Webinar
Mental Health Solutions: Improving Care
Time & Location
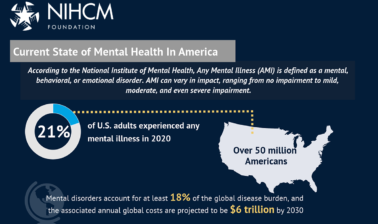
The COVID-19 pandemic has highlighted the importance of mental health but it is still difficult for many to get the care they need. Many people reported poor mental health after experiencing stress and worry around the pandemic. However, one-third of adults in the U.S. went without mental health services or medication when they thought they might need them. Barriers to accessing mental health care, such as social stigma, scarcity of services, and affordability, make it difficult to receive treatment.
In this webinar, we heard from mental health leaders who are working to improve access to mental health care. Speakers discussed:
- Guidance to individuals and families on navigating mental health, including diagnosis, treatment, and recovery
- Community and peer support for mental health and the work to transform care to be culturally responsive care and focused on social inclusion
- Providing high value and appropriate support such as integrating behavioral health into primary care
0:06
Good afternoon, I'm Kathryn Santoro, Director of Programming at the National Institute for Health Care Management Foundation. On behalf of NIHCM, thank you for joining us today for this important discussion on ways to support access to mental health care.
0:22
Nearly one in five Americans live with mental illness, and despite growing awareness and understanding of mental health, it is still difficult for many to get the care they need.
0:32
Over half of adults with a mental illness do not receive treatment.
0:37
Many Americans live in areas with a shortage of mental health professionals and experience a variety of barriers to mental health services.
0:46
Additionally, the COVID-19 pandemic has exacerbated and contributed to existing mental health challenges and increased the demand for services.
0:56
Barriers to receiving mental health care range from affordability and availability challenges to the persisting stigma associated with mental illness.
1:08
May is Mental Health Awareness month and a time to address the impact that mental health has on the well-being of all Americans, and a time to collectively work to address barriers to improve access to mental health services for those who need them.
1:24
In supporting mental health and access to services we hope that anyone affected by mental illness can get appropriate support and care..
1:33
Today we will hear from a prestigious panel of experts to learn more about mental health and strategies to improve access to care, including culturally responsive support and crisis services.
1:46
Before we hear from them, I want to thank NIHCM’s President and CEO, Nancy Chockley, and the NIHCM team, who helped to convene today’s event.
1:55
You can find biographical information for our speakers, along with today’s agenda, and copies of their slides, on our website.
2:04
We invite you to join the conversation on Twitter, using the hashtag #MentalHealthSolutions.
2:12
I am now pleased to introduce our first speaker, Dr. Ken Duckworth.
2:16
Dr. Duckworth serves as the Chief Medical Officer with the National Alliance on Mental Illness.
2:22
Dr. Duckworth is a leading mental health expert – board certified in adult and child/adolescent psychiatry, and has extensive experience in both the public and private sectors.
2:34
We are so honored to have him with us today to share NAMI’s recent work on mental health. Dr. Duckworth?
2:40
Thank you, Kathryn. I'll be speaking for about 10 minutes or so and make sure we have time for conversation.
2:47
We have two other terrific speakers as well. So reduce suffering on your part. I only have two slides.
2:54
So, let's take the first slide please.
2:56
So, as Kathryn mentioned, you know, the pandemic has been a watershed moment in mental health.
3:05
In many ways, one of the biggest is many more people reported having the experience of a mental health condition.
3:13
And, in this, I say, best of its kind survey, to date, the CDC indicated in an online survey of June, 2020. So, that's 3 or 4 months into this, reported out in August, 2020.
3:30
A pod is closest to real-time biopsies.
3:32
You're going to find many people, 41% reported a true mental health condition. So they used the PHQ 9 G 87, a trauma scale, and it's validated.
3:42
And if you take a look at this anxiety and depression 31% trauma, 26% increased substance use, 13.3%, suicidal ideation increased.
3:58
So we're a pretty high number, over 10%, and it was higher in young people.
4:04
They didn't do age, um, you know, 10 to 17. They started at 18. They wanted to be adults.
4:10
Hispanics were higher, black respondents were unpaid caregivers.
4:15
For adults, we're hire much more suicidal ideation, essential workers.
4:22
So this is a transformation in my way of thinking about this, is that mental health went from the problem to all we have.
4:31
I was impressed that I probably did eight times as many media conversations in 20-20.
4:37
That's in 2019.
4:40
People want to talk about recovery telehealth, connecting with others how to find a therapist because of the supply demand mismatch.
4:49
And, um, I feel like it was a transformational moment.
4:54
And if there is a silver lining to the mental health aspects of the pandemic, it is that so many people experienced it in themselves, or in their family members.
5:08
Right.
5:08
So with 41%, if you have five people in your life, it's now statistically unlikely that none of them are involved in having a mental health condition that they're experiencing.
5:21
Let's go to the next and final slide, Kathryn.
5:26
So I took advantage of this opportunity to write NAMI’s first book.
5:31
And I made a very deliberate, intentional set of decisions about the book, The National Alliance on Mental Illness, which is your largest grassroots organization in America for people with mental health conditions, and those who love them.
5:47
That's never had a book, And I always thought it would be a good idea.
5:52
I want to emphasize this book, which is up for sale on Amazon.
