Webinar
The State of Oral Health: Increasing Access & Reducing Disparities
Time & Location
An estimated 80 million Americans currently lack access to dental care. As oral health is essential to the overall health and well-being of an individual, the high volume of those without access can have potentially devastating health consequences such as an increased risk of developing cardiovascular disease, respiratory disease, chronic diseases, diabetes, and adverse pregnancy outcomes. Three main barriers to accessing dental care include coverage, provider shortages, and cultural barriers to oral health. In this webinar, we heard from leaders in the field of oral health who are working to reduce disparities in access to and quality of care.
Speakers discussed:
- Federal initiatives to reduce health disparities and advance oral health equity, while furthering oral health in pediatric populations
- A health plan foundation’s investment, in collaboration with the Duke Endowment, to improve oral health in the Carolinas, including in rural communities and school-based programs
- Interprofessional approaches to integrate oral health into education and care delivery models
0:05
Good afternoon, everyone, and welcome to today's webinar.
0:09
Before we get started, I would like to go over a few items, so you know how to participate in today's event.
0:17
If you've joined the presentation listening using your computer's speaker system by default, and you would prefer to join over the telephone, just select telephone in the audio pane, and the dial in information will be displayed.
0:32
You will have the opportunity to submit text questions to today's presenter, by typing your questions into the questions pane of the control panel on the right-hand side of the screen.
0:46
You may submit questions at any time during the presentation.
0:50
We will collect these, and try to address as many as possible, during the Q and A session at the end of today's presentation.
0:59
I would now like to introduce Kathryn Santoro, who will be moderating today's webinar.
1:07
Good afternoon. I'm Kathryn Santoro, Director of Programming at the National Institute for Health Care Management Foundation. On behalf of NIHCM, thank you for joining us today for this important discussion on oral health and disparities.
1:22
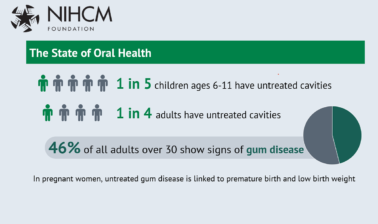
One in five children ages 6 to 11, and one in four adults have untreated cavities.
1:28
Additionally, 46% of all adults, over 30, show signs of gum disease.
1:35
Poor oral health can have a tremendous impact on the rest of the body.
1:39
Untreated gum disease increases the risk and severity of chronic illness, including heart disease, diabetes, and stroke.
1:48
The importance of oral health, as well documented, yet substantial barriers exist to achieving oral health.
1:56
Many Americans live, and dental shortage areas don't have access to fluoridated tap water, or encounter cost barriers to accessing oral health care.
2:06
The pandemic has exacerbated many challenges around accessing oral health care, and many Americans, delayed oral health care during the past 19 months.
2:17
Today, we'll hear from a prestigious panel of experts to learn more about the need for oral health and strategies to address the disparities around oral health care.
2:27
Before we hear from them, I want to thank NIHCM President and CEO, Nancy Chocolatey, and the NIHCM team who helped to convene today's event.
2:36
You can find full biographies for all of our speakers along with today's agenda and copies of slides on our website.
2:43
We also invite you to join us in the conversation today on Twitter using the hashtag oral Health.
2:50
I am now pleased to introduce our first speaker, Dr. Natalia Chalmers. Dr.Chalmers is the first ever Chief Dental Officer with the Office of the Administrator at the Centers for Medicare and Medicaid Services.
3:04
She's a board certified pediatric dentist, oral health policy expert, and public health advocate, and she brings more than 20 years of clinical, research, industry, and regulatory experience to her role.
3:18
We're so honored to have her with us today to share CMS's vision for oral Health. Dr. Chalmers?
3:27
Thank you, Kathryn, for this kind introduction. It is truly an honor to join you with my fellow panelists and reflect on how we can address oral health disparities in access to care. Next slide.
3:46
I started my presentation, oral health, and evidence, and data driven approach, to achieve better health, equity, and fiscal responsibility. And I hope you'll all join me, explore the evidence around the importance of oral health. Next slide, please.
4:08
I would like to take a moment to share the CMS vision for the future.
4:14
Our administrator, to keep the books mature, has developed an inspiring vision that CMS will serve the public.
4:26
That CMS will serve the public as a trusted partner dedicated to advancing health equity, expanding coverage in improving health outcomes. The first pillar to support this vision is that we will advance health equity by addressing the health disparities that underlie our healthcare system.
4:45
The second is to build on the Affordable Care Act and expand access to quality, affordable health coverage, and care.
4:55
The third one is to engage our partners and the communities we serve throughout the policymaking and implementation process.
5:04
The fourth one is to drive innovation to tackle our health care system challenges and promote value based person centered care. We'd like to refer you to the CMMI website to see their vision and white paper on The Future of Innovation in CMS.
5:23
The fifth pillar has to do with being stewards for these programs, and so we will protect our program sustainability for future generations by serving as responsible stewards of the public funds.
5:38
And last, but not least, is to foster a positive and inclusive workplace and workforce, and promote excellence in all aspects of our operations. Next slide, please.
5:49
I think this slide says it all. The Surgeon General was very clear when he said, You are not healthy without good oral health. I would like us to keep that in mind as we move forward, trying to address disparities in our healthcare system. Next slide, please.
6:08
three things I hope you come away with, the first one is that oral health is about equity, and we will explore this further.
6:15
It's also about fiscal responsibility. And when oral health needs are not addressed early, we end up encountering costs into healthcare systems that are avoidable.
