now we need to take that further. We're working on improving our greenhouse gas accounting practices to better account for our Scope three emissions, which, as we know, are difficult to account for, but could represent a large piece of our missions.
44:24
And especially with many of our employees working at home, how does that impact our environmental footprint As an organization? We're working towards carbon neutrality and zero waste. We're also trying to develop a best in class, environmental responsible procurement program. We've been a leader in supplier diversity for a long time, and we want to get our environmental sourcing up to that same standard. So, you know, when we think about individual consumer power, right, we've seen that individual consumer power is key to advancing. Environmental actions, like we saw with BPA when it sort of came out of market, based on the call of the consumer, organizations also have a lot of power with how they use their dollars and they're spending. So, when we procure goods, when we procure services, when we enter into business partnerships, Blue Cross expects those partners to be doing the best that they can for the environment as well and we want to use that power that spending power to really catalyze change.
45:26
The last part of this is helping our associates and employees bring Sustainability home where all adapting to this new remote work environment and many people will stay working from home. So how do we take the practices we've developed for inside our buildings and bring those home to us to our employees at home. So, they're working in healthier environments that they're composting at home and we're incentivizing them in educating them to do so. Next slide please.
45:55
We've also expanded our sustainable development goals so previously we've reported on zero hunger, good health and well-being and responsible consumption and production.
46:06
Next slide please. Moving forward, we are going to go after three more sustainable development goals, including sustainable cities and communities, climate action, and reducing inequalities. So, we are expanding our reporting and expanding the way we approach our UN Sustainable Development Goals.
46:27
Next slide.
46:30
The next thing I want to talk about is the work we're doing to advance environmental justice, which is a pillar of our health justice strategy, which is our approach to corporate citizenship at Blue Cross. Next slide.
46:41
Sorry, trying to whizz through so that we have time for conversation. This slide just highlights what our corporate citizenship strategy is and the work that we're doing in communities did in Massachusetts to help people lead a healthier life with more equitable access to environments, experiences, and education needed for good health. We see that as that work sort of falls into three categories for us. That's our work to advance food justice, Environmental Justice, and Racial Justice. And EJ is obviously a really important part of the work that we're doing for climate and Health Equity. Next slide.
47:20
Here, I just highlight two of the partners that we work with, to advance our EJ work, you know, really when you when you do this work, it's so important to really let the community lead the way. They know what the burden of pollution is and they know the work that needs to be done. So, we partner with to organizations, these are just two examples. Green Roots and ... Farms, who both the terrific work in the Chelsea in East Boston area of Massachusetts, which has a really, really difficult burden of air pollution, noise, pollution. There are some manufacturing operations on the Chelsea River and we support these organizations with our grant making, their financial support, their in kind support, and through providing volunteers through our employee volunteering programs.
48:12
Next slide.
48:15
Next, I want to talk about sort of that trusted communicator component of this work. So, step three, in our work to advance climate and health resilience, is to communicate, to educate, and to empower. And I just want to, I want to recognize here that, I think what, what has been one critical flaw of the environmental movement, or environmental support for climate action. Whatever you want to sort of talk about, our need to galvanize around this work, is, I think, oftentimes, environmentalists', public health officials.
48:48
We assume that those members of the community that we want to work with, we want to get folks to change their behaviors to prioritize these things. We assume that they understand, and so, what we're doing is we're asking people to change without really telling them the why exactly. So, we really see communicating, educating, and empowering people about the intersection of climate and health to be a really key part of this work that we can contribute to.
49:15
Next slide.
49:18
So, I just want to highlight that there's a huge appetite. According to the Yale program on Climate Change communication, when asked if folks are interested in more information about climate change, and wanting to see more reports in the news on climate change, a nationally representative sample from the US, 74% of people said they were interested in hearing more.
49:40
Next slide.
49:42
And just 78% of people said they wanted to hear more about the impacts of global warming in their local community. And as doctor Barbara said, many of the health impacts of climate change are highly localized. So, it's interesting to know that 78% of people want to know more about that.
49:59
Next slide.
50:02
Here's an example of some of the ways that climate is impacting health that we think that our members, our providers, our associates should know about and and maybe haven't had the opportunity to be exposed to this information. So, for example, recent research on the heat the health impacts of heat stress on children have found that in extreme heat there is an increase in ear infections in ER utilization for heat related illnesses in gastroenteritis and other adverse outcomes in children. We know there's a robust literature that heat stress is leading to higher rates of pre-term birth, low birth weight and stillbirth in the United States. And we know that there's many ways that climate change impacts air quality and this just might not be information that people have been privy to and as a health communicator, we want to help people learn about those things in a very accessible and easy way.
