Webinar
It’s OK Not to Be OK: Physician Burnout and Mental Health
Part of "Health Care Workforce 2021"
Time & Location
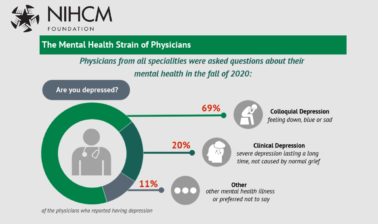
The COVID-19 pandemic has exacerbated the existing crisis of physician burnout, with lasting implications for health care access and quality. A recent survey showed 8% of physicians permanently closed down their offices in the last year due to financial and mental strain, resulting in potential gaps in coverage for patients. Around 71% of physicians reported exhaustion and burnout in 2020, up from an estimated 29%- 54% of health care workers in 2019. The pandemic has highlighted the critical need to reduce the stigma physicians encounter when seeking help and increase their access to mental health health services. In this webinar, we heard from health care leaders who are working to reduce burnout and address challenges related to the pandemic.
Speakers discussed:
Overview of physician burnout before and during the COVID-19 pandemic, how it impacts patient care and access, and how federal and health system leaders can improve clinician well-being
Why doctors are hitting their breaking point and what they are doing to help each other and promote a culture of wellness in the medical field
A statewide collaborative to support providers through rapid sharing of evidence-based science and funding support to build resilience during the pandemic
Kathryn Santoro (00:00:01):
Thank you. I'm Kathryn Santoro, director of programming at the National Institute for Healthcare Management Foundation. On behalf of NIHCM, thank you for joining us today. This is our second webinar in a series on supporting the healthcare workforce.
Kathryn Santoro (00:00:17):
The COVID-19 pandemic has exacerbated the existing crisis of physician burnout. Seventy-one percent of physicians reported exhaustion and burnout in 2020, up from an estimated 29% to 54% of healthcare workers in 2019. This has lasting implications for both healthcare access and quality.
Kathryn Santoro (00:00:41):
A recent survey showed 8% of physicians permanently closed down their offices in the last year due to financial and mental strain, resulting in potential gaps in coverage and access for patients. The pandemic has also helped advance the discussion that we will continue today of clinicians experiencing moral injury as they have been on the front lines of the COVID-19 battlefield for this past year. We will hear from a prestigious panel of experts to explore strategies to support clinician wellbeing during the pandemic and beyond.
Kathryn Santoro (00:01:18):
Before we hear from them, I wanted to thank NIHCM's president and CEO, Nancy Chockley and the NIHCM team who helped to convene today's event. You can find full biographies for our speakers, along with today's agenda and copies of their slides on our website. You can also find more information on the Do No Harm documentary on physician suicide, one of NIHCM Foundation's journalism grantees. Our grant is supporting film screenings and panel discussions for legislators, medical schools, and hospitals across the country, to open a dialogue about the challenges and solutions to this crisis. You can visit their website at donoharmfilm.com, to find ways to see the film for individual and group screenings. We also invite you to join the conversation today on Twitter using the hashtag #physicianburnout.
Kathryn Santoro (00:02:15):
I am now pleased to introduce our first speaker, Dr. Donald Berwick. Don began his career as a pediatrician and as a leading authority on healthcare quality and improvement. He is a former administrator of Sienna and currently serves as president emeritus and senior fellow of The Institute for Healthcare Improvement, which he co-founded. Don also serves as an advisor to NIHCM and we are so grateful he is with us today to offer his perspective on this important issue. Don.
Donald Berwick (00:02:50):
Thank you so much, Kathryn. It's an honor to join you on this very important topic. I'm grateful to NIHCM for teeing up what's going to be a fine session, I'm sure, with my colleagues Mona and Tom. My intention in the next 15 minutes is to rather breathlessly, is to introduce you to some of the science that we have beyond the problem of physician burnout. The bad news is there's a lot of burn out, the good news is we know a lot about what to do about it.
Donald Berwick (00:03:21):
Definitions here and I'll give you references shortly. Burnout is a syndrome characterized by a high degree of emotional exhaustion and high depersonalization. That means the [inaudible 00:03:33] of the job itself, a cynicism and a low sense of personal accomplishment from work.