5:56
All proceeds go to NAMI, this is a love gift on my part.
6:01
This is something I just wanted to do for noemi. The book's gonna come out in September, and I wanted to tell you a little bit about it, because this is one of the things that NAMI is doing.
6:11
NAMI also led the 9 8 8 crisis Phone call movement.
6:17
So, you know, 9, 8, 8 will hopefully become, then 9 1, 1 of mental health crisis for the Suicide, National Suicide Crisis Prevention Life, Suicide Prevention Lifeline.
6:31
It doesn't really create services. That's another advocacy challenge.
6:35
But I would say that's a big, recent NAMI activity, the book I interviewed, 130 people, I interviewed real people who used their names.
6:44
I did not use composite people or fake people, as many books do.
6:50
The whole idea of this is to reduce the shame discrimination, Those walks that you hear in the background are two dogs on a nearby neighbors dogs.
7:00
And they've decided only during my talk, to get quite involved in battling out each other. So, don't worry if nothing terrible is happening. It's just two dogs. This is the joy of home.
7:12
Work in the pandemic, 130 people. About 80 of them have first person lived experience, About 50 of them are family members.
7:19
And I asked them, what worked for you, what made a difference for you.
7:23
What helps you communicate in your family?
7:25
How did you manage some of the tensions in our field?
7:29
And then I also did something that I hadn't seen in a book, but I always wanted, which was to have americus experts answering the most common and important questions that I get.
7:45
And so this is both first person questions and family questions, So the first person questions would include: why should I participate in research?
7:57
I get that I have bipolar disorder. Do I really have to take these meds forever?
8:01
That's by Dr. Andrew Nierenberg, Mass General Hospital.
8:06
What do I think about interventions for self harm?
8:11
Here's a discussion of DBT.
8:20
There used to be examples of first person questions, and then the family questions.
8:26
For example, I had Dr. William Miller, who invented motivational interviewing.
8:30
Answer the question, How do I get my family to talk to someone who doesn't seem ready for help?
8:37
Dr.Christine Moutier, the Medical Director of the American Foundation for Suicide Prevention.
8:42
Answer the question: My family member is expressing suicidal thoughts. How might I approach them?
8:49
So the joy of this project is this is a practical book that is based on real people's stories and what they have learned.
8:57
In this way, the real people I interviewed are also experts.
9:02
They have a different kind of expertise than the Director of the National Institute of Mental Health, or a World famous researcher, but they are also experts. That is the joy of this book.
9:15
So, if any of you are inclined to buy it, you know, go right to Amazon.
9:22
If you want me to do an event for your organization related to the book, send me an e-mail.
9:30
I have 130 people from 38 states, and I'm going to be traveling to America in the beginning of September.
9:37
And I'll have people from the book on the stage with me everywhere I go across the country.
9:43
So 98 is a big material intervention that NAMI's doing, and the other big project happens to be this little book that I've worked on.
9:52
9 8 8 is kicking in around July 16th.
9:56
There's going to simplify people's experience of seeking crisis services, but it does not itself create services.
10:05
So, I want to emphasize, those are two major things that NAMI is working on, support groups, peer support groups, educational programs, educational programs, and schools.
10:17
It covers the entire waterfront of Peer support.
10:20
That is all three whether the peer as a first person lived experience or as a family member. So I want you to know about NAMI, I want you to know about nominees , a beautiful organization filled with amazing people. I only scratched the surface in terms of my interviews. So Kathryn, I'm gonna stop my remarks there. I think for 10 minutes. I'm happy to pick up questions near the end of today's session, and thank you for having me.
10:48
Thank you, Dr. Duckworth, for your leadership and for sharing a little bit about this book. And we look forward to having you on for the Q&A.
10:56
Next, we will hear from Dr. Chyrell Bellamy, an Associate Professor in the Department of Psychiatry. She is the Director of Yale’s Program for Recovery and Community Health and serves as a Senior Policy Advisor to the Connecticut Department of Mental Health and Addictions. Dr Bellamy has experience as a frontline service provider, community educator and organizer, and as a community and academic researcher.
11:24
We are grateful Dr. Bellamy is with us today to share more about peer support and culturally responsive approaches to mental health care. Dr. Bellamy?
11:33
Dr. Bellamy.
11:36
Thank you so much, Kathryn, for the introduction. It's a tough act to follow after Dr. Duckworth. Very excited to hear about the book that you did for NAMI, and particularly that you're honoring lived expertise. So I'm happy to get a copy of it in my hands. Thank you for that. So, if we can get started with the presentation, next slide, please.
12:14
So let's just get started. Here's a poem that was written by my friend and colleague, a playwright and artist and poet who lives in San Francisco. And we wrote a book together called Positive Negative Women of Color in HIV and aids. We need you,
our brothers, our sisters and our people.
12:39
Help us. We affirm ourselves in loving ourselves. Whoa, that's when we can't stand because the souls of shoes have traveled on our backs for so long. We need our brothers, our sisters, and our people.
12:53
Thank you.
12:55
Next slide, please.
12:59
Keep going.
13:01
So, unfortunately, the situation that we're dealing with right now is pretty dire. We know that Black and Latin X people and people with mental illness are dying 25 years earlier than the rest of the rest of society, and there's a lot that we need to do to change that. Next slide, please.
