Webinar
Investing in Children’s Health and Well-being
Time & Location
In addition to its physical toll, the COVID-19 pandemic has had a devastating effect on the emotional and psychological well-being of children and young adults across the country. The pandemic has exposed the need to address the rising rates of anxiety, depression, and suicide among young people. Care providers fear that the pandemic, and the lack of action to address issues related to it, could have a long term negative impact on young people, especially LGBTQ, black, and brown youth.
This webinar brought together experts to discuss the opportunities and strategies to help care for children and young adults' mental and physical health after a year of unprecedented challenges. Speakers discussed:
The COVID-19 pandemic’s effect on the mental, emotional, and behavioral health problems of children and adolescents in the United States and efforts to promote children’s well-being
An organization's efforts to prevent suicide among LGBTQ youth by providing free resources, support centers, and access to 24/7 crisis services
A health plan foundation’s commitment to partnerships to strengthen and protect children’s mental health throughout the community
Kathryn Santoro (00:00:00):
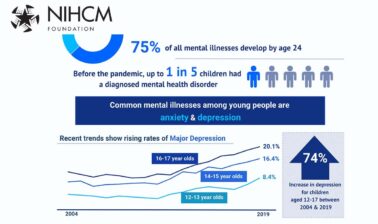
Thank you. I'm Kathryn Santoro, director of programming at the National Institute for Healthcare Management Foundation. On behalf of NIHCM, thank you for joining us today for this important discussion, Investing in Children's Health and Well-being. Prior to the pandemic, up to one in five children had a diagnosed mental health disorder and recent data is beginning to illustrate the impact of the pandemic on children's mental health.
Kathryn Santoro (00:00:29):
In a recent survey, more than 20% of parents with children ages 5 to 12 reported their children experienced worsened mental or emotional health during the pandemic. Disparities in access to care existed prior to the pandemic, particularly for children of color and LGBTQ youth, and these inequities have only been amplified by the disproportionate impact of the pandemic on these children. The pandemic created a perfect storm of stressors that may also increase the risk of children having adverse childhood experiences such as living in poverty, experiencing violence, or being exposed to adult substance misuse, which can lead to long-term mental health and substance use issues.
Kathryn Santoro (00:01:21):
Children's mental health is intertwined with our physical health and overall wellbeing. Today we will hear from a prestigious panel of experts to explore strategies and solutions to invest in children and young adults' mental and physical health after a year of unprecedented challenges. Before we hear from them, I want to thank NIHCM's president and CEO, Nancy Chockley and the NIHCM team who helped to convene today's event. You can find full biographies for our speakers along with today's agenda and copies of their slides on our website.
Kathryn Santoro (00:01:59):
We also invite you to join the conversation on Twitter using the hashtag children's wellbeing. I am now pleased to introduce our first speaker, Dr. Kelly Kelleher. Dr. Kelleher is distinguished professor of pediatrics and public health and ADS Chlapaty endowed chair for innovation and pediatric practice in the colleges of medicine and public health at the Ohio State University. He is also a vice president of community health at Nationwide Children's Hospital in Columbus, Ohio.
Kathryn Santoro (00:02:38):
He is a pediatrician and health services researcher focused on improving and measuring the quality of pediatric care for high risk children affected by social determinants of health, violence, neglect, alcohol, drug use, or mental disorders. We are so honored to have him with us today to share his perspective on strategies, policies, and investments to improve child health and wellbeing. Dr. Kelleher?
Kelly Kelleher (00:03:08):
Thanks, Kathryn, and pleasure to talk today, and especially about something that we should all care passionately about, and that's investing in child health and wellbeing. But before we get into the actual investment strategies, I think we have to talk a little bit more about COVID and children and when surviving is not surviving well. And as my colleague, Dr. Hoagwood said that children are going to be the longest surviving victims of the COVID pandemic because the pandemic has dramatically altered, not so much their health and wellbeing from direct infection, but the likelihood that they will grow up in any economy in poverty.
Kelly Kelleher (00:03:50):
And so children are already our most poor age group. They are the group most likely to be poor in the United States, and they're most likely to become poor during this COVID pandemic. We noted that after the 2008 recession and after the recession in early 1980s, children were the most adversely affected, and for the longest period remained the most poor during those times. So children will suffer most of the economic consequences we see. And what does that mean for them?
Kelly Kelleher (00:04:24):
Well, unfortunately this is before the pandemic, the number of behavioral health patients seen in the Nationwide Children's Hospital emergency room, and this data has been mirrored nationwide, we have reports on that and we could share, but in the years preceding the pandemic, we had a 500% increase in emergency room visits for behavioral health. And if we look at suicide attempts in even more current data, the rate of death by suicide in the US, the blue line here, is continuing to go up for children aged 5 to 19 and has risen even more during the last year.
Kelly Kelleher (00:05:11):
If we look at the most recent data from the CDC, and this is the hardest to see, and I'm not spending a lot of time on all the effects of COVID, I'm focusing on suicide and mental health and crisis, but it's a marker for severe disability and concern. And you'll see in the top graph, females, the rate of ED visits for females in our current year, the top line is spiking. And in boys it's rising, but among girls it's spiking much higher than it's ever been. And we are feeling that in our local emergency room, in our local psychiatric beds and in the number of children coming referred from schools for anxiety.
Kelly Kelleher (00:05:54):
So we should expect that COVID is going to have long-term effects and certainly if nothing else, the loss of class attendance in our schools. So children are not surviving well through this pandemic. Of course, we can talk about the racism involved and the fact that brown and black children suffered disproportionately through all this, but the take home message on the COVID pandemic is that the economic effects are going to dwarf the immediate health effects.
Kelly Kelleher (00:06:23):
Poverty and unemployment will go up. We know that homelessness and family violence go up after every recession, and this one is very deep, that educational disruption will cost potentially a whole generation, a cohort of children, several measures of literacy and graduation rates and low immunization rates for things like measles. Many children missed their routine shots and we are anticipating and the CDC has warned about measles epidemics and other common communicable diseases, an increase in drug use, mental health and trauma related conditions.
Kelly Kelleher (00:07:01):
At the same time that's all happening to children, tax revenues have plummeted in many cities and counties and states and not-for-profit organizations have gone bankrupt during the pandemic. So many child serving agencies who are already vulnerable are closed. I hope I've depressed everyone and said all the negative things that we can, we could spend more time on that, but we really want to turn to solutions because we understand a lot better about what causes problems and how to invest better now.