6:25
And last, but not least, oral health is about inflammation.
6:29
And if we want to improve clinical outcomes, we need to address unmet oral health needs. Next slide, please.
6:40
This is a trend of the prevalence of untreated tooth decay in primary teeth among children.
6:46
ages 2 to 5 is a pediatric dentist treating many of these children.
6:51
And they, some of them pre co-operated in require additional support so that the treatment can be performed, but we have amazing strategies in prevention that work really well, and have to be employed to address these disparities. See the gray bars, you know, this is the level of racial disparities that exist, where 15% of black non hispanic children have untreated tooth decay compared to about 7% in white, non hispanic children.
7:23
And also, you can appreciate the income disparities on the right, 17 for children living below the 100% of federal poverty level, compared to only 6% of children living at over 200% of the federal poverty level.
7:38
Next slide, please.
7:39
These disparities persist throughout adulthood, and you heard in initial stats on the prevalence of through doing this. But here, we see that broken down by age from 30 to 65.
7:52
And they can note that 65 years or older people in the black, the blue bar, 66% of them have Thank you.
8:03
Can appreciate the racial disparities that exist with food in places where non hispanic blacks have rates of about 60% of food intake as compared to 40, with non hispanic whites.
8:19
And as with the children, Indian treated cavities, again, you see adults in poverty have a tribalism. Food intake is around 60% compared to only 30, those who live 400% above the federal poverty level. Next slide, please.
8:37
And Death continues, as people age, and in adults, 65 years or over. Complete tooth loss, or also known as evangelism increases with age.
8:51
There are no significant differences between men and women, but the racial disparities are quite clear.
8:57
30% with non hispanic blacks experiencing ... compared to 16% of non hispanic non hispanic whites, or 15% with Hispanic.
9:08
It is encouraging to know that there has been an overall reduction in total prevalence of ..., but we need to address the health disparities. Next slide, please.
9:23
This is a really clear picture of the progress we have made in access to dental services for children in poverty. It would appreciate the change over the last 16 years, and increase access to care for children living below the federal poverty level, But notice how, in the middle, there is very little change for both adult groups.
9:46
And, on the right, adults who live below the Federal Poverty Guidelines have seen no improvement in access to dental services while they have been increasing access to care for adults, living above the 400% of the federal poverty.
10:03
Next slide, please.
10:06
I think one of the primary challenges for oral health, and now integration with the healthcare system, is that these clinical scenarios are perceived very differently by patients and providers.
10:19
So on the right, you see a non healing ulcer over the owner aspect of the left forearm. And clearly, it's, you know, inflamed and swollen, and losing. And on the left, you see someone who has chronic periodontal disease.
10:35
What goes on under-appreciated is that the total inflammatory surface around the teeth on the picture on the left would result in an ulcer of that size.
10:47
And many times that goes unnoticed. So you would never imagine someone presenting with this level of inflammation. And a clinician says, oh, let's take care of your diabetes. Right. And this has been the challenge to commute.
11:01
How do you communicate these two conditions for the body, identical? The body doesn't know where the inflammation started, it reacts the same way.
11:10
Next slide.
11:16
Don't do these diseases are associated with many inflammatory comorbidities, such as cardiovascular disease, type two diabetes, rheumatoid arthritis, inflammatory bowel disease, Alzheimer's, non alcoholic, fatty liver disease, and cancers.
11:33
And the way the ...
11:35
Packages disseminate through the blood, so that's called vector E Mia, all through the oral pharyngeal and oral digestive pathway, resulting in increased inflammation and exacerbation of these conditions.
11:50
And if you're in healthcare, you know that the majority of our resources are addressed trying to address these conditions. And yet, we don't address the fear. you don't have the disease. That's fueling the inflammation.
12:05
Next slide, please.
12:08
Or oral health has also impacts beyond health care.
12:12
If you have oral health, it will be an obstacle to employment.
12:17
It is the number one reason why children miss school days, and also it impacts their performance.
12:24
Oral health is linked to substance use disorder, and that connection is actually bidirectional, because many substances negatively impact oral health.
12:34
Oral health is also an independent predictor of all cause mortality.
12:41
So just to keep that in mind, when we talk about the impact of poor oral health on the well-being of our beneficiaries. Next slide, please.
12:51
It is important to reflect where our beneficiaries present with oral health care needs.
12:57
On the left, you see the dental delivery system with many well established patients who have access to care.
13:04
And the occasional patient that shows up to the front door as a dental office only when they have a problem.
13:13
When oral health care needs and ought not be addressed, many of them exacerbate.
13:18
And patients then present to the Emergency department with oral health care needs. Again, some of them will show up with one emergency, but many will return.
13:27
When the condition is so poor, some of them have to be admitted into the inpatient admissions, right. And now, we're moving from the fiscal point of view from a visit. The Emergency Department on average can cost $900 to an inpatient cause that could range from 10, 20, 30, depending on the state.
13:46
The ambulatory surgery point of care is really important, one, for very young children, as pointed out in the beginning, but also for children and adults with special healthcare needs.
13:57
Urgent clinics are also a point of care, and you will hear later in the program how schools serve as an incredible opportunity for access to health care for children.
14:08
We have to talk about the health information technology divide, the lack of diagnostic coding between the two systems, and how we need to integrate and coordinate care better. Next slide, please.
14:22
For children enrolled in Medicaid, dental services are essential and provided. However, you can see here that the percentage of Medicaid eligible children, 1 to 20 who receive a preventive dental service in 2019 varies dramatically by State, and that is to say, it's a benefit, and coverage alone is only the first step, and there are many barriers that need to be overcome to ensure access to care. Next slide, please.