13:23
For black and latin X communities, we are still needing to address things like stigma and discrimination with mental illness. Again, as Dr.Ghaffar mentioned, COVID has unified us and in a sense. Right, so, that people struggle, we know that people have struggled. We know that, you know, covert has really brought to light what mental health needs, but we also know that for many people that have major challenges with their mental health stigma and discrimination continues to be something that's very real.
13:57
We need more positive messages. We need more people that are out like me, as well as others that are out about their own mental health experiences across the board.
14:10
We also need to make sure that we're doing our best to improve healthcare for all, and, particularly for blacks. Next, we need to find ways to enhance the issue around trust in the health care system that, you know, sort of plagues our communities. one way is by bringing and supporting more providers with diverse racial and ethnic backgrounds, and developing more clinical staff trained and providing culturally responsive care to our communities.
14:45
And then, we need to make sure that when people are seeking mental health services, that they have access to it, and particularly, folks have it private, or knowing, Sorry. Next slide.
14:58
So, introducing peer support, in an ideal world, because all provide peer support based on our life experiences, we do it every day, different issues, but similar results. I know for me, as a person who was, I was in my forties, having my first child. I need peer support from other moms about what it is like to be a new mom. And particularly, what does it like to be a mom who is older. I also would have benefited from peer support when I was 16 and suicidal.
15:28
And throughout my years of going to college when I was dealing with major challenges related to my mental health experience. Peer support has been defined by the fact that people who have life experiences can better relate, and can, consequently, more authentic empathy and validation.
15:46
People with lived experience can offer each other practical advice and suggestions, strategies that professionals may not offer or even know about.
15:55
Next slide, please.
15:59
So what are some of the gifts peer supporters can offer? And I say gifts because I think that lived expertise is again, the installation that I hope is possible, Particularly that's so important right now. For many of the people who are feeling the effects of long term COVID modeling one example of recovery knows there are so many different ways. So many pathways to recovery. But having a model, but it could be, and what it looks like. It's very helpful. Mentoring, coaching, engagement, and connection. The art of connection is huge. Some people just need, having someone there that they can connect to, about their home that will help experiences, but also just about, you know, what is it like to live life on life's terms, right? So, and then their street smarts and navigating the system. Navigating the mental health system.
16:54
That is, for people who have never been through the mental health experience, knowing how to connect with it, how to, how to access care, what's going to happen as they're going through the system is going to be really important. Community networking. And, again, community connection is also key. And I also have here that has declined, which is a term that's a phrase that was coined by the United Colored Women Lead back in the early 1900s. And lift as we climb essentially means that as we are climbing the ladder of success, that we are able to grab a person's hand next to us so that they are climbing with us. And that's just really key to the work that we're doing in the field of peer support. Next slide, please.
17:41
Now, here's just some initial evidence and we've done a lot of work at the Yale program for Recovery and Community Health under the leadership, The leadership and my mentor, so particularly the outcomes are equivalent to non peer support providers with some studies showing slightly better outcomes with peer support staff.
18:06
Also that longer community tenure and those receiving peer support and one randomized controlled trial peer support staff. So, ability to reach people who have more vulnerabilities and or are harder to engage. And that's by my colleagues here at Yale.
18:30
But we know that we are only scratching the surface, and we're really encouraging NIH and other funders to support more research, because more research is needed to examine the effectiveness of peer support. Not only mental health, but across a variety of different fields, because we do know that it works. And particularly, to examine the culturally responsive approach to it.
18:55
Next slide.
18:58
So introducing the IMANI Faith faith Based Recovery Program. And this is a project that's currently being funded by NIH via one, but also we do programming through Connecticut's DNS, and Sam sent through the state opioid recovery response. So we aim to promote healing, health, and healing for ourselves and our communities, how we do this by creating a sense of unity, that we are in this together, creating a sense of collective responsibility through a participatory process and key to the work that, you know, we do and community, but that all of us should be doing. And community, really involves participation, participation by those with lived experience, by family members, as well as by your neighbors, policymakers, leaders, et cetera.
19:50
Next slide, please.
19:53
This is just a photo of some of my colleagues.
19:56
And these are just some of the pastors who are involved in the MIT Breakthrough Initiative. Next slide, please.
20:12
And these are actually, some of our facilitators are, are Black and latin X facilitators, who we've trained to deliver the MIT breakthrough, a monolithic space, and for churches, as for latin X churches, and poor black churches, and the state of Connecticut.
20:26
And we're really providing, well, well, well, in mining, to develop, initially, to help people who have issues related to opioid use, and particularly addiction in general. We know that mental health is a huge issue for people who use and addiction. And so now is the time to make sure that we are not separating these issues that we are impacting now, half as much as we are addressing issues related to addiction.
20:53
Next slide, please.
20:56
And this is just a quick overview of the money you've given, feel free to reach out to me. But it's a six month process, which includes 12 weeks of classes and activities focused on the eight dimensions of wellness. developed by a lived experience research who is amazing as well as Dr.Michael Roe. And the five R's of citizenship. So, we combine those two, and we train people around those areas, as well as provide a sort of wrap-around peer support, as well as Community support. Every Monday project is facilitated, facilitated by a person with lived experience, as well, As a faith based member of that church.
21:40
Next slide, please.