Kelly Kelleher (00:07:32):
So what are the solutions that we can think about? And I want to describe our investing in child health and wellbeing in three forms. First, we have to build health, second, we have to build family wealth and third, we have to build community wealth. These are communities that have chronically been disinvested in and do not have access to resources that can be retained. So we have intergenerational poverty that is forced upon families by disinvestment practices and the only way to correct that is to reinvest.
Kelly Kelleher (00:08:04):
So investing in health, family wealth and community wealth, and I'll cover those first by a slide and in the interest of time to make sure we have time to talk about all these, I'm not going to spend a lot of time on this, but our family centered model really focuses on bringing new resources into the environment and altering the structures that families engage with to lead the best outcome. And we have partners in the city of Columbus, Community Development for All People, the faith-based organization, and United Way that help us intervene in affordable housing, health and wellness, community enrichment, education, and economic development simultaneously in a place-based approach, and I'm going to talk about some of those right now.
Kelly Kelleher (00:08:52):
But again, how do we first invest in the health side? Investing in child health doesn't necessarily mean investing in the traditional healthcare system. In fact, it means breaking the fourth wall of the practice. We know the healthcare system was broken before the pandemic and the pandemic emphasized that we are not reaching our most vulnerable families. So we have to break the fourth wall of practice and engage in radical approaches.
Kelly Kelleher (00:09:20):
And they include going to where families are: school-based forms of care, mobile clinics, texting services for medicine and information, home visiting programs, delivery of medicines to schools and families in the home and finding innovative partners like doulas and other faith-based and community partners who are more engaged on a day-to-day basis with people who are afraid to engage with our system. For example, we know that 45% of adolescents in the United States do not get well care every year and about 25% have no contact with the healthcare system. We have to break through those kinds of numbers.
Kelly Kelleher (00:10:01):
We learned that telehealth and digital care work sudden rise from 1% tele-health to 40% overnight practically during the pandemic, showed us that it can be done and it turns out that our no-show rate, our absentee rate goes down. People are unable to make tele-health visits and we have to find ways to help families do that when they choose. But most importantly, we go from an our patients only to an all children model, a true population health model.
Kelly Kelleher (00:10:33):
And in fact, our hospital has set goals for the county to achieve health outcomes for all children in the county, not just our patients. And I think that's the model that we have to move towards, is thinking about all children, not just as those that show up. Related to that is the fact that Columbus has becoming an all care for children, a child center community. It's not the hospital's business to take care of all children, it is the entire community's business.
Kelly Kelleher (00:11:04):
And so that means coaches, teachers, principals, partners in not-for-profit agencies, employers, everyone has to understand that their actions matter and their actions matter in the wellbeing of children. So all children and all care for children are two important principles. Those investments though in health aren't enough if we don't also invest in family wealth. Family financial health is as important as medical care and maybe more important in long-term health outcomes for children and adulthood.
Kelly Kelleher (00:11:37):
And the National Academy of Medicine has put four reports out last year that all focused on improving child outcomes, and every one of them highlighted the central role of reducing child poverty, and one of them had a plan to do so. And we've implemented many of those investments in building family wealth in our health system. And so to do that, I'm waiting for the magic slide here, to do that, this is a picture from our tax clinics, our website where tax help for central Ohio families, we implement in our clinics, tax clinics where we do free tax preparation by volunteers for earned income tax and childcare and now meet child tax credits.
Kelly Kelleher (00:12:19):
We provide utility supports, we're beginning of program to emphasize SSI enrollment for children with qualifying disabilities, Medicaid enrollment and financial literacy. If our families can't get access to the resources they need, then they're not going to be healthy no matter what we say in the office. So we are trying to implement all these resources to families to get money directly to them. And then inside our health system, it's critical that we also think about implementing what we need to do to help families benefit from improvements in well-being and income.
Kelly Kelleher (00:12:57):
So we have a neighborhood hiring training and promotion effort in partnership with Goodwill and our faith-based partner that actually has hired 1200 people over the past five years. Our new local purchasing efforts are now focused on making sure vendors are local wherever possible and we invest in the communities that are most needy. We have a livable wage policy now and we are gradually moving towards requiring all our vendors to have a livable wage policy as well because the current federal minimum wage policies are unacceptable.
Kelly Kelleher (00:13:34):
So if we want to invest in building family wealth and make a difference to improve the health of the children, we have to make sure families have the resources to keep their kids healthy. And finally, we talk about investing in community wealth. And community wealth means that communities can take care of each other and help other families that when they're in need. And there are two main classes of doing this, one is shared equity, shared ownership. And how do we do that?
Kelly Kelleher (00:14:06):
We are working on affordable housing construction on a community land trust in partnership with the city and county. We have set up joint ventures for affordable housing with the local CDFI called Ohio Capital Corporation and community development corporation, that's sponsored out of one of the churches locally and working on a second one now. And these affordable housing ventures among our various partners have topped a hundred million dollars recently on south side and Linden areas in Columbus, Ohio.
Kelly Kelleher (00:14:39):
We are exploring credit union investment because credit unions invest much more locally and at a lot more small loans and we think that's a useful tool for developing shared equity in the community. And then helping people build home ownership, home ownership requires subsidies to build in poor communities and help people get there. And it can be done on land trust properties at a lower cost, but it really requires partnership with philanthropy to understand that we really need to transfer more and more home ownership into communities.
Kelly Kelleher (00:15:15):
Finally, community ownership things, actually setting up a community development corporation and joint ownership with the hospital, setting up ownership of a bike cooperative in south side and working on one in Linden right now, two of the neighborhoods in our area that have been affected by red lining and racism and blight for a long time. And finally, a fresh produce collaborative developing to handout and produce and allow people to shop for fresh produce and more than 400 people a day coming through our produce collaborative.
Kelly Kelleher (00:15:48):
For more ideas about building community wealth, I really recommend people read the Democracy Collaborative material because they have some of the best primers on that. So we know that investing in child health and wellbeing in United States, we have a history of poor stewardship of children. We have a history of redlining and racism for many children, and this is a Columbus Ohio map of some of the red lined neighborhoods for 80 years that resulted in neighborhoods that profoundly concentrated our black population and also concentrated our infant mortality and gun violence and race and suicide attempts.
Kelly Kelleher (00:16:28):
And so now we've also had a history of child under investment in our democracy, which is a side effect of the fact that kids don't vote. And those are worsened by COVID and especially poverty, but we have solutions. And this is a picture of my grandson, Oliver who watches every move I make at home every day pretty closely and he's observing whether we're really living true to our values for children that we talk about all the time.