14:52
one incredibly useful opportunity is to understand dental and medical utilization and seek opportunities for collaboration.
15:04
On this slide, you see the total and broken down by the age of the beneficiary, utilization of dental services, and medical services.
15:14
First, what is really clear is that the overall utilization is very similar, but there are two different trends, the dental falling, these U shape utilization with very low in the early ages.
15:26
Where medical, using this slope utilization.
15:30
And so it presents an unique opportunity to intervene early on, and, and collaborate with our medical colleagues to advance oral health services, and in a non dental setting. Next slide, please.
15:45
From the Early and Periodic Screening Diagnostic and Treatment report that states provide, for children 1 to 2, you can see this is the States geographic variation of oral health services by a non dentist provider.
16:00
Again, you can appreciate the differences between the States. And the States that are hatch over are now engaged with the Centers for Medicaid and chip Services in a Learning collaborative of how to advance the prevention and reduce childhood caries. more. Information about The collaborative is available on medicaid dot gov.
16:21
Next slide, please.
16:24
It is important to understand dental expenditure, of the healthcare system in the broader healthcare expenditure.
16:32
And, you will see that that accounts for about 4% of $124 billion. But, note, these circles, the two circles in red, right? This is, for physician services, we have out of pocket spending, about 9% for dental.
16:47
It's 40%, and the other piece that many of you will be familiar with, the Medicare space for physician services, is about 23%, and for dental, it's zero. Next slide, please.
17:04
Thinking about the priorities and spending in the healthcare system, the striking differences between the public, private, and out of pockets systems, if you will. We spend the most on diabetes, in the public space, about $55 billion every year, and I already highlighted cow oral health is connected to that.
17:23
But you see, oral health, spending ranks 34th in 47, in the private insurance business, or the private delivery system. Oral health services, rank 11 and 12, and diabetes is now number five. But out of pocket spending, oral health in, well, dental services are number one and number two.
17:43
Next slide, please.
17:47
For Medicare beneficiaries, this is from a survey that's conducted by the Centers for Medicare and Medicaid Services.
17:55
We understand their expenditures and also out of pocket, and, again, if you see, they spend about $4000 on prescription drugs, about $3000 on physician services, and so forth.
18:09
And when you compare, yes, when you look at the out of pocket proportion, you appreciate the dental services have the highest out of pocket rate. Next slide.
18:23
And so, one opportunity that is really clear is to address the emergency department visits for dental needs, because they are about equity. They have a huge financial impact.
18:38
If they contribute to many re-admissions, they're linked to mortality. And last but not least, too many opioids and antibiotic prescribing.
18:47
Next slide, please.
18:52
The chart on the right clearly indicates who is the primary pair for these conditions. In 2014, Medicaid became the primary payer for emergency department visits for dental conditions among adults.
19:08
And you will see on the chart on the left, the age group most impacted by this is ages between 19 and 30 for these two age groups together.
19:18
Why is this important? Because, next slide, please.
19:23
Dental pain is one of the number one reasons why opioids are prescribed to adults that present to the Emergency department.
19:31
Here, you see an unsettling trend for over 10 years where dental pain and kidney stones are sort of playing in debt. And dental pain is still one of the top reasons for opioid prescribing. So it's not only impacting the overall health but it's fueling the opioid epidemic.
19:51
Next slide, please.
19:54
And so, the Centers for Medicaid and chip Services released last week, a comprehensive study on the Medicaid Adult Beneficiaries Emergency Department visits for non ... dental conditions.
20:08
That study is available on our site and will be shared with the materials after the webinar. Key findings of the report examine the emergency department visits for non traumatic dental conditions for Medicaid, non dual adults.
20:28
And in 20 18, there were approximately 663,000 such emergency visits, and approximately 7500 of them resulted in an inpatient admission. And we report this by state, both the inpatient admission, as well as the emergency department visit.
20:48
So, next slide.
20:50
So looking ahead, what are some of the challenges and opportunities we have had? We have been in the middle of a pandemic for 20 months or so.
21:02
The goal here is not something that will leave us quickly. Many children, so covered. one thing we refer to in the beginning, as impact is access to many services, But compared to ...
21:16
level, we're still about 30% below where we were, so that is a huge.
21:22
If you will, accumulating a burden that we will have to face sooner or later. You'll see these by the recent reports on medicaid dot gov.
21:32
We have to think about system capacity. They have innovative approaches, such as telehealth, that could help us address unmet needs. What is the role of school based programs? And you'll hear from fellow panelists of some innovative ideas.
21:48
Thank you for your attention, and I look forward to your questions during the question and answer session.
21:55
Thank you so much, doctor Traumas for highlighting some of the key challenges and opportunities for reducing disparities. And we look forward to continued conversation and questions with you at the end of presentations next. We will hear from Katie I's Vice President Program and Strategy at Blue Cross and Blue Shield of North Carolina Foundation.
22:17
Katie works closely with the program team, grantees and others to support communities in North Carolina, to look upstream and transform practice and culture to dramatically improve health. In addition, she provides leadership for the Foundation's focus on oral health.
22:33
We're so grateful. She is with us today to share her team's efforts on partnerships to support oral health and North Carolina.
22:41
Katie?
22:44
Thank you, and appreciate both of you for that great setup.
22:48
I will take a little bit of a different approach. As I said, as Kathryn said, we're a statewide funder.