21:43
And so these are just some of the unique factors, the money. one is that, you know, we definitely have to make sure that we are doing the ... zone. Distribution is so important that we are able to save lives and we have to do more of that. People are dying because of the opioid epidemic and we really need to do better at reaching. People address harm, reduction harm reduction is, is really key to making sure that people have particularly people who continue to use that. They have to support that. They need intensive wraparound coaching that is built on primarily issues around spirituality. Spirituality as we know is huge culturally, but I can bet that you know many of your mothers and grandmothers Okapi praying for you right now. Next slide please.
22:39
And this is just some demographic information about, you know, some preliminary work from MIT, as you can see, and this.
22:49
And I have 1008 that the folks that we are really reaching are people who have some huge vulnerability, 74% have experienced homelessness, 65% experienced violence, as many have experience, excuse me, childhood, you know, physical, verbal, or sexual abuse. As you can see, while the project does target latin X and african Americans, we also serve white folks, as well, that the project is open to anyone who walks through those stores.
23:22
Next slide, please.
23:24
And MIT has shown some significant changes. So we know from baseline to week 12 that there were changes for people who came in with using substances that at the end of 12 weeks, we saw changes in overall wellness across all of the Internet. And this was huge. And this is a huge reason why we need to continue to focus on the internet, just because it's not just about usability, et cetera. Addiction and mental health for people, it's about being able to address all those different aspects of people's lives. Next slide please.
24:02
And the next slide relates to our citizen citizenship measure. again, developed by Dr.Michael Rao and that's really across those seven domains of citizenship, such as stewardship, civil rights, caring for others, personal responsibility.
24:18
And, again, you can see that there were increases over time for, from baseline to 12 weeks, next slide. So, what can we do and what can we do today? And I'm going to start from the bottom.
24:31
So, the first thing is that, you know, even though, call, it may have the answer, the playing field, you know, so that we're all sort of impacted. We do need to do more to stop the discrimination associated with mental illness, and that makes sense. We need to find peer support, research, and programs. We need to expand these programs, particularly peer support, to communities of color, and really focus on culturally responsive care. And we need to provide insurance coverage for peer support and community health work. I think that's very key to the work that we're doing, but we do need more coverage and funding in that area. So thank you so much. And I appreciate being here with you all today.
25:13
Thank you, Dr.Bellamy for highlighting these great examples of peer and community support and for some guidelines on what can be done today.
25:23
Next, we will hear from Dr. William Beecroft Behavioral Health medical Director at Blue Cross Blue Shield of Michigan. He has been instrumental in the development of innovative programming and behavioral health, including collaborative care, crisis, programming provider, delivered care management, and first episode psychosis programming.
25:45
We're grateful to have Dr. Beecroft here today to share Blue Cross and Blue Shield of Michigan's efforts, support mental health and crisis service, says Dr. Beecroft.
25:58
And an honor to be on this distinguished faculty panel today. It's an honor for your time.
26:04
So, listen to our story of being able to help individuals in our community be able to access care.
26:12
It's been an honor in my career to be able to take care of a lot of people with behavioral health conditions, over 38 years practice.
26:20
And then, here at Blue Cross Blue Shield of Michigan, it's been an honor to really help develop, along with the team, and along with the company, these services to be able to improve access and be able to help people. And all those things that they said I did, I didn't create those all myself.
26:36
It's been a whole team that's been doing this, and we only took the literature and it's evidence based, as evidence to go forward.
26:45
But with crisis services, we'll dive right in here.
26:47
It's the right care, at the right time, the right place, same side thing, because put it together very, very well in their roadmap, crisis services. Next slide, please.
26:57
And what we're really looking at doing is trying to be able to act to do things that the public system has been doing for 20 years or more very, very well.
27:07
You can move on to the next slide, the Executive Summary slide.
27:12
In many respects, they have gotten it right, to be able to get urgent and crazy based interventions done.
27:22
Emergency rooms are very good to be able to take care of people that need services.
27:26
But for behavioral health services, they can be lifesaving.
27:29
But it can be very difficult to work with them.
27:33
I did an awful lot of that in 38 years.
27:35
And being able to have confidentiality, being able to have a quiet space, being able to have a safe space, because then anyone that's going into going into an emergency room.
27:46
There's all kinds of layers And things you can hang yourself on and hurt yourself by cutting. There's all kinds of things that can get you in traces.
27:55
So being able to look at crisis services, I think is really something that we can develop an alternative path to getting those services that are really required for those individuals.
28:08
Psychiatric, urgent care is taking on a kind of a life of its own.
28:13
But this is for just urgent care or medical services, a place that people can go.
28:18
Be able to get assessed fairly quickly if they need higher levels of care that can be helped.
28:24
But usually it's things like being able to get no prescription refill or being able to find out if they have something that needs to have a higher level of care.
28:35
Can they get an outpatient therapy appointment and kind of work in that direction?
28:40
Where we really picked up, the task is developing a system of payment for mobile crisis services and crisis stabilization.
28:50
You can go onto the next slide. We also have a crisis residential, already paid for.
28:55
The next slide shows the mobile crisis.
28:58
Um, concept and being able to have a mobile team.
29:05
You can move on to the next slide.
29:09
Maybe hanging up.
29:11
There we go.
29:12
A mobile crisis team is a master level provider, at least, with peer support that can go out to a person's home.
29:21
They can go to a primary care doctor's office if the primary care, we need to go
back one I'm sorry.
29:28
Back on the mobile crisis slide.