Kelly Kelleher (00:16:55):
So our investment should focus on a child health system that includes all children, all doors open and all care for children. And we've built family wealth through entitlements, credits, resources, income and literacy and then we built community wealth through shared equity and community ownership. I believe these are the only ways we're going to really make a difference and prevent the long-term harmful effects of the increased poverty from COVID.
Kathryn Santoro (00:17:24):
Thank you, Dr. Kelleher for sharing your great work and how collaboration to address the social determinants of health can lead to positive outcomes for children and families. Next, we will hear from Dr. Amy Green, the vice president of research at The Trevor Project. Dr. Green is a licensed clinical psychologist. At Trevor Project, her team supports the organization's life saving work by using data and research findings to advance its crisis services and peer support program, as well as advocacy and education initiatives. Under Dr. Green's leadership, the research team produces innovative research that brings new clinical implications to the field of suicidology and LGBTQ mental health. We're so grateful she is with us today to share her team's research. Dr. Green?
Amy Green (00:18:23):
Hi everyone. Thank you so much for having me and thank you, Dr. Kelleher for such a powerful presentation. I think that we'll see some of the similar themes show up in this work as well. But I am Amy Green, I use she, her pronouns and I am the vice president of research at The Trevor Project and I'm going to talk a little bit today about LGBTQ youth suicide risk during COVID-19. So for anyone who hasn't heard of The Trevor Project before, we are the world's largest suicide prevention and crisis intervention organization for lesbian, gay, bisexual, transgender, queer and questioning young people.
Amy Green (00:19:07):
And those who are familiar are probably most aware of our crisis services platforms and that includes Trevor Lifeline, TrevorText, and TrevorChat which allow you to reach out to us using 24/7 phone, texting and web chat. We also have a safe space online social networking platform for LGBTQ that's called TrevorSpace, and it allows LGBTQ youth around the globe to connect with one another and find support. This type of virtual network becomes even more relevant during times like the COVID-19 pandemic.
Amy Green (00:19:39):
Throughout the pandemic, we at Trevor have used the phrase physical distancing rather than social distancing because we know that our youth have multiple ways in which they form social connections. And TrevorSpace provides a way for LGBTQ youth to maintain support and acceptance, even if they're physically isolated from people and places that affirm them in their identity, and we'll talk a little bit more about that in a little bit right now. So to support our mission of ending LGBTQ youth suicide, we also have an education department that provides education and skills to others to best support LGBTQ youth and prevent suicide.
Amy Green (00:20:15):
We have an advocacy department that works to support LGBTQ inclusive policies and to stop practices that may harm LGBTQ. And then of course, we have the research department which is where I sit. Well, one of the reasons The Trevor Project exists is because LGBTQ youth are at significantly increased risk for suicide compared to their peers. And in fact, data consistently shows that LGBTQ youth are four times more likely to attempt suicide each year compared to youth who aren't LGBTQ.
Amy Green (00:20:49):
There's the minority stress model, it's used as a primary framework to understand how LGBTQ youth disparities and suicide risk relate to the experiences they're having in the larger world about discrimination, rejection and victimization, which then result in shame and stigma. And we know that there's nothing about being LGBTQ that places youth at greater risk for mental health challenges or suicide, but it's the way that they are treated and the experiences that they have.
Amy Green (00:21:21):
And we also know that this minority stress can be most persistent and impactful for those who have multiple marginalized identities. In our research, that's most often LGBTQ youth of color and LGBTQ youth who are transgender or non-binary. And so given the increased risk of suicide and mental health challenges that we already know historically have existed among LGBTQ youth, when we started last year hearing about that there may be a longer pandemic, even though the initial data was showing that youth were less likely to be impacted in terms of their physical health from the COVID-19 pandemic, we immediately became concerned for the wellbeing of LGBTQ youth during the pandemic.
Amy Green (00:22:07):
And so in March of 2020, just as the pandemic was beginning to really take hold in the US, our research team created a report that's one that you can see here, detailing what we expected based on what we knew so far about LGBTQ youth and about suicide during major disasters and pandemics, what we expected to be the major concerns.
Amy Green (00:22:29):
And the three areas that we really looked at at that time were: health physical distancing from others and being isolated in places where youth may not have any support for their LGBTQ identity might impact them, ways that the economic strain, poverty and jobless might disproportionately impact LGBTQ young people who we know are already more likely to experience poverty, underemployment, housing instability, and ways that the existing high levels of anxiety and depression that LGBTQ youth had historically before the pandemic might place them at greater risk for the definite stressors that were going to happen during this year.
Amy Green (00:23:08):
And then as far back as February 2020, so if we think back to that time and how much was unknown, The Trevor Project began preparing for ways we might need to shift our service model to meet the needs of LGBTQ youth during a pandemic. Previous to that, all of our Lifeline calls took place in our call centers in New York and Los Angeles. And thanks to our amazing technology team, they worked around the clock to ensure that we could continue to offer services 24/7 to youth while going fully remote for the first time in the organization's over 20 year history.
Amy Green (00:23:42):
And so because of that effort, so we were able to continue even as there were surges in our volume was youth experiencing changes like they've never before had with the closure of schools and lots of connections, we were able to be there. We also were able to collect a large amount of data from LGBTQ youth over the course of the pandemic. So each year our research team conducts a large national survey of LGBTQ youth. You can see there that nearly 35,000 LGBTQ youth from across the US took part in our 2021 survey, and these are youth ages 13 to 24.
Amy Green (00:24:20):
This year, our data collection occurred in October to December 2020, so sort of right in the middle of the pandemic, which gives us unique insights into how LGBT youth were actually fairing during the pandemic. And our sample this year was incredibly diverse so we had 45% of our sample identifying as LGBTQ youth of color, and more than one in three identifying as transgender and non-binary, which gives us the ability to look at our findings, not just in aggregate, but more inter sectionally to understand the experiences of marginalized subgroups within the LGBTQ community.
Amy Green (00:24:55):
And so next, I'm going to review a couple of our main findings. Since we only have a short amount of time, I would encourage anyone interested in learning more about the survey to go to our website, thetrevorproject.org and there you'll find the full report both in PDF and a Microsoft format to look through. I also want to say that before I review this data, I always like to give folks a warning that their rates for suicide and mental health concerns among LGBT youth are quite high and can be difficult to hear and I also want folks to know that this is a general population sample rather than Trevor's crisis service users.