22:54
We're focused on systems change, and I was asked specifically to share about our school based oral health work, but I also want to contextualize that to some degree. And I'll start with the assumption that some in the audience are looking for strategies to increase access to care locally, or at a larger scale.
23:11
So, next slide, I'll appreciate the sort of orientation for the science and data, and bring it a little bit more qualitative with this quote.
23:21
That's really an observation like this that highlights what moral challenges that was alluded to. How much inequity is, is baked into the way we frame up and address oral health.
23:32
And in particular, the notion of the slow motion catastrophe really resonates with me on these poor oral health, come, the oral health outcomes. The ..., opioid prescription ED visit, the doctor ...
23:47
described, are really part of a longer trajectory of chronic disease.
23:52
And, you know, the lay person, which is what I am, have been socialized to think about oral health really Episodically, but it's a chronic disease, And it's our belief that the school based model can really be a part of acknowledging and addressing that.
24:07
Based on their care model, they meet children and families where they are and create an environment where they can take a much more patient centered approach and preventive approach to oral health care.
24:22
A little bit about North Carolina, and the data that doctor Tremwel shared shows us. We're not unique here, but we do see significant equity.
24:30
We know that preventive care is cost effective, but it's not accessible to those who are at the highest risk in insignificant parts of our state.
24:40
And that's because of cost, and access barriers, including workforce.
24:45
And so those conditions really have led us as a foundation to focus on workforce policy and financing, in our strategies around oral health. And I hope that by the end of this sort of talk, you'll, you'll share some of the understanding about how school based work is a part of that.
25:05
Moving on to the emerging context, slide around the coven.
25:11
The questions I thought submitted with registrations really thought about the interests and the impact of covert, and, again, doctor Thomas mentioned some of it, but generally, it's really fast track some innovations here in our state, and lots of interests in tele dentistry and Minimally Invasive Care.
25:30
It's created some new incentive for the dental profession to move towards prevention centric approaches.
25:37
And those are some of the same approaches that really preserve structure and contribute to value, and are really easily applied in the school based setting.
25:47
I'll just also add, I don't think this was mentioned, it really contributed to staffing shortages and we see that in the safety net in private practice.
25:56
And then the piece around foregone care. Certainly, in schools, we are beginning to see the effects of that. What time of disease progression happened in the last 18 months of relative isolation, when people weren't seeking care?
26:12
And we're also seeing supply chain issues impacting some of our school based programs, as well.
26:17
But the bottom line is really that the impact on the oral health system during the pandemic has been disrupted. We think there will be greater inequities, and worse oral health, and that some of that disruption could lead to innovation that has an important impact.
26:33
So on the next slide, I'll sort of move into our school based oral health work, and the model that we're supporting.
26:40
And this is 1 of 3 strategies that we use in our oral health focus at the Foundation. Really supporting the spread of these models across the state.
26:49
I'll say it is not the first approach we used when we started out funding oral health about 10 years ago, but really builds on our experience and learning over time, and the relationships and momentum that has been built in the state.
27:04
We are trying to do this at a pretty significant scale, and we have three funders in two states and two dental schools, in addition to all of the clinics and communities involved, but it's something that can be replicated at a local level, and really sort of builds on our experience that these programs have to be sustainable and must be dental homes. But, again, no reason it can't be done at a smaller scale.
27:30
And so, you'll see on that slide, the program goals we have, it really is about creating access to oral health care in a setting where children spend much of their time in the school, and we believe this has the potential to address many of the barriers to oral health access that exist in communities today.
27:49
The partnership and you'll see at the Duke Endowment, the Blue Cross Blue Shield of South Carolina Foundation, and our Blue Cross Blue Shield of North Carolina Foundation. We've been working on this together since 2019.
28:01
Um, and just technically, it starts with a six month Readiness grant, that we actually have our grant opportunity open right now, for a fourth cohort of these grantees.
28:15
Those are $65,000.
28:17
And then we go into a couple of years of implementation funding that support sort of the startup costs of these new programs.
28:25
We provide technical assistance throughout the initiative.
28:29
And we've sort of created the opportunity to fund up to 10 programs a year from both dates, and the programs really vary based on the community's needs and the assets there. But the model really requires kids being seen in schools to have a dental home that will ensure that their treatment needs are addressed, either by a dentist who is visiting the school, or by a referral to a fixed site.
28:56
And that requires a lot of partnership between the school system, teachers, administrators, the clinic staff, the Navigators, who work with families, and then, as well as the families and kids themselves that are essential for making that work.
29:12
And, as I said, each implementation is different. But all of the programs emphasize prevention and less invasive care as part of their comprehensive care models, in part due to their setting and the opportunity to focus more so on prevention.
29:29
On the next slide, you can see the locations of the school served by the first three clinics, and each color represents a year with Orange being the first cohort of grantees.
29:40
And so those are the locations of the school. There's some coded pickup, as I said, related to supply chain, and, and whether schools are allowing sort of outside providers into the school setting this year. But this is sort of largely what we expect, we'll see when things settle.
29:58
They're all sorts of models. As I said, some of them are busses that pull up to a school and see the kids in the bar. Some of them, you know, a lot of them are portable equipment that gets brought into the school.
30:11
And this is not only about feeding these models, but it really also engages the organizational and political leaders, as well as the school leaders who want to do things differently in their communities. And they have really become champions for this work, and the policy changes that support it.
30:28
In terms of coverage, if you're familiar with the geography of North Carolina, you'll see we're in some rural areas, but perhaps not, not necessarily the ones where the access barriers are graded or the outcomes are the most challenging.