Donald Berwick (00:03:39):
You'll hear the word resilience used a lot and the definition is here. Resilience refers here to the glue that holds groups together, provides a purpose larger than the solitary self. You're part of something bigger than yourself, and allows entire groups to rise to the challenge.
Donald Berwick (00:03:55):
As you heard from Kathryn's introduction, we have some bad problems with burnout in healthcare. They pre-exist COVID, rates of burnout among doctors, nurses and nurse practitioners and physician's assistants are relatively high compared to other job occupations and they have been for years. These data are nearly 10 years old and you can see the high levels of burnout. If you compare physicians to the overall population for burnout rates and for satisfaction with work life integration, physicians turn out to score rather poorly compared to the population at large. As Kathryn said, COVID has made it worse. Burnout rates now in the COVID era approach well over 50% for physicians asked about their current state of mind.
Donald Berwick (00:04:45):
The consequences are severe. This slide comes from the Mayo Clinic book that I'll be showing you shortly. But it catalogs all of the downstream effects of physician burnout and loss of resilience, both for the individual physician and for the physician in their professional role. The consequences for patients and patient care are also serious. For example, in the area I'm very concerned about, medical error, there's two and a half fold, a 220% increase of medical errors in the work of the good physicians who are burned out.
Donald Berwick (00:05:27):
The science I'm going to be sharing with you has a lot of pedigree. I want to call your attention to these two recent books, which to me create a goldmine of opportunity for those interested not just in documenting burnout, but learning what to do about it. The first, it's got to be the instant classic literature by Steve Swensen and Tait Shanafelt, Strategies to Reduce Burnout: 12 Actions to Create the Ideal Workplace. I'll be sharing with you quite a bit from this book in the few minutes ahead. The National Academy of Medicine has also had a ongoing project on physician burnout and it included this very seminal report on physician burnout, which appeared last year from a consensus panel report. The stuff I'll be presenting to you comes from both of these documents.
Donald Berwick (00:06:15):
The first scientific point I want to make is you can measure burnout. Christine Maslach, 40 years ago developed what's known as the Maslach Burnout Inventory. It's not just specific to healthcare, but it's very pedigreed, it's well documented, it's easy to use. It is long, there are 50 items in the Maslach Burnout Inventory. Steve Swensen and Tait Shanafelt proved at Mayo Clinic that there are three items which basically capture from that inventory, most of the variants you're going to see in the overall score. A question about emotional exhaustion, a question about the cynicism or depersonalization at work and a question about self-efficacy. A sense of being able to have an effect on the condition of the patients and the workplace.
Donald Berwick (00:07:03):
Those of you interested in getting serious about this in your organizations, I will tell you, this is just one among several well pedigreed instruments that can be used to study and measure and track burnout levels in your organization.
Donald Berwick (00:07:15):
I mentioned the National Academy of Medicine Project. This is a major project, I believe it's been going on over three years now. It's an action collaborative on clinician wellbeing and resilience. Several key figures from American healthcare are leading this and it's a rather large campaign. I assume that if you would get in touch with the National Academy of Medicine, you too can become more involved with this very important platform for leading, I believe now even more so, to a national campaign to improve physician wellbeing.
Donald Berwick (00:07:46):
The goals of that National Academy action collaborative is raise the visibility of the problem, to understand the sciences behind the challenges and to advance solutions in concert with the people as part of the collaborative.
Donald Berwick (00:08:00):
I'm showing you this model, which I know you can't read it on the screen here, make use of it, but each of the major searchers in the arena of physician burnout have produced models of the factors that underlie wellbeing, resilience and burnout. This is the model that was generated by that National Academy of Medicine report, which is now used as an action framework for organizations and policymakers to think about moves that will help improve clinician wellbeing.
Donald Berwick (00:08:28):
Most of the rest of what I'll be showing you comes from these two absolutely key researchers who were involved and remain involved with the National Academy. On the left is Dr. Steve Swensen, from Mayo Clinic Intermountain Healthcare, now back at Mayo and Dr. Tait Shanafelt, also at Mayo Clinic originally, now at Stanford. Steve and Tait are, I would say, the thought leaders in this field. The people that have done the most disciplined research. They've done it for a decade, they did it long before surf was up on this problem and the COVID pandemic.