Amy Green (00:25:29):
Sometimes when I review this data, people think, "Oh, that must be the rates that they have for youth who are already in crisis who are using Trevor project services." But in fact, we don't do any recruitment through our own services. So these numbers are actually what's happening in the broader population of LGBTQ youth this year. In terms of the overall sample, so across all youth, 42% of LGBTQ youth reported seriously considering suicide in the past 12 months, with 14% reporting that they attempted suicide in the past year.
Amy Green (00:26:06):
And consistent with what we already know about suicide risk in general, those who are younger, so those are LGBTQ youth ages 13 to 17, this was school age youth compared to those who are 18 to 24, had the highest risk of considering and attempting suicide in the past year as did those who are transgender and non-binary where you can see over half of trans and non-binary youth seriously considered attempting suicide in the past 12 months.
Amy Green (00:26:31):
We look back at our previous survey, so this is our third year conducting this survey, the rates of considering and attempting suicide remain relatively comparable across the years. But I'd like to draw your attention to the right side of the graph where we see significant disparities for LGBTQ youth of color. Now, in some of the preliminary national death data that's come out from the CDC released for the year 2020, there was actually a slight decrease in suicide deaths overall compared to previous years.
Amy Green (00:27:01):
But the data wasn't segmented so it wasn't examined in terms of gender and race ethnicity, and age. And in fact, in some state level analyses that have occurred, they've shown reductions in their state were among white individuals, and that they actually had increases in suicide deaths among people of color. And in our data, when we look at LGBTQ youth of color, we appear to see growing rates of suicide risks compared to LGBTQ youth where you can see there that 12% of white LGBTQ youth reported that they attempted suicide in the past year compared to 21% among black youth, 31% among native indigenous youth, 18% among Latinx youth, 21% among those who had multiple race ethnicities.
Amy Green (00:27:46):
And so this is a very concerning trend that is something that historically hasn't been attended to in much of the field of suicide in general. There is now increasing attention particularly to the rising rates among black youth in terms of suicide side risk. But I encourage everyone when you hear data and information about mental health and suicide risk over the pandemic, when you hear aggregate numbers to think about the ways that that may not represent all individuals the same.
Amy Green (00:28:18):
Similar to some of the data that Dr. Kelleher presented that's come out recently, we've seen increases in just a recent report from the CDC emergency room visits for suicide attempts, that those numbers for girls have been much higher than the numbers for boys. When we look at aggregate, that number looks much smaller than it is actually when you separate it out. And so it really highlights the importance of looking at the impacts of the pandemic among subgroups looking inter sectionally and not just taking a one size fits all approach to what's happened in this country.
Amy Green (00:28:55):
Next, I'm going to talk a little bit about anxiety and depression. So in the past year of our survey, 72% of LGBTQ reported symptoms of anxiety or a generalized anxiety disorder, and that was using a brief standardized anxiety screening tool with 62% reporting symptoms of a depressive disorder using a brief depression screening tool. For comparison, last year when we asked these same questions and used the same screening tools, 55% of LGBTQ youth reported depressing symptoms.
Amy Green (00:29:26):
So it does say that we might be seeing an increase among a population that already has... those are really high rates of reporting anxiety and depression. More likely than not, LGBTQ youth are experiencing anxiety and depression. And that's true last year and it's more true this year. And once again, if you look on the right side of the graph where we break out that data in terms of race ethnicity, when we look particularly at depression, we're seeing greater risk and greater rates again, among those who are younger who are transgender, but also LGBTQ youth of color particularly looking at the differences in black youth in terms of rates of depression, something that hasn't received as much attention in previous years as it needs to now and thinking about all that 2020 brought for those youth.
Amy Green (00:30:16):
When we asked youth how often they would describe their mental health as poor, so a frequency question, never, sometimes, 70% said their mental health, they would describe as poor most of the time or always during COVID-19. So really showing that mental health is a struggle for these youth. And unfortunately, when we asked about mental health care, nearly half said they wanted it in the past year, but they couldn't get it. If you look at that pie chart there, you can actually see that by far the largest portion of the pie, only 16% didn't want it, 36%, so a little more than one in three wanted it and got it, but nearly half you said they were struggling, they wanted mental health care, they couldn't find a way to access it.
Amy Green (00:30:56):
And we know there's a number of barriers. We had questions asking them about barriers and they range from things like fears about how to even talk about mental health, how to find a provider, how to talk to their parents and get help, to challenges in finding LGBTQ competent providers where they live, as well as things like costs and concerns about having insurance coverage. And if you look at the full report on our website, you'll see that there's large disparities in who is able to access care.
Amy Green (00:31:24):
So if we look at that 48% compared to that 36%, overwhelmingly LGBTQ youth of color were in that group who wanted mental health care but didn't get it and less likely to have received mental health care despite the fact that I just showed you those slides showing the elevated rates of suicide risk, anxiety, and depression. Going back to the original report where we talked about the concerns that we had starting just in March 2020 about LGBTQ youth, one of the main things that we've been concerned about is the idea that these youth would be isolated and distancing in places where they didn't have support for their identity.
Amy Green (00:32:06):
And in fact, nearly half of LGBTQ youth ages, 13 to 24, including 60% of those who were transgender or non-binary said that COVID-19 impacted their ability to express their LGBTQ identity. And while the rates are higher for those who are 13 to 17, so that's the group that we would assume would be most likely to be living with their families, and we'll talk a little bit later about the rate at which families affirm LGBTQ identities, but it's not high, the rate for those 18 to 24 are also high.
Amy Green (00:32:38):
And one of the things that we've heard repeatedly on our crisis lines is from LGBTQ youth who were in college or out on their own and they were in a place where they were able to be out, accepted and express their identity only to have to return home as the pandemic began to families who are unsupportive and resulting in them having to conceal their identity from their family to hide who they are, which I'm sure you can all imagine can be quite challenging and stressful to happen every once in a while, but for someone to have to conceal and hide who they are on a daily basis after being in a place where they were able to express themselves and safely be who they are, can be incredibly challenging and obviously relating to some of the concerns that we're seeing for LGBTQ youth across the pandemic.
Amy Green (00:33:35):
And this kind of goes with something that Dr. Kelleher was talking about, going back to fears about how the economic impacts of the pandemic impact youth. So among our LGBTQ youth, we found that 30% said they had trouble affording food in the past month. Asking them about food insecurity, whether or not they ever went hungry, or their family didn't have money to buy food, 30% of them, including half of those who are native or indigenous.