29:32
They can go to a primary care doctor's office who's done the screen of a PHQ nine and ask the number nine question. Are you suicidal?
29:39
and they could be able to come into that office and assess those, that individual, be able to look at what is the diagnosis that we're dealing with?
29:47
What would be a nascent treatment plan to be able to put together, be able to co-ordinate that with the individual and or their families?
29:56
We have this also available for children and be able to put together a plan that they might be able to get a psychiatric deployment quickly within maybe later that afternoon, or the next morning, get them involved in a partial hospital program, or take them to a crisis stabilization unit, which we'll talk about in a minute.
30:15
They could also go into an emergency room to be able to help provide those services that many emergency rooms don't have, especially, don't have quickly.
30:25
And in our plan, the providers that we have can either reach out by telemedicine, or they can reach out in person within minutes, two hours, not hours to days, Like sometimes happens in emergency rooms. I'm not beating up on emergency rooms. They're extremely important in our society.
30:47
But for people with behavioral health conditions, this may offer a substantial alternative level of care.
30:53
They can provide more focused, more direct care towards their names.
30:58
Next slide for the crisis stabilization unit.
31:02
Crisis stabilization unit is actually a physical location and this is an example of one of our providers.
31:09
Lobby area of the setting that you'd be walking into as a citizen coming in from a community.
31:17
You can also call them, they can do this by telemedicine to a certain extent but the actual physical examinations really need to happen in a facility and we're also looking at being able to house people overnight for the observation part of it.
31:31
Crisis stabilization units are akin to a med surg observation unit which has been around or about 25 years.
31:40
Um this is the place where you'd come in, you'd be triaged into a meeting with a mental health professional.
31:48
At that point they could make a thorough diagnostic evaluation.
31:52
An assessment work will work out a treatment plan with you of what you agree to be participating in and what your needs might be.
32:00
Be able to get a psychiatric evaluation if needed, and that psychiatric evaluation treatment could be initiated.
32:08
Also, if you didn't need the psychiatric evaluation for medications or additional psychotherapy, a mental health professional, that's all you could initiate treatment of a psychotherapy of whatever need you have a family therapy appointment.
32:25
But you're also there, working with peers, and if you need additional testing, say, medical testing, laboratory exam, imaging, anything like that can be done in this type of a facility, are coordinated with this type of facility. So, that treatment would be initiated.
32:43
You could be observed for a period of time, you could be overnight.
32:47
Just like the med surg observation units, the length of stay we're looking at is no more than 48 hours.
32:53
We really need to tree, as you enter the next level of care, that care needs to be coordinated by warm handoff.
33:02
It could be a crisis residential program, where you're going to be staying a bit longer in a 24 hour a day supervised setting.
33:09
Could be into a partial hospital.
33:10
Where you actually are going home at night would be in an ILP where you're maybe going to work income into this 3 or 4 times a week or outpatient.
33:19
You still could go to a hospital, SAMHSA says that about 40 to 45% of people are still going to need psychiatric hospitalization, even if they go to a crisis save unit.
33:30
But the idea here is that the other 55 to 60% don't need that level of care.
33:36
And can get care that they need no less stigmatizing. A more comfortable, a more confidential space.
33:43
Next slide, please.
33:52
There's a couple of slides here that we probably skip through pretty quickly, because we've already gone over the distribution of services.
33:59
This one goes over some of the things that you've already seen. So we can move on to the next slide.
34:09
I think in an effort to preserve time, I will skip over some of these pretty quickly, but this one is really important, because now I'm moving into talking about another alternative way of being able to improve access.
34:23
We know that about 80%, arguably between 75 and 80%, 85% of primary care doctors prescriptions for antidepressant medications are made by primary care doctors.
34:36
We know that the mental health and behavioral health workforce is not enough, not adequate for our population.
34:45
So the two teams really need to ally together.
34:49
And that's where collaborative care can be a really significant value going forward.
35:06
So this is the business case.
35:08
We're not sure how expensive behavioral health is, but how important it is to treat the entire person, not just their behavioral health needs or their medical needs, but to treat them all.
35:21
It's been mentioned previously that people with schizophrenia, anywhere, from 25, 25 to 28 years earlier than an aged man population without schizophrenia.
35:31
It's really important to take care of them, as well as people with depression, all the other mental illnesses that can occur, and substance use disorder.
35:42
We also know that the medical costs for treating people with chronic medical illness, as well as mental health illnesses are 2 to 3 times higher than those for treating people with conditions.
35:53
That is just one or the other, And also, the majority of protected savings from integrated care are associated with facility hospitals in emergency department utilization.
36:05
Integrated care is an important term, because there's multiple forms of integrated care. We have chosen to move towards the collaborative care model.
36:13
That doesn't mean these.
36:14
The other models are not effective and helpful, but collaborative care has the most data to support an evidence base, and that's where we have focused our energy.
36:23
Next slide, please.
36:29
Collaborative care has a little different team kind of orientation.
36:33
And it's its population focus, because we screen everybody in the primary care practices and identify people with primarily anxiety and depression.
36:42
But we're also looking at pediatrics populations, substance use disorder populations, populations of people with severe mental illness.
36:51
And it can be also we're looking at developing a high risk pregnancy perinatal program to be able to use this.
36:59
It's measurement, guided, PHQ nine, GAD seven.
37:03
Whatever the tool, whatever the population you are really screening for is what tool you can use.