50:59
Next slide.
51:02
Dr. Balbus talks about the threat to our health infrastructure. Now, we have a lot of providers we work with. We have a robust network. Are they all aware of the ways in which climate change is a threat to our health care infrastructure? And what is our role in helping them to understand.
51:18
Next slide.
51:21
So, how do we do that work to communicate and empower? We want to provide opportunities for our associates to learn about climate and environmental issues. We want to educate people about the ways in which the environment and health are connected and really making it clear that the climate crisis is a health crisis.
51:39
We want to support and incentivize action among our providers among our members, among the communities we serve. And we want to work in partnership with municipal leaders and lawmakers to advance healthier environments for healthier people in the communities that we serve. At Blue Cross, about 80% of the municipalities in Massachusetts get some fluid blue cross coverage from us, and some of them have robust climate action plans, and are really ambitious, And some of them really haven't thought about their emissions or their climate change adaptation at all, so how can we support those varying degrees of climate planning in our municipalities?
52:22
Next slide.
52:24
I'm just going to jump through here, and then interest of time. Next slide.
52:30
Next slide.
52:32
Next slide.
52:34
I just want to close with this one quote from John Holdren, who was the climate Advisor to President Obama and said this back in 2007, we basically have three choices mitigation as we know, that's reducing our emissions, adaptation, like increasing a wall to prevent from sea level rise and suffering. We're going to do some of each. The question is what is the mix going to be?
53:02
The more mitigation we do, the less adaptation will be required and the less suffering there will be.
53:08
Next slide.
53:11
I'm happy to talk more about this with any health care organizations, any other insurers. I think, you know, it's very clear that we have an imperative as health organizations to really act on these issues. You can always contact me via e-mail or on Twitter at Dr. Lindsay Butler.
53:33
Thank you, Lindsey, I'll ask all of our panelists to join us back on camera for our Q&A session.
53:42
I'm going to start with a question for the full panel by offering to Heather. First, can you share any thoughts on boosting Brazilians specifically and rural health systems, which face that dual challenges of treating higher risk populations as well as financial challenges?
54:03
Yes, thanks, Kathryn. I love this because it gives us an opportunity to leverage, leverage, leverage.
54:08
Right now, the Biden Administration has been successful in passing by partisan infrastructure funding, so that means communities all around the country, particularly, communities that are eligible for rural development dollars, will have funding to help faith through very creative way. So rural health associations, hospitals, should partner with their local municipal leaders, county leaders, to see how they can leverage infrastructure dollars to improve the infrastructure of those hospital systems around those hospital systems. And also partner with businesses in the area. There are a couple of great examples of that. South Carolina Reaches Regenesis project is one, like in on a couple others. But there are a lot of them that there. I think that's a great place to start.
55:00
If I could just add, Kathryn, one thing that we saw, Texas with some of the really severe storms, was that on community health centers with solar, actually were still able to provide health care throughout the storms. When some others had total collapse of their grid and infrastructure on Harvard is doing some excellent work around The Resilience of healthcare infrastructure, Harvard Sea Change. So I'd recommend taking a look at some of the work they're doing.
55:31
Great. Thank you.
55:34
We had a few questions come in about clinical education. And, we found there is a gap and clinical education of medical professionals, of the actual health impacts of climate change, especially as it relates to air pollution, and how to express that to patients, as well as the fact that US physicians have a lack of familiarity with the Northern migration of Tropical Diseases and their health effects. And not for John, or for any of the panelists, but, John, you could start. Or is there any part of clinical education that's a part of what you're working on? And as any other work that you could share with our, with our audience?
56:15
Sure.
56:16
It is an important point.
56:18
You know, one of the things that I've felt, you know, having worked on education in academic centers.
56:25
Speaking with health professionals about climate change and health for over 25 years, is, people need to know what they can do, and they need to know why they need to know physicians, and healthcare, and nurses, and healthcare professionals, more so than anybody else, because the, you know, the curriculum is jammed, the educational needs are huge.
56:46
So, you know, just my first answer, that question is yes. I mean, there's a lot of stuff going on and we're supporting it, and we will support it.
56:54
You know, I think that that the undergraduate years for most of the health professions are the best time starting early, I think that kind of the beginning and the end.