Amy Green (00:34:04):
And I think that we've probably seen the videos of earlier in the pandemic, the lines for food banks with cars lined up, but the reality of this and how frequently it was happening for these youth is quite severe. And as you can see on the right-hand side of the slide, there has been a strong relationship, not surprisingly, between experiencing this type of food insecurity and concerns about how they were going to eat and suicide risk with 11% attempting suicide in the past year if they didn't experience food insecurity.
Amy Green (00:34:36):
This doesn't necessarily mean that they were living in abundance, but that that wasn't as much of a concern. Those who were experiencing food insecurity, 25% of those reported that they attempted suicide in the past year. And so while we need to invest in mental health and mental health care like Dr. Kelleher said, we also need to really invest in the impacts of poverty and preventing poverty and helping families and communities to generate wealth so that we don't see these types of impacts on youth for their wellbeing.
Amy Green (00:35:13):
So going back to the conversation that we had earlier about minority stress, talking about the impact of discrimination, victimization and stigma and how that impacts youth and how it impacts youth who have multiple marginalized identities. So in this first slide, I'm going to show you the rates of attempting suicide based on experiencing discrimination. So we asked youth about three aspects of their identity. We asked about their sexual orientation, we about their gender identity and we asked about their race ethnicity, and for each individual their experience of discrimination.
Amy Green (00:35:46):
So in the past year were you discriminated based on your sexual orientation? 9% who said "No, I haven't," attempted suicide, 21% who said, "yes, I had," attempted suicide. And we'd see similar impacts there based on gender identity and race ethnicity as well so almost like a doubling effect. But then we also know these identities don't operate in isolation. So if we look at cumulative experience of discrimination, we can see how multiple forms contribute to suicide risk.
Amy Green (00:36:23):
In this case, 7% of LGBTQ youth who said they didn't experience discrimination based on their sexual orientation, gender identity, or race ethnicity, so it's youth who did not experience it, 7% of them attempted suicide. If we look at each cumulative impact, so one type 13%, two types of their identity, 24%, all the way up to LGBTQ youth who were discriminated based on their sexual orientation, their gender identity and their race ethnicity, 36%, more than one in three reported they attempted suicide in the past year.
Amy Green (00:36:56):
And unfortunately, even with the progress that's been made for LGBTQ rights, discrimination remains common with more than half of LGBTQ youth reporting they experienced it in the past year based on their LGBTQ identity. And in 2020, we have even higher rates of discrimination based on race ethnicity, for black and Asian-Pacific Islander youth with 67% of black LGBTQ youth and 60% of Asian-Pacific Islander LGBTQ youth reporting they were discriminated based on their race in the past year.
Amy Green (00:37:25):
Really showing that again, while we need to attend to mental health, we can't ignore what's happening in the broader society and how those experiences are impacting our youth in ways that really contribute to suicide risk. And so now I'm going to turn to a little bit briefly, and I'm happy to talk more about this in the question and answers about what are the ways that we can interrupt this? What are some of the things that we can do to reduce the risk?
Amy Green (00:37:56):
So fortunately, one of the most consistent findings relates to affirmation and support from others. So in the grand scheme of things, it's not that challenging or expensive as an intervention of providing affirmation and support to tell someone that they're accepted for who they are and they're loved for who they are, that's a pretty cheap intervention if you can get people to do it. And so we asked youth about places where they felt affirmed in their LGBTQ identity and focused on places in our recent survey where LGBT youth were spending most of their time.
Amy Green (00:38:26):
So that's online, at school, whether that was remote or in person and at home. And as we suspected based on past data, only about one in three LGBTQ youth reported that their home was LGBTQ affirming. So most youth were indeed in a place where they weren't affirmed in their LGBTQ identity. But half said their school was. And for most, online was a place where they could find affirmation support. In each of these places, when they're affirming is associated with reduced risk for suicide.
Amy Green (00:38:56):
But school is generally among the strongest, and this is true in our past research as well, that school is a very strong, protective factor when it's affirming for LGBTQ. And so it's a place where we need to invest in training and support of all school staff to ensure that more than 50% of youth describe it as affirming. We'd see a large change in the wellbeing of LGBTQ youth if that number went up to 50, 60, 70% of LGBTQ youth who had an affirming school ideally with the goal that we would get to a place where every single LGBTQ youth went to a school where they felt they were affirmed and able to be themselves in their identity.
Amy Green (00:39:35):
And finally, I'm going to leave you on one last slide about the wellbeing of LGBTQ youth, and that is that although LGBTQ youth discussed a number of challenges in their lives and ways they were struggling across the COVID-19 pandemic, they also lifted hundreds of ways they find joy and strength, and that includes things like visibility and connections to LGBTQ community, having access to supportive and accepting friends and family. And we know from my research that having at least one accepting adult results in LGBT youth being 40% less likely to attempt suicide. And so that's why we encourage all adults to work towards being an accepting person for LGBTQ youth.
Amy Green (00:40:17):
And if you look at this and you look at this list, you can see that the ways to improve things and the ways to support LGBT youth are really quite simple, it just takes all of us being willing to be that person who accepts, supports and loves an LGBTQ youth. And so thank you, and I'm looking forward to taking questions and talking more about this during our question and answer section.
Kathryn Santoro (00:40:39):
Thank you so much Dr. Green for The Trevor Project's leadership both the reading public awareness through your research and providing the crisis intervention services you mentioned to really confront this public health crisis. Blue Cross Blue Shield of South Carolina Foundation is a statewide leader, partner and funder addressing health gaps for South Carolina's economically vulnerable citizens and serves as an agent of change to support innovation and value added public private partnerships. They have had a long standing focus on investing in the health and wellbeing of children and families. To hear more about their efforts, we are now joined by Erika Kirby, the executive director at Blue Cross Blue Shield of South Carolina Foundation. Erika?
Erika Kirby (00:41:32):
Thank you, Kathryn and thank you to the NIHCM team and my fellow panelists, Dr. Kelleher and Dr. Green. This is such an important topic and we are pleased to provide a snapshot of some of the activities and projects and efforts going on in South Carolina. So on behalf of our board of directors, again, I thank you for the opportunity to tell the story about what's been happening in South Carolina and some of our efforts.
Erika Kirby (00:41:59):
I'll first start with a little bit of an overview about the Blue Cross Blue Shield of South Carolina Foundation. As Kathryn said, we are a statewide health foundation established in 2003 and since then have continued to focus on investing in all 46 counties across the state, looking to improve access to care. We've focused on workforce efforts, improving the quality and value, certainly investing in a two generation approach and all towards the eye of those that are economically disadvantaged and how do we bridge health and health care?