37:08
And it has substantial evidence.
37:10
Base is over 90 evidence based trials that show collaborative care to be very effective. Next slide please.
37:20
The model is a little different than a regular practice in medicine.
37:24
Um, in many respects the medical field, the primary care field, has always been the primary provider, being kind of the captain of the ship.
37:36
And over time we have developed other things. We've developed other practice strategies using team medicine.
37:44
The family centered medical home was one of the first ones, so then Provider Delivered Care Management came along about 10, 12, 12, 12, 14 years ago.
37:53
And now, Collaborative Care is another descendant of those team medicine components.
38:00
But what we add is the psychiatric consultant and the behavioral health peer manager then coordinate what's going on with each case That has been screened into this program.
38:11
The Behavioral Health Case Manager is the primary liaison along with the primary care doctor to the patient.
38:17
The psychiatric consultant never sees the patient directly in this model.
38:23
They can, they can do a consultation. But that is a rarity.
38:27
Mostly it is that a psychiatric consultant is reviewing the cases, being able to advise the primary care provider as to what's the next step in this person's care.
38:38
Be it a different type of psychotherapy. Getting them into psychotherapy.
38:42
Being able to look at which medications might be appropriate, if the medications are ineffective, or they're having side effects, not to be able to change. Or to be able to add adjuvant medications to this. And when enough is enough in this setting.
38:56
And we really need a second tier or tertiary care intervention for that particular individual.
39:03
Another big piece of this is being able to help people, people's data really checked with, through this systematic case review tool, to keep tabs on the progress, to keep tabs on the labs that are going on, the interactions with their therapists, these sorts of things. Next slide, please.
39:31
So, a couple of testimonials here, and then I'll jump onto another couple of slides, and then we'll be able to have some questions.
39:39
But a patient testimonial, and this is a real patient, this isn't just an actor telling you all these things.
39:44
This was a family member who was enrolled in Collaborative Care.
39:49
She enrolled for about 2.5 months.
39:51
Used the tools every day, learned, during, really learned, during her calls with a behavioral health case manager, what she needed to know about the issues that she was dealing with.
40:03
And looks forward to her follow-up calls.
40:06
Um, the other one is it provided testimony?
40:10
And the biggest thing from this is that the collaborative care model made a huge difference in that particular provider's ability to manage their patients.
40:23
Mental health, in the long term, case manager, has been able to spend more time with me, has been able to provide vital information, and in helping to manage the patients, complex, social and mental health outcomes.
40:36
In this model, they can also do, with the social determinants of health, being able to look at the logistics of getting people where they need to be coordinating with the other, other people that are touching them in the care modeling system, and families being able to coordinate with family members.
40:53
I go to a lot of regional medical directors meetings.
40:57
And what I hear back is that from the primary care doctors, especially, is that, no, we're 75, 85% of us are burned out.
41:06
You know, many times, colleagues of mine from working in the hospitals say, I really don't want to be a Dr.anymore. I wanna, I wanna go be a carpenter. I want to do something else.
41:16
After a year in this program, I get the feedback.
41:20
Hey, I love my job, I love being a doctor, my patients get better.
41:24
I want to go to work every day, again, so much different.
41:28
And we can't afford as a society to let any Dr.just leave medicine because they're burned
out.
41:34
We have to take care of them, to be able to move forward. And I say, doctors in a very generic term.
41:39
Any healthcare provider at any level of care. Next slide, please.
41:55
So, in Michigan, we've really done a very aggressive program to be able to pull together and train providers.
42:04
We have been able to train 180 practices in the last 2.5 years.
42:09
We had put away some practice transformation funds that were available for us to be
able to do this and after making the case to our senior administration.
42:17
And they very heartily grabbed this and said, this is a great model to move forward with.
42:23
And it has been very helpful in backing this program.
42:28
84 have been added in 20 21. We develop a pediatric module for our training programs, and we've partnered with a large mister mid-western University.
42:39
And also A Clinical Innovations program on the west side of the state.
42:45
So we have a distribution, uh, using the same curriculum that we all developed together. The ability to train people in different parts of the state to be able to do this.
42:56
The pediatrics practices asked for us to develop this module.
43:01
And so we put this together, and we've trained up 20, they're really working quite well.
43:06
These are practices, and practices aren't just one doc or one nurse practitioner, or one Clinical Nurse Specialist or PA.
43:14
They're a bunch.
43:15
So we have 600 practitioners that we've actually trained and 800 practice practice should be practitioners', not practices, um, receiving the value based reimbursement that we offer to get people in the center to do this kind of work?
43:32
Um, we're also launching a co care designation program to be able to then have our members and case managers be able to find these programs much more quickly than us knowing where they are.
43:46
Next slide, please.
43:48
I think that brings us to probably questions.
43:53
Help, our pediatric adolescent model.
43:56
This is the adolescent model. It really does look at the difference with adolescents and kids.
44:03
We've driven this down, to about a 10 year old, is probably the earliest age group we want to try to manage in a primary care setting with these kinds of needs.
44:13
But the additional components of that.
44:21
Practice is looking at community based services, therapy, therapists, medical, being able to coordinate with health coaches and community health workers, peer supports, to be able to really help all of that system work together. And, consequently, it takes more time for the behavioral health care manager to be able to manage these cases. And, their caseload can't be quite as high.