30:43
And so, in this fourth and fifth cohort that we're recruiting for now, we're going, we're doing some pre readiness coaching. And we identified 20 high priority counties where we really want to speed some of these programs over the course of the next few years.
31:01
On the next slide, you can see, the focus on PA has been significant, in part because we are doing this at scale.
31:09
And so it's led us to focus on all of the aspects of the planning that are required for success.
31:16
And it's a screenshot of an article from Maternal and Child Health that really focuses on the TA curriculum.
31:23
The grantees in these cohorts receive peer support from each other, which is really critical, and technical assistance, led by a team led by Amy Maarten, at the Medical University of South Carolina, and also supported by East Carolina University School of Dental Medicine.
31:41
And that technical assistance covers many topics, you know, starting with site selection, service scope, How to use electronic records in this environment, the different staffing model, how to develop partnership, billing, consent, and case management and navigation.
31:59
But I would say that, you know, a significant pieces, what the cohort learns from each other.
32:04
and the peer, you know, some of the stories I've heard from the site, now, where you want to install the electrical at the school.
32:11
So you can plug in your van or your bot, and warm it up before the school doors open.
32:16
Not parking your vehicle to unload your chairs and other equipment on the athletic field in the mud, or these are the real life lessons that peers bring to each other that really influence the success of a program on the ground level and have also proved invaluable.
32:35
On the next slide, you'll see a sort of deeper screenshot into the components of the technical assistance, And, again, you know, there's this expansion planning period for these grants.
32:47
And during that period, really focusing on a care management plan, a business plan, a community engagement plan for those.
32:57
So that will be successful in all domains and really achieve the impact and the sustainability.
33:04
That TA is offered by pre-recorded webinars, live Webinars, convening, and individual coaching for the grantees, so that they can apply what they're learning.
33:16
And then we've also built in this, a lot of peer connections so that people are visiting each other and the programs in the state post be what it is, what's happening on the ground and different sort of manifestations of the program.
33:30
And that networking among the safety net dentists and administrators has gotten a lot more robust over
time and gives a sort of common ground to innovate beyond the school based work as well.
33:41
On the next slide, I wish I could show you a video, but we've got a screenshot of doctor Francisco Rio through that Kinston Community Health Center, to sort of show what this looks like in action.
33:52
All of these sites really offer full scope care that can include a referral and navigation to a fixed site, and it's needed but by doctor Rios visits the school and does most of the services on site at the school math exam, radiographs planning varnished restorations. And most of the sites use silver diamine fluoride as well.
34:16
The care managers and navigators are a critical part of this work to liaise with the schools and families.
34:23
And yeah, you can really sort of see for misquote how much of a passion that has become in the clinic within our first cohort.
34:31
And they're working in 13 schools or a community health center, working in 13 schools in their county. And when they go out, they see about 25 students a day.
34:40
And they are working their way through the prevention, treatment, and referral as needed.
34:45
I mentioned that, you know, that sort of leads to other work and a school based center in the Mountain west.
34:52
I heard from one of their dentists recently.
34:54
During the course of their work in the school, they've also grown a lot at their fixed site. They went from one dentist and now they have more than three FTE dentists. They've added three ... to their clinic.
35:06
They've added nitrile.
35:08
They've put it in a mobile unit. They're increasing their sort of sealant first focus in the clinic.
35:15
And their use of silver diamine fluoride. And, of course, that's not all attributable to this work, but it reflects I think the leadership that these folks are bringing as well as the sort of desire to learn, innovate and expand their services.
35:30
Um, that really has served them well and in applying in, developing these programs and applying them elsewhere.
35:39
And I'll say it's a big success to know that most of these sites are using a recent rule change around public health hygienists in their school based settings. And North Carolina was until recently, one of only four states that really didn't allow hygienists to deliver any preventive services without a prior exam by a dentist.
36:01
That changed that to a limited degree in 20 20 and it was one of the really first substantive practices that changed in our State for more than a decade.
36:10
But many of these sites are, sort of, jumped immediately into using it.
36:14
So it really, sort of a connection to our policy work.
36:19
The grantees are contributing to advocacy for that policy change, but they're also providing experience and models that show what it is like, what it looks like on the ground when it's being used.
36:30
And that lowers the perceived barriers to others to see that model in action.
36:35
And so it really provides not only feedback loops to the future policy agenda, but reinforces any changes that we make in the policy environment as well.
36:46
And so, that'll lead on the next slide, into, sort of, the snapshot of our policy change strategy.
36:54
And just want to reinforce that strong connection between the school based programs and our strategies to advance payment and policy change.
37:03
So, we support a coalition working for that. And the schools really serve as a proving ground and a platform for scaling and helping to identify what other policy changes are needed.
37:14
Those new programs not only create the access point, but also a shared understanding among families, dentist, and hygienist, and advocate about what practices and policy changes are needed and how to work to reduce those barriers to care for them, and they become a part of that network of advocates.
37:35
And so, on the next slide, just some screenshots of different articles, publications that have come out recently. And, you know, I really appreciate the data that Dr. Chalmer shared, and we'll just underline that.
37:48
data has been really critical to this initiative as well.
37:53
Sort of both data transparency at the state level.
37:57
And we're, we're not yet at a point where we can see the impact of these programs reflected in our data, but I do hope that'll come.
38:05
But we do know that the data transparency among sites, and the data transparency, or use of data within the individual implementation, has really contributed to sort of growth and technical assistance.