Erika Kirby (00:42:38):
In 2018, we took the added step of prioritizing three key health issues, those being oral health, mental health, and diabetes, and kind of embedded with that certainly is a focus on health equity as well as looking at addressing the social determinants of health, not only from an issue perspective, such as food insecurity yet also from a convening perspective that as a corporate philanthropic organization lends us the opportunity to oftentimes pull different groups across sectors, across communities together.
Erika Kirby (00:43:19):
As we look at the status of mental health and wellbeing in South Carolina and this certainly reinforced much of what Dr. Kelleher and Dr. Green have already addressed in terms of what was already happening with our mental health of our young adults and young students prior to COVID, but certainly in light of COVID as we have looked at the impact of COVID prior to COVID, we have ACEs data and we have almost two thirds of our adults report at least one ACE, 22% report two plus and we have roughly 16% report three or more ACEs.
Erika Kirby (00:44:02):
A study done through parents and caregivers in conjunction with our Children's Trust of South Carolina and the South Carolina First Steps Organization found that 83% of these parents and caregivers reported higher levels of stress and anxiety just simply due to COVID. So we look at the rates of untreated depression and here at graph pulled from partner organizations looking at suicide rates of South Carolina. And I dropped this in here because it provides context not only for South Carolina, yet as we look from a South Eastern perspective, how we compare to rates relative to Georgia and North Carolina, our sister states, we ranked 41st in the nation for overall child wellbeing.
Erika Kirby (00:44:56):
And as we look at the suicide rates, in blue is South Carolina continuing to increase and at a much unfortunate, greater cliff than our neighboring states. So the foundation's strategy to support mental health as indicated earlier in 2018, early beginning in 17, 18, we wanted to take a more intentional focus into how we were able to use our role, our statewide presence and the different assets that we have, the convening power, the ability to connect individuals across sectors and what was the unique role that this foundation could play in addressing mental health and wellbeing in our state?
Erika Kirby (00:45:47):
So our overall strategy includes a strong focus on prevention and earlier identification, yet also a connection to services and workforce and building up a workforce for health, in this case, a workforce for mental health. And I made this note that when we intentionally looked at what we could uniquely and how we could uniquely serve our state, it's with recognition and acknowledgement and appreciation certainly that there are many partners in South Carolina doing phenomenal work and there's a lot of organizations, efforts, conversations going on.
Erika Kirby (00:46:25):
So our intent was to identify how we could add in, accelerate, support innovation, address some existing gaps to what was already currently going on. So with the three main themes of our overall mental health strategies, we have a number of projects in each of these themes, but for today's discussion, I will just briefly touch on one example from each of these four. Starting with prevention, looking at increasing awareness and stigma reduction.
Erika Kirby (00:47:07):
We certainly have been able to have conversations with organizations, in this slide we're highlighting our partnership with NAMI, the National Alliance for Mental Illness in the South Carolina chapter. And when we sat down with them and had conversations, this was really back in 2018, about their footprint with using the national developed, Ending the Silence for middle and high school students, it became clear that this was, as Dr. Green said, kind of creating this perfect storm of what else was going on and what needed to be filled, what were the gaps, what opportunities.
Erika Kirby (00:47:50):
And where they were at was often dependent upon smaller grant funding or very localized grant funding. So as we spoke with the team and leadership, I'm able to really see opportunities of how we could scale the Ending the Silence curriculum, more of a regional approach. And so not only did this provide more consistent presence at a local place, but then also identified additional schools and counties based on higher rates of suicide and suicide attempts.
Erika Kirby (00:48:31):
So as we looked at this design and really a co-design, if you will, of how to structure this to increase access, to have that more consistent localized presence, being able to break funding together from other funds that either the state association had or even local chapters that had been received, really being able to set our eye on reaching over 150,000 teens through this regional tiered approach and being able to evaluate more intensively than what had previously been able to do in South Carolina and with that information, being able to see significant increase in the contact to the crisis text line and suicide prevention line.
Erika Kirby (00:49:24):
And because of these trainings, and these are just accomplishments to date, 180 students came up to the presenters, which include an adult as well as a peer that has experienced and has lived experience with mental illness. Over 50 students have been able to identify an immediate crisis need and were connected to services. Without this ability to scale and replicate and design this regional approach prior to COVID, I think we would have really found ourselves in a different place.
Erika Kirby (00:50:05):
What this has enabled is even though they transitioned to doing virtual workshops and virtual trainings to the best of their ability, they had connections with schools prior to COVID. And so it provided an added mechanism and an added venue in which to support schools, the staff, the teachers, the families and the students. Also along the realm of prevention and moving upstream and looking at the adverse childhood experiences and protective factors, we have certainly recognized as a health foundation, the connection between ACEs and health outcome.
Erika Kirby (00:50:54):
In conversations with, in this case, our partner Children's Trust of South Carolina among others really to develop a more concerted statewide effort to address ACEs and build protective factors, and there's two components to this. And when we started these conversations acknowledging that there were a lot of partners working on and supporting, being trauma informed, training workforce, making training available to the clients that they served, what was still missing and what did we need to do as a state to really accelerate our efforts at addressing ACEs and building protective factors?
Erika Kirby (00:51:37):
And where that landed was a two-pronged approach to have better information to guide decisions, and to then be able to use that information and data and translate that into action, all to impact health and address health disparities that we know have the short-term and long-term implications as a result of this trauma. The first element was the data and training arm. And so we looked at this, we were able to enhance the data collection efforts within the state, and as a result of that, able to have county level data.
Erika Kirby (00:52:19):
And this is just... there's an image of some of the county level reports that were able to be generated. But being able to have that more granular level data, we all know health is local, right? And being able to have information that, to also to Dr. Green and Dr. Kelleher's point of using information in a way that really depicts the populations in the communities most accurately. And so this county level data has been instrumental in using to educate and convene partners.
Erika Kirby (00:53:01):
It certainly has been also helpful in soliciting information on aligning efforts, which I'll talk about in the next slide, but very much looking to identify per county and then at a regional level, what were some of the issues, the ACEs that were more prevalent in one county versus what may be seen in a different county? With this information, certainly trainings to increase the awareness, also different studies and benchmarks of what the perceptions of key individuals were regarding the impact of ACEs, their level of understanding and what potential strategies and solutions could we take action on as a state?