44:46
But the additional members, as you see on the right there, are the Parents, schools, therapists, and other community resources.
44:52
It can be extremely helpful.
44:55
And we can move the last slide.
45:04
So, the key takeaways here, is the crisis services can really offer an offer specialized specific here, being able to decrease stigma, because you're going to not necessarily ER in a very uncommon potential place.
45:17
But being able to have a confidential place, that's not necessarily associated directly with the hospital, although they can be, they can be on the hospital campus.
45:27
It's a more comfortable setting, it's safer, integrator schema thing, and can be able to utilize the acute care, hospital setting, for people that are having other severe, life-threatening needs, such as a heart attack or stroke.
45:42
It's not to say people with behavioral health conditions don't have those also, They do and they need to be in the ER also.
45:49
But for people that don't have those immediate needs, the crisis services really can be an additional adjunct to an alternative path. And collaborative care really increases access.
46:00
In my practice, I panelized at about 600, 800 patients, as many patients as I could take care of effectively.
46:09
In this practice, I've talked with other people that have been doing this and other big centers.
46:15
We're thinking that a psychiatrist can be able to have psychiatric influence and the care of roughly 2500 patients.
46:23
So that multiplier of being able to work as a team, with primary care, psychiatry, together, being able to really work on taking care of individuals.
46:33
With a trusted provider that the individuals have, they have the trust of their primary care doctor, less stigmatizing. They don't know nobody from the outside knows if you're gonna get treated for a cold or, or for your depression.
46:46
So that really prevents that issue of stigma in general.
46:53
So with that, I will open it up to questions, and, again, thank you for your time for listening today.
47:01
Thank you so much. Dr. Beecroft. We would like to use the remaining time to engage in our Q and A session and ask our panelists to come off mute and back on video. And our audience can continue to submit questions via the Q&A.
47:17
I'm gonna start with a question for Dr.Bellamy.
47:23
We had an audience question about, could you touch, could you describe the tool that you use to rate changes with regards to the eight dimensions of wellness?
47:37
Hi. Thank you so much for that question.
47:40
And I can share with you our, our eight inches and wellness measure, but it covers all aspects of those. eight dimensions really engages with the data. to help them figure out, you know, whether they are meeting those eight dimensions. That can be used as an instrument, as well as a tool that can guide someone working with, with a person around us. eight dimensions. But I would be more than happy to share that with you.
48:19
Great. Thank you.
48:21
Um, next question for it.
48:25
Dr. Duckworth, you had mentioned some teen subpart groups and Dr.Beecroft had talked a lot about their adolescent care model. Could either of you talk a little bit more about caregivers and support for parents of teens struggling with mental health issues and specifically, does NAMI have a support group that people could access?
48:51
So NAMI has 650 affiliates across America, right? So everywhere you are, there's a program.
49:00
There are multiple programs in Michigan, and there's multiple programs near New Haven. Kathryn, where are you today?
49:06
Virginia NAMI Northern Virginia is a powerhouse, I live in Boston.
49:14
There's a comedy of NAMI resources, so each individual affiliate has its own capacity.
49:20
So you have family to family, which is adults, typically, who are parents of adult children, who have serious mental health conditions.
49:30
There's a program called NAMI Basics, which is for parents of younger children.
49:36
There are peer-to-peer programs, so I guess what I would say is start by contacting your local known, find out what support programs they're up and running.
49:47
In Bucks County, they run on it and 50 programs a month, and I'm not making that up.
49:53
I interviewed one of the leaders in County, Pennsylvania, North, North Philadelphia, That's what he told me. It's incredible.
50:03
So, these programs are all free, They're all with people like you, same or similar developmental stages.
50:09
Now, in college, there's NAMI On Campus, which is the largest program at America's favorite basketball university. I'll leave it at the biggest program, the Blue Devil University. So, that is something for younger people directly. There's also a place called Active Minds, which is a non-profit, which is directly devoted to youth mental health. So I think the place to start is contact your local NAMI, see what they're offering.
50:42
Great. Thank you for that question.
50:43
They do excellent work and are behavioral health care managers internally, add them on speed dial and the other community resources.
50:53
But we've also done some specialized services, Grand Rapids, to be able to help support community support groups. And that sort of thing.
51:04
Great. Thank you.
51:06
We have several questions from audience members and comments on the shortages that we're facing that we've been discussing today. Can any of our speakers talk about what you see as some of the most promising strategies or policy changes that can help change requirements and easy access to different types of mental health practitioners?
51:32
So, it takes eight years to make a social worker in eight weeks to generate a demand crisis, right?
51:37
So, the workforce is nowhere near what we need at this point. The Collaborative Care is a way to deploy psychiatrists, smarter, so they can care, take care of thousands, instead of dozens of patients.
51:52
There are loan repayment models that are engaged, but I don't find them to be nearly as comprehensive enough.
51:59
Technology is one potential avenue.
52:03
So telehealth doesn't create people, but it may improve efficiency for people in terms of getting health.
52:22
There's now 20,000 apps in this completely unregulated space with rare exceptions.
52:28
And so what do you think about that? Is that a supplement?
52:32
Is that a replacement? Each individual story is different, but there's no question.
52:37
Mental health needs more people. It needs more diverse individuals. So we have to create the conditions that people want to do this work.
52:45
It isn't easy. We have to pay for it so that you can have a viable career paying off your student loans.