38:19
And, coaching and changing applications at the Epic Clinic level. So, I'll just close with that learning from us around the importance of data and data transparency. And the fact that the school based programs are really not working in isolation from our policy focus work, but are an opportunity to build momentum and inform our larger change agenda.
38:42
Back to you, Kathryn.
38:45
Thank you, Katie, for sharing Blue Cross Blue Shield of North Carolina Foundation's Leadership on Oral Health, and these great efforts and takeaways for how we can improve access to care for school aged children. Next, we will hear from Anita, Professor and Associate Dean Emeritus at the University of Colorado Medical Center. She was a founding member of the National Interprofessional Initiative on Oral Health and now serves as executive director.
39:14
She brings over 30 years of research and education experience to this conversation, and we're so grateful. She can be with us today to share her expertise and perspectives.
39:29
Thank you, cancer, and I appreciate that introduction.
39:33
12 years after NIH was founded, we continue to play an essential role in a national effort to create systemic change by bridging historical, medical, and dental silence.
39:47
We began as a partnership between three foundations.
39:51
A philanthropic center, They created a case study and collective impact, engaging non traditional partners to integrate oral health, to activate change.
40:02
Capitalize on two emerging trends in a professional core competencies for collaborative practice and payment and practice reform designed to achieve the Triple Aim.
40:13
We consider how oral health is given its critical relationship to overall health.
40:19
The be the perfect exemplar for interprofessional education and integrated collaborative practice models to improve health equity and reduce disparities.
40:31
Our assumption was that workforce transformation is critical to accelerating change, and that patients would have better oral health if their primary care provider addressed some oral health needs during routine visits, including education, preventive care, and referrals.
40:48
Next slide.
40:53
So how did we get here in the US? As you've heard, patient care is typically fragmented.
40:58
Many of our patients see a physician regularly, and visit a dentist and this doesn't include the PA's nurses, and others who provide primary care.
41:08
What this slide does document is 108 million missed opportunities for primary health care providers to engage patients in preventive oral health care, education, screening for early identification of disease and referral to dental professionals.
41:26
The fragmentation of care doesn't just impact a provider's communication to the patient.
41:30
It also impacts the flow of information between providers related to their patients' oral health.
41:37
Next slide.
41:41
That there is a bidirectional relationship between oral health and systemic disease.
41:46
However, it is depicted on this slide.
41:48
Typically, there's little to no communication between our dental and medical care practitioner silos.
41:55
The flow of information about the diagnosis and treatment of a chronic disease, like diabetes, for example, is heavily reliant on the patient acting is going into it, which is not only burden on the patient, but also often an unreliable means of communicating critical health information.
42:14
Next slide.
42:16
Give them these issues.
42:18
We now recognize that in addition to fragmentation of care faces, access to dental care remains a significant barrier with 62 million individuals living in Health professional shortage areas, and two thirds of Medicare recipients lacking delacroix rich. So, where do they go? As you've heard, they end up in what I call the rabbit hole of our nation's emergency rooms, where providers are often unprepared to deal with their concerns.
42:45
This issue of insufficient dental health professionals to care for our population won't be resolved soon, So we need as a country to consider who else we could engage in prevention, because, unlike many aspects of normal aging, poor oral health can't be prevented.
43:03
Next slide.
43:06
In 2009 to address the systemic problems, NIH evolved as a consortium, thundered by health professionals and national organizations with a shared goal of eradicating dental disease.
43:18
Our assumption was that if we can integrate oral health into the education and professional coursework of providers, they want to enter the workforce ready and willing to partner with other health professionals to create a new standard of oral health in primary care.
43:34
We recognized that primary care prevention is critical, but providers also need to be ready to screen for oral health concerns in acute, chronic, and specialty care.
43:48
The NIH is a systems change initiative, and we provide that support to facilitate interprofessional agreement and alignment across health professions to ready an inter professional workforce for whole person care.
44:02
We work across Madison, PA's, nursing, dentistry, pharmacy, and social work.
44:07
Next slide.
44:09
Now, oral health isn't a new concept, and this graphic captures the opportunity for change. We see the progression of the field, and the growth of policy documents that over the past 20 years have been driving change across our healthcare system.
44:24
two of these documents have given a big lift to the oral health integration movement, versus a report on the integration of oral health in primary care practice, describing what we can do by defining a set of oral health core clinical competencies for non dental providers.
44:43
The interprofessional education collaboratives, core competencies for practice describes how to work together in a collaborative team based environment.
44:53
Next slide.
44:55
Change happened because we intentionally adopted three core strategies: We cultivated leaders, facilitated in her professional learning an agreement, and we created support tools and resources to build a shared understanding, knowledge and skills in oral health.
45:11
These strategies inspire a philosophy of collective impact, where we work across health professions and mutually supportive ways to create a movement that drives change, leveraging the unique capacities of each partner to maximize our impact. Next slide.
45:29
So I want to shift our attention, as I know you're interested in the tools and resources that are preparing our primary care workforce and others to integrate oral health.
45:38
The Exponential Growth Smiles for Life, the nation's most comprehensive and widely used oral health curriculum.
45:44
Now, there's over three million unique site visits, and 470,000 courses completed for credit.
45:50
However, anyone can use Smiles for Life without registering, and because educators can download module slides, elections, our numbers only recognize a percentage of them actually using the curriculum.
46:04
The endorsement of a health profession and over 20 professional organizations documents the widespread acceptance of the curriculum across health professions, as well as rec throwing, interprofessional agreement, and the need for shared ownership of oral health.