Erika Kirby (00:53:54):
The second part of this overall commitment has been working at the community level. So not only what data do we have, trying to strengthen the data, but then how are we using this data to translate into action? So to complement, having a stronger, more robust lens and profile on the impact of ACEs in South Carolina at different levels, state, regional and local, the development of the Empower Action framework, which was, again, trying to help communities translate the whats into the hows.
Erika Kirby (00:54:32):
And so equipping them with the data but then walking them through five steps of using this information and then looking across sector to engage schools, governments, parents, different community members and providers, health systems, safety net providers really all towards the eye of aligning on increasing their understanding of ACEs, how to build protective factors and what they could do as a community as well as in their own organization to really change the dynamics and change the narrative within their community.
Erika Kirby (00:55:15):
So where this is at, three counties in the state are going through this framework currently and they are using this to develop an action plan, really again, to look at how they can look at this two generation approach, to build protective factors, to reinforce earlier detection and acknowledging that this is... really has been an opportunity to respond to the needs as partners were expressing. They value these data, but they wanted to know how do we actually use it and what do we do with this information?
Erika Kirby (00:55:58):
And so this framework was developed in response and throughout the end of 2021, all of these action plans will be developed. There was somewhat of a delay due to COVID and of the hindsight 2020 brought us, but the coalition students stopped meeting. They had to change to virtual meetings, so many conversations did, yet their commitment to these issues and these discussions, certainly that has been accelerated and elevated due to COVID. Their commitment is something that we applaud and appreciate.
Erika Kirby (00:56:44):
Moving on to connection to service. As a philanthropic organization, we tend to look at grant opportunities and needs. Sometimes the simple is the most effective, and in this case, it was partnering with the Mental Health America Greenville as our state's satellite for handling the national suicide prevention line calls. And what they needed was a more sophisticated capability to handle the calls coming in. So again, we started this prior to COVID and we're able to have in place expanded phone capabilities going from one line up to 30 calls, so where they could significantly increase and keep calls in the state.
Erika Kirby (00:57:40):
And why this is important is prior to this expansion, when the calls were diverted to an out of state call line volunteer and recipient, they perhaps did not know the context and resources that were available to an individual locally. And so by keeping these calls in state, we're not only able to connect them better to resources. To date, there's been a significant increase in call volume but we've been able to... or Mental Health America Greenville has been able to respond to that due to this increased capacity.
Erika Kirby (00:58:25):
It has allowed 29 lives to be saved since implementation of this phone system. And so again, just sometimes being able to hear what the needs are, what our partners are telling us and responding to those needs and being able to fill in gaps, that sometimes seems so basic, but in the absence of funding for supporting something like expanded phone lines, we would've missed the opportunity to support those individuals needing these services at such a critical time during COVID.
Erika Kirby (00:59:02):
The last element I will touch on is workforce. And so we've had a long history of promoting a workforce for health and COVID certainly has elevated and surfaced the need for more mental health services, and certainly and more specifically to youth in schools, the school-based mental health services. In South Carolina, our state department of education and department of mental health came together to outline a vision by 2022 that all schools would have access to a mental health clinician.
Erika Kirby (00:59:39):
And so the foundation has been able to support that vision through two projects. The first being the engaging in training with compassion project to really create a trauma informed and trauma responsive school environment. This is a tiered approach that is working in two school districts, coupling the mental health centers and the schools within these school districts to provide training for all of their teachers, support and increase awareness of the school administrators, and then equipping the school-based mental health clinicians with added professional development in tools and resources and guidance on how best to support a particular child's needs.
Erika Kirby (01:00:30):
Second element of this has been our efforts to really look at how do we develop a sustainable school mental health workforce, and a pathway to increasing the workforce of mental health clinicians specifically working in that school-based setting. And so this is looking at really providing clinicians with what it's like to work in a school setting. Oftentimes as individuals leave with their degree in hand, they may not have had exposure to working in a school setting. So providing them an opportunity to know what it's like to work in a school setting all towards the eye of increasing recruitment and retention and providing, again, more robust services for right needs to address the right... or right strategies to address the right needs at the time.
Erika Kirby (01:01:33):
And also as part of this, really beginning to explore different types of school mental health support, and how do we look at different individuals such as community health workers or behavioral health interventionists, perhaps those that are not trained as a mental health clinician, yet how do we look at expanding supports toward that multi-tiered system of support, tier one, tier two, earlier identification, increasing awareness to allow our clinicians to focus their time and meet the needs treatment wise, but then also being supported to go down into tier one, tier two of overall education awareness and really creating a much more comprehensive approach to school-based mental health services?
Erika Kirby (01:02:30):
For the sake of time, that's just a quick overview of each of these projects. Again, certainly it goes without saying that we owe much appreciation to our partners. There are many partners I did not mention during this, but it really is our effort at trying to meet the needs, respond to gaps, accelerate efforts in innovation. And I close with this slide. If any one has been to South Carolina, we have beautiful beaches. And one thing that is true though, is they're constantly changing.
Erika Kirby (01:03:04):
And so our challenge is to constantly evolve, know when to shift, how to shift in response to what's going on around us. And it is something that mental health is an ongoing commitment that we see and its connection to overall physical wellbeing and appreciate the opportunity to mention a few projects and happy to answer any additional questions during the Q&A section. And with that, I'll turn it back over to Kathryn.
Kathryn Santoro (01:03:41):
Thank you so much, Erika for your leadership and commitment and for sharing these excellent projects in South Carolina. We'd like to use the remaining time to engage in a Q&A session with our audience. So please continue to submit your questions in the Q&A tab and I'll ask our panelists to come off of mute at this time. And following up from Erika's comments on the mental health workforce, we had a few questions come in on mental health workforce shortages and the impact on access. And are there any lessons learned or emerging technologies coming out of the past year that you think might help alleviate this problem going forward? For any of the speakers.
Erika Kirby (01:04:35):
Thank you, Kathryn. This is Erika Kirby. I'll provide an initial response and certainly let my fellow panelists respond. So I think this past year has elevated tele-health and virtual modes of service delivery across many different sectors, and certainly to include the school systems and the education system. South Carolina is one of I believe 15 states in the Healthy Students, Promising Futures Learning Collaborative, really looking at increasing the use of telehealth, currently they serve 80 plus schools.
Erika Kirby (01:05:13):
And we've seen that even with our work in pre-medical clinics that prior to COVID, patients and perhaps family members weren't maybe as comfortable or as willing to use virtual services. And I think with COVID, really creating this nexus of kind of eliminating all other options other than telehealth and virtual, it really has enabled a transition point and a pivotal point in which more individuals are comfortable providing services as well as using and receiving services.