52:52
Right? So I would say collaborative care is the best answer. Dr.Beecroft developed that very well. Technology apps, technology resources are a second thing to consider. And the third thing is we have to help mental health practitioners with their students.
53:12
I would agree with all of those things.
53:14
You know, we've found some disparities in different counties in Michigan that the federal level of reimbursement for student loans is different than the local level.
53:27
And these individuals get stuck in between, and they end up not getting their loans
repaid.
53:32
So we have to figure out that on a regular basis and coordinate that loan repayment can be for everybody when they do the work with a non-profit.
53:41
You know you've got that program, multiple different programs, to make it easy, push the easy button here. We have to make it easier.
53:51
Yeah, I would agree with everyone on everything that's been said as well in terms of loan repayment and incentives, as well as telehealth approaches. And, again, to continue to fund and support peer support initiatives.
54:07
I also think that we should move toward, you know, we were doing well at getting a crisis stabilization, but also adding peer respite And peer respite best run by people with lived expertise would be very then the test. So offering other options for people. And in terms of access, I think, you know, for those who are not accessing through traditional ways, I think we should also look at more street psychiatry initiatives and really doing more outreach to get people out there and where people are in the community.
54:46
two, to follow up questions to that, one for Dr.Duckworth mentioned this proliferation of mental health apps and technology. And, you know, how do we help people understand what additional research as needed, to unlock the potential for that to help people?
55:08
Um, yeah, so the American Psychiatric Association has something on their website to help you evaluate mental health that looks at privacy, data sharing.
55:21
What might it offer you?
55:23
And, you know, some of these apps, unfortunately, are not attentive to things like privacy and data sharing, right? So, you have to think this all through.
55:33
Basically, is, Look at this tool and figure out what it is you think you need.
55:42
Many people download apps, but don't engage with them.
55:46
So, the key is to find something that will work for you. What you will find compelling downloading an app is not the same as benefiting from the use of an app.
55:56
So, there's plenty of companies working in this space. Very few of them are FDA approved.
56:01
It's a tremendous leap to do that, but the APA is the American Psychiatric Association Technology Center, just it'll come right up if you Google it and just evaluate, you know, how you think about these 20,000 apps that are out there, because there might be a one that can help you.
56:18
But you should know what the limitations are, because it is the Wild West. Kathryn.
56:25
Dr. Bellamy, to one of your comments, how do we meaningfully integrate people with lived experience and that design of policies and programs?
56:37
First of all, it's about believing that it's important. And so, and I think that's really key, that, you know, we look at other countries, like the UK. And Canada, where Lived experiences. All of the different initiatives.
56:51
And it takes funding for programs, as well as for research, and so many people, and Bob, and co design efforts, people living with, as well as those family members as well, at the table discussing these issues. Designing the research, and being a part of that, The analysis of the research. And also, part of the implementation, we gotta do more than, just next to it, We really need the Center, the embankment, and get people involved in doing the work participation.
57:33
We've talked a little bit today, too, about stigma and are we at a tipping point of overcoming stigma? We've seen some strides coming through the pandemic. What barriers remain, and what are some effective interventions to decrease stigma, to increase access? And ask?
57:54
You know, part of that to the Dr.Duckworth mentioned, the crisis phone line, How can we, know, how can, you know, folks on the meeting today, how, how promote that line, and just continue this conversation on mental health and not lose sight of that?
58:10
So shame prejudice and discrimination is how I think about I'm not really a big fan of the term stigma, to get anything except the potential for another barrier. And I think you've seen a transformation in attitudes towards mental health.
58:25
The supply demand mismatch is one evidence of that. Try to find a therapist. Now, it is really not easy. More people are seeking help than ever.
58:35
That does not mean the problem is solved, and it does not mean it is happening evenly in all communities.
58:40
But one of the reasons I decided to actually energize real people through the book was to expressly get to that, Instead of what others do, which is make composite fake people.
58:50
I don't think that was useful.
58:53
The reason is to protect the person's privacy if you think there's something to be ashamed of, so I invited people who want to tell their story, to tell their actual story.
59:01
They're actually got people, it's not a fake person named Tom Smith from Ann Arbor, Michigan. There's a man named Tom Smith.
59:06
He lives in Ann Arbor, Michigan. He's living with bipolar disorder, and he's trying to figure it out, So I think this is a little small step.
59:14
NAMI has tried to make people tell their story, both in all our multiple programs, and in our little book.
59:24
Thank you for that. We are out of time. We have some additional questions for our speakers who are willing to take that. We can share them with them directly for follow up, but do you want to be cognizant of the time, and thank our excellent panelists, speakers for being with us and sharing your work and perspectives. And we will be making a recording of this event available, as well as slides. Thank you to our audience for joining our discussion and for your questions.
59:56
Your feedback, your feedback is important to us, You can take a moment to complete a brief survey that will open on your screen after the event. A lot of great resources have been mentioned today. We also have some resources available on our website, including every cent infographic on mental health care and solutions. So thank you all again for joining us today for this important conversation.
1:00:23
Thank you for your time.
Presentations

Ken Duckworth, MD
National Alliance on Mental Illness

Chyrell Bellamy, MSW, PhD
Yale School of Medicine

William Beecroft, MD
Blue Cross and Blue Shield of Michigan
More Related Content
See More on: Behavioral Health