46:23
The endorsement of the health professions is supported also by the eight independent modules that extend across the Lifespan nigel's.
46:31
Log and track progress to a back end database, making it possible for many of these professionals to receive up to eight hours of continuing education, free continuing education.
46:42
And because it's profession neutral, these modules can be used by health centers and other facilities to educate our staff in a common curriculum, including specific instruction in team based interprofessional care.
46:54
New series of modules were recently adopted for community and frontline health workers, including a focus on the needs of pregnant women and older adults. Next slide, please.
47:06
While the Smiles for Life database tracks the spread of the curriculum, it doesn't help us understand how the curriculum might be impacting patient or practice outcomes.
47:15
In a recent survey, we asked users if someone was polite.
47:18
If it influences their activities by leading them to start an activity, perform it more regularly, or perform it better.
47:28
Providers across professions reported to us that Smiles for Life influenced many oral health activities, but
especially those that require more oral health knowledge, and I'd like to drill down on the next slide.
47:41
Referrals are something we routinely expect a direct care provider to do. Yet, even with that, we see that a third appeared to do this more regularly. And almost 40% felt they did this better.
47:53
In terms of anticipatory guidance, 60% said they felt they did this better. And almost 50% said they began applying for garnish as a result of the curriculum.
48:04
Next slide.
48:06
Almost 60% say that they do a better job of carrying out risk assessments with about the same number conducting a better oral exam.
48:13
With 50% filling, they do a better job of oral cancer screening.
48:17
In summary, we found that the curriculum chose to positively influence the practice of oral health across professions.
48:25
We also learned, however, that organizational factors may influence the uptake of oral health activities in primary care practice.
48:34
We're often faced with significant challenges when it comes time to integrate oral health and practice, due to the systemic ways that practices are organized. Next slide, please.
48:45
So I briefly want to mention our work, with Qualis Health, to create a White Paper and Oral Health Integration Framework that supports these practice transformations.
48:54
The framework describes five actions that primary care teams can take to promote and protect patient and rural health.
49:01
Ask about risk factors and symptoms, look for signs of oral health risk, or active disease, Decide and the Most Appropriate Response, Act to offer preventative interventions and referral for treatment, document to structured data, to support shared decision making and population management.
49:22
Also released an implementation guide, A toolkit reflecting our experience field testing, 19 diverse primary care practices, Use the framework.
49:33
The tool and the guide includes specific resources, the practices found helpful like referral agreement, patient engagement strategies, and EHR templates.
49:44
The tool allows settings to customize integration efforts based on the setting, staffing, and patient population.
49:51
Because we know that while policies and rules that govern our health care system are often national, our solutions must be local, responsive to these communities and populations that we serve, so that all patients can have care whenever and wherever they need it.
50:07
These tools are just two of the many examples that can be used to support oral health integration at the local level in education and practice, while at the same time pushing and transforming systemic levers for interprofessional practice and oral health integration.
50:23
Next slide.
50:26
In addition to tools and resources, we've intentionally invested in cultivating leaders in the PA and Nursing profession's.
50:33
This has resulted in systemic change integrating oral health into education and practice for those professions.
50:40
National studies now document that 96% reporting PA programs now integrate oral health.
50:48
Their graduates are three times more likely to integrate these skills in practice.
50:54
Our nursing home is created by researchers and strategies, foreign nations four point two million nurses for seeding transformation across primary, acute and chronic care settings. Next slide.
51:09
Our most recent strategy is to support online connect partner efforts.
51:14
... is a recognized thought leader from public and private policy organizations, payers, and health systems.
51:21
By way of example, our recent partnership with the Primary Care collaborative resulted in their publication highlighting a scope of today's integration efforts across the US. It's a great resource for those seeking examples of interprofessional initiatives that highlight collaboration between primary care and dental providers, including ... therapy.
51:43
Next slide.
51:45
The disruption that we're witnessing today provides a unique opportunity to think differently about the way we work together, collective impact has been foundational to accelerating change and to align it growing in a professional oral health field.
52:01
The change is never easy, especially when we don't have a shared concept of where we want to end up.
52:07
So, in this defining moment, integration is critical to our work, potentially transforming the way much of today's care would be delivered.
52:17
The bidirectional relationship between oral and other systemic diseases provides a strong rationale for integrating oral health and primary care.
52:26
However, policymakers and clinicians often use the terms, collaboration, co-location, and integration interchangeably, and inconsistently, to describe these varied approaches to practice.
52:40
Depending on the needs of specific communities, we know that all of these models have value.
52:45
But while we work to create a shared understanding of the terms to characterize that, the things that are taking place in practice, we're also exploring whether benchmarking degrees of collaborations can help us identify next steps or best practices to prepare our workforce and health systems to the backlog feature care that we face for the pandemic.
53:08
We advance a vision of transformed, Integrated Practice, where providers and patients view the operation as a single health system, treating the whole person using shared decision making, EHRs, and payment systems, An equitable system, or principles of prevention, whole person care, are applied to all patients, not only targeted groups.
53:30
Next slide. So, what have we learned?
53:33
We've learned the organizational change process requires system wide intervention.
53:37
Then having the right people in the right place for the right reason can change ideas and practice.
53:43
And the key is having the right tools and resources to really have an impact on the knowledge, skills, and attitudes of our providers. We can achieve our vision of oral health for all, unless we change our approach to oral health care.
53:58
Integration, and collaborations key. We can't do this alone.
54:02
We really need to move beyond the symptoms of health disparities to aiming our policies and funding, changing the structure, and creating those disparities.