57:02
So, you know, when you have a little more space in the curriculum at the beginning, and then also in the continuing education, I think there's a lot can be done in terms of maintenance of practice, projects going on in clinical spaces that relate to sustainability and resilience.
57:16
That can, a, the growth of awareness and understanding of professions.
57:21
But, um, you know, I think the more that we can tie this to clinical practice and what people are actually doing, so that it's there as an advocacy role, but I think there has to be also this pragmatic, you know, Why do I need to know this in order to make it'll be more effective and have higher quality delivery of care.
57:39
But where I'm heading in this, ramble is a hum, you know, I think when we are at the point where health systems to get an alignment with the climate agenda, When health systems, when the people who are managing the floors, have to be thinking about where their energy is coming from. Where their food is coming from, with food waste is going.
58:00
When that becomes part of the DNA of the health system, That's when there will be transformative interest and understanding and educational opportunities. Because people are going to have to learn how to do that.
58:13
And in so doing, that will open up that space.
58:20
Lindsey or Heather?
58:21
Anything?
58:23
To add aggregate, it gives us an opportunity to really, again, get to that economic piece, as well as find those spaces, where communities really want to see a forward. Focus on how they can engage in opportunities that provide education. That provides span and scope for how climate solutions are really going to be implored. And so, it really is a great space to dig into a bit deeper on, on those opportunities.
58:54
I'll just echo what doctor Barbara said about maybe the place for it is in the undergraduate education, and I would argue that that's the case for no matter what an undergraduate studying these days. No one should be leaving their undergraduate education. Without some knowledge of global warming and the way it impacts systems. And the way it impacts human health, so I just wanted to echo that.
59:21
Have time for one more question. We thank our audience for all the great questions, and we will be sharing them with the speakers. What do you think would be a starting point for our local organization that's just beginning to focus on how we can address climate change as a social determinant of health? And in terms of just one example of local health organizations, there are a few questions about how bank community health centers or clinics, who are on the front lines and communities right now.
59:57
I'll say, real quickly, don't recreate the wheel, as Dr.Butler was provided a wealth of information. And current existing research as well as policy that is underway that you should spend some time really reviewing, digging into and seeing what's there that exists already, and how that overlaps what's happening in your current community. So, doing a bit of listening within the community, but also taking advantage of these resources is a great first step.
1:00:27
I think, you know, also in line with the education question, I think one of the other made inroads for the change that we're looking to create, and the health improvements we're looking for is and how the energy both touched on this is the social determinants of health.
1:00:41
There are seven categories of social determinants of health and only five categories of zip codes right now.
1:00:47
Natural and built environment are systematically not part of it.
1:00:50
But when we put all seven together, then we have that local solution space, we can codify, not just the education or the transportation, the food security, domestic violence, homelessness, but also the quality of people's housing.
1:01:04
The quality of, you know, the green space and the natural environments that are.
1:01:09
So, I think it's just building so, so important, both to climate resilience, but also just mental health and well-being.
1:01:17
When we have that incorporated into how care is delivered and how upstream drivers are now are integrated into local health care.
1:01:27
I think that's going to be very powerful to Heather's point, tapping into the resources that can give you that information.
1:01:35
Oh, I just wanted to say, my initial thoughts are just, on the acute side, I would say, just awareness of heat stress, awareness of heat stress when you are treating elderly patients, when you're cheating, children, when you're treating a pregnant woman, just awareness of that danger. And communicating that danger to patients. And then, on the longer term side, I would say, you really can't reduce your emissions without knowing where they come from. So, trying to do the best you can at accounting for your personal emissions or emissions as an organization.
1:02:09
Well, unfortunately, we are out of time. I want to thank our excellent panelists speakers for being with us, and sharing your valuable insights and perspectives. We will be sharing a recording of the event and our slides, and thank you to our audience for joining in the Discussion. Your feedback is important to us. Please take a moment to complete a brief survey that will open on your screen, after this event. And you can also find our recent infographic on Climate change and health on our website, and we look forward to continued conversations on this issue and the months and years ahead. So, thank you all, for joining us today.
Presentations

John M. Balbus, MD, MPH
Office of Climate Change and Health Equity at HHS

Heather McTeer Toney, JD
Environmental Defense Fund

Lindsey Butler, PhD, MSc
Blue Cross Blue Shield of Massachusetts
More Related Content
See More on: Health Equity | Environmental Health | Social Determinants of Health