Erika Kirby (01:05:54):
So I would say that that will continue to be a trend of delivering services. And for our rural communities, the majority of South Carolina counties are medically underserved shortage areas. And so the ability to use telehealth services really will equip providers be it, school, mental health clinicians, healthcare providers to reach communities, partners, families, youth that may not otherwise have access to an in-person clinician.
Kelly Kelleher (01:06:32):
This is Kelly, I just would only add to that. We are seeing increasing use of peer support and a lot of services and increasing... we have to talk about prevention here because we keep talking about treatment and we're waiting until people are sick or disabled or how far down the line and the most efficient way to do this is prevention. But of course, our current payment system doesn't support that. But as we do more and more value-based purchasing and capitation services, more systems will integrate prevention into their workforce and we can use a lot more peer and community health worker type personnel to provide those services, which is the only sensible way to do this since we've been calling for more mental health workers for decades.
Amy Green (01:07:21):
This is Amy. I agree with what both of them have said and I want to add on one of the things that when we talk about changes in the COVID-19 pandemic. There previously were different reimbursement rates for when we talk about mental health care and therapies for someone who's doing services through telehealth versus in-person. There's also state licensing laws that doesn't allow someone to cross state lines and seeing patients and some of those out of necessity for the COVID-19 pandemic went away in policy changes.
Amy Green (01:07:55):
And I think that there's a lot that we can learn from when everyone felt like everything was so urgent, how quickly change was able to happen in some of these areas that I know a lot of folks have called for and worked for for years, but given what we've talked about today, in terms of the urgency here, the urgency is ongoing and so I think part of it is continuing to find creative ways to make changes that increase access. Because I saw some of those questions and answers and I empathize with folks in the challenge of finding mental health care for you, then calling providers and finding that no one's there.
Amy Green (01:08:36):
And part of that is ensuring that reimbursement rates for providers encourage them to be taking on clients that have case loads, part of it is increasing our workforce and our workforce that are working in the community and not just in a lot of... I know a lot of therapists, a lot of concerns that I hear from folks are that most of the therapists, particularly who are LGBTQ competent, particularly who are competent in trans and non binary issues are private pay, which does not work for many of the folks who need those services.
Amy Green (01:09:05):
And so finding ways and funding streams that provide access to more folks because this is not something that's going away, the mental health challenges that have risen and the issues that have arisen isn't going away. And so we need to continue to find those types of solutions that in the beginning of COVID-19, and I also think Kelly had said in the beginning of the presentation, how quickly things change in terms of overnight going into a world of tele-health when this has been something that the field's been pushing for a while, but we need to keep thinking about those urgent pushes and changes.
Kathryn Santoro (01:09:41):
Great. Thank you. Kelly, you alluded in your presentation to the impact of lost revenue. Are there key services impacting children that have been cut over the past year due to the pandemic that have a proven return on investment and should be prioritized? And also for any of the speakers or maybe for Erika, how do you see private and philanthropic dollars helping to leverage some of this loss of public funding or how public funding has had to change over the past year and potentially going forward?
Kelly Kelleher (01:10:23):
So again, I don't think there are specific... so we've been talking a lot about mental health and behavioral health, I don't think there are specific services that went away but what did happen was that many vulnerable child serving sectors that prevent children from having problems went away. So many childcare services for families closed due to the pandemic and people being forced home from work and not being able to gather because they were living on the edge.
Kelly Kelleher (01:10:55):
Many afterschool programs have closed in our area and I see that nationally that's becoming increasingly common. Programs that serve children, we know that preschool is one of the most important things long-term prevention that people can do to get kids kindergarten ready and able to learn from school and focus on third grade reading as a marker of long-term success. Those things all suffered. Another thing that suffered tremendously was primary care infrastructure for children.
Kelly Kelleher (01:11:29):
So children in rural communities and seen at community health centers were particularly vulnerable to closures of hospitals and practices around the country. And so many children did not receive their well care shots. I mentioned the measles epidemics and other things that we're expecting, many of those children will not be able to go to school because of legislation that forbids it in the fall. So they will be without immunizations and unable to attend school for weeks on end, again, even if school restarts. So we have some rapid work. We are mobilizing vaccine clinics over the summer at some of the school sites to have families come in and get caught up because we're expecting many of those children to be excluded come the fall.
Erika Kirby (01:12:18):
This is Erika. And I would add to your question, Kathryn, kind of the role of perhaps private philanthropic organizations during 2020 and certainly as we're halfway through 2021, looking to continue to establish this public private partnerships. And it would be the examples I provided are with nonprofit organizations.
Erika Kirby (01:12:50):
So I certainly want to elevate the role that nonprofit organizations can be and can play that they oftentimes are serving the most disparate groups that are in rural communities, that are lower income, that are facing more of significant health disparities. And so the more that health systems, organizations, schools, et cetera, can partner with these types of organizations that provide a key service, be it food pantries, food banks to address even looking at food insecurity, philanthropic organizations have pivoted extensively in 2020 by allowing a greater flexibility in use of dollars.
Erika Kirby (01:13:40):
A survey done in South Carolina of many of our state's nonprofit organizations, and I can certainly provide the reference to our statewide association of nonprofit, identified that some of their key needs for social service nonprofits had been needing to support the mental health of their staff and then in turn that the mental health of the clients that they serve, in addition to food support as well as perhaps more in immediacy of early 2020, some of the PPE and protective equipment needs. And so I just want to flag that also partnering with the nonprofit organizations really helps bridge and make for a more robust public private partnership.
Kathryn Santoro (01:14:35):
Great. Well, thank you. And unfortunately, we are out of time today but I do want to thank our excellent panel of speakers for being with us and sharing their valuable work and perspectives. If you missed any of their presentations, we will be sharing a recording and copies of the slides are available on our website. We also want to thank our audience for joining us, thanks for your excellent questions. We also would love to have your feedback. Please take a moment to complete a brief survey, which can be found on the bottom of your screen. And please also check out our other resources on our website, including recent infographics on children's health and register for our upcoming webinar, Achieving Health Equity for People with Disabilities During the Pandemic and Beyond. Thank you all again for joining us today.
Speaker Presentations

Kelly J. Kelleher, MD
The Ohio State University and Nationwide Children’s Hospital

Amy E. Green, PhD
The Trevor Project

Erika Kirby
Blue Cross Blue Shield of South Carolina Foundation
More Related Content
See More on: Coronavirus | Maternal and Child Health | Social Determinants of Health