54:12
NIH activities are made possible due to the generous gifts of our legacy thunders.
54:17
We appreciate that along with us. They're making the right thing to do, the easy thing to do.
54:23
Thank you for the opportunity to speak today.
54:28
Thank you, Anita, for sharing how we can work together across the health professions to improve oral health and reduce disparities.
54:36
We'd like to use our remaining few minutes to engage in Q&A with our audience, so I can invite our speakers to come off mute and join us on camera. And I wanted to start with the follow up question for Dr. Chalmers. Could you share with us what states are participating in the CMS Learning collaborative?
54:58
Yes, absolutely. So, this is a very action oriented learning collaborative that supports the States in the design and the implementation of quality improvement projects.
55:09
Would emphasis, again, is providing access to fluoride varnish for very young children under six, and the 13 states we're working with our Alaska, California, Connecticut, Idaho, Louisiana, Massachusetts, Mississippi, New York, North Dakota, Oklahoma, Oregon, South Dakota in Washington, and has been really an incredible opportunity to connect with the states. I love, I think you said the action is very local to understand the challenges and help them overcome those with the principles of quality improvement.
55:45
Thank you. We had a few questions come in about disparities and oral health and the American Indian and Alaska Native population and I know in the infographic that NIHCM created, we, you know, tried to include some data. But I know there's just also some data collection challenges and was hoping, Dr. Chalmers and others. Could you speak to that to the extent you have experience working, working with that population and addressing those disparities?
56:18
Yes, share these well-known disparities. And what I can assure everyone, is that the administration is very much committed to collecting quality data, to your point. Sometimes the data is hard to find, But we, we are committed to developing strategies to address these needs.
56:37
Because if you don't know the problem and can fix it, there are many challenges.
56:42
But the nice thing about being in an administration that is so supportive in addressing health equity, is that we can find creative tools to address them.
56:51
Great question.
56:52
I'd like to add, I'd like to add to that if I could, just from the perspective of my role as chair of the advisory Committee and training in Medicine and Dentistry, one of the solutions that our committee has identified, and just recently, is preparing a letter that will go to the Secretary of HHS.
57:11
And the Congressional committees, is to really prioritize development funds, funding, and development of programs, on hands that support IHS delivery sites.
57:24
And we're hoping that that will be another way to systemically push some of these changes into the areas of need.
57:32
Great.
57:35
And a few other questions came in about disparities and access disparities for people living with disabilities.
57:44
Are there any innovations or sort of other strategies that you could share with the audience about reaching, reaching those people?
57:58
I guess, I would, it's clearly an important need in a very underserved population. And, and, again, the committee is now looking to use their 19th report, which they're annually prior to the Secretary in Congress to really support funding for programs that address the needs of individuals with developmental disabilities, just isn't IDD specifically.
58:23
And if I could share my clinical perspective, you know, I've had the opportunity to treat many children with developmental disabilities, and the challenge they face as they age into adulthood is finding providers that will address their needs adequately. As I mentioned in my earlier remarks, as sometimes, the operating room is the safest place for them to receive care. But we've also seen such an advancement in preventive measures that, again, just really training the workforce to address the needs of the individuals with disability, and providing points of axes that are convenient for them. And, and really could put them on a trajectory to good oral health.
59:05
Thank you for the question, it's extremely important.
59:08
Sure.
59:12
We have a lot of questions coming in that we're gonna have to follow up with some of the speakers individually since we're almost out of time and I know Katie, some specific questions about getting some great insights from you on the school programs. But maybe just to close, you know Katie spoke about some of the innovations coming out of pandemic or other lessons learned if you would, each one to share with us. You know, something that you didn't get a chance to say today or another innovation that you'd like to leave us with. This has been a really powerful presentation with a lot of great data, a lot of great insights for our audience.
59:53
So, Katie, do you want to start, is there anything else that you've been seeing that you want to share?
1:00:00
Overall reflection, I'd share is that things that we want thought impossible are actually possible, and so how do we leverage that momentum and insight to do better?
1:00:12
Anita.
1:00:14
I mean, I think the shifts in policy and payment that are occurring due to the pandemic or something we need to pay great attention to, successfully meeting the needs of more individuals and particularly their scientific innovations that are coming from the telehealth space, which really can provide, go a long way I think to providing access and collaboration across providers and patients.
1:00:39
Dr. Chalmers, I just want to thank you for the opportunity to bring a focus on this very important issue.
1:00:46
And this is the, it's the beginning to start the conversations, and it needs to be translated into action so we could see improved oral health for all the beneficiaries. Thank you for the opportunity.
1:00:59
Well, thank you to our really excellent speakers for being with us today. Thank you to our audience. We will be sharing a transcript and a recording of this. We also would love to have your feedback. You can take a moment to complete a brief survey, and also invite you to check out our other resources. I mentioned our recent infographic on oral health.
1:01:25
You can also access the speakers' slides and additional resources on our website, and we also invite you to register for our next webinar that is occurring next week. That will focus on the impact of long ... Ed. So, thank you, all, again, for joining us today.
Speaker Presentations

Natalia Chalmers, DDS, MHSc, PhD
Centers for Medicare and Medicaid Services

Katie Eyes, MSW
Blue Cross and Blue Shield of North Carolina Foundation

Anita Duhl Glicken, MSW
National Interprofessional Initiative on Oral Health & University of Colorado School of Medicine
More Related Content
See More on: Health Equity | Health Care Reform | Social Determinants of Health