Donald Berwick (00:08:56):
I mentioned frameworks you will find in Tait Shanafelt's work at Stanford, the Stanford WellMD Model of Professional Fulfillment. Again, there's more here that you can digest. These slides will be available to you and you can check out Tait's work. But if you want a framework for action on burnout and wellbeing, the Stanford model is strong.
Donald Berwick (00:09:18):
And the Institute for Healthcare Improvement, the organization that I used to lead, and now senior fellow at, has produced a downloadable framework for producing joy in work, which is the positive side of the challenge of working on burnout. There is a lot of action going on at IHI, I urge you to get on the IHI website if you want to see ways to join the Institute for Healthcare Improvement activities on joy in work.
Donald Berwick (00:09:43):
I'm going to take the last couple of minutes to show you the framework that emerged from Steve Swensen and Tait Shanafelt's work at Mayo Clinic. This comes from their book and I strongly commend it to you. Steve has redacted the results. It took four areas of action for organizations or individuals that want to work on burnout or resilience. Or as they put it, flourishing. They're rather interesting categories, highly actionable, four categories.
Donald Berwick (00:10:12):
They all cycle around this central model of conditions for flourishing. They're called here by Swensen and Shanafelt, agency, coherence and camaraderie. This comes from 40 years of research and especially decades of research on self-determination theory. Studies of core human needs that are not just anti-burnout, but pro flourishing.
Donald Berwick (00:10:40):
Agency refers to the capacity of individuals or teams to act independently. The sense that I can do things. Coherence is a sense that you're part of something larger than yourself. And Camaraderie is a matter of social capital and interaction. You'll see these three play out in the model that Mayo Clinic produced.
Donald Berwick (00:11:02):
The first of the four areas, you may be surprised about. It's called removing pebbles. It has to do with the concept of leadership taking action to remove small hassles from the work of the workforce all the time, every day. The constant removal of small obstacles to getting one's work done through the framework that Swensen teaches is listen, sort, empower. It's just a framework for rapid cycle improvement of removing pebbles. It involves just what it sounds like it involves. It's identifying what's hassling people trying to do their work, to get through their day. Then as a leader, as an executive, as a manager, understanding what those hassles are and simply removing them constantly with feedback to the workforce on that job.
Donald Berwick (00:11:45):
In the Institute for Healthcare Improvement, we ran a project in our leadership alliance, which you are welcome to join, there are 55 organizations in it now. Two years ago, we ran a project on stupid rules. Rules that stand in the way of patient care. Eighty-five percent of those rules turned out to be non-regulatory, they were perfectly within the capacity of organizations to change things to make it easier for the staff. Twenty-four of the 55 organizations produced a list of 360 stupid rules in one week. The entire project then got devoted to stopping requirements to do stupid things in the work with patients.
Donald Berwick (00:12:18):
The results of the work on pebbles is astounding and well documented. Well documented in cluster randomized trials. This is systematic research done at Mayo Clinic. A 21 point reduction in burnout. That's not a 21% reduction in burnout, that's a 21 point reduction in the Maslach scale score. Highly positive results for satisfaction and teamwork simply by organizing leadership energies to remove little hassles in work.
Donald Berwick (00:12:50):
This is testimony from a doctor and nurse partner at McKay-Dee Hospital Intermountain Healthcare System, who basically conducted in their team in the ICU, a removing pebbles project. They had astounding results. Six months after that project began, they had reduced rounding times in the ICU from over seven hours to an hour and a half. Understand what that does to the conditions and motivation and sense of empowerment of the workforce. And it can be done right there at the front line as long as there are leaders willing to facilitate removing the pebbles.
Donald Berwick (00:13:26):
This next slide shows you a resource you can have. The American Medical Association has set up a steps forward online access model, built on the Shanafelt and Swensen model, in which there are tutorials linked to every one of the four elements I'm showing you. This is the tutorial for the pebbles removal project. The only thing you need to notice, is if you get on the American Medical Association website and look at the steps forward modules, you'll be able to do self-study on these four areas.
Donald Berwick (00:13:56):
The second area is a surprise. Its commensality. This comes out of research that Steve Swensen has done and it is supported by three randomized clinical trials, all which have results including reduction in cortisol levels, stress levels in subjects in at least one of the trials. It has to do with eating. When people in an organization or a group are able to spend time together relaxed in conversation where there are no boundaries, no rules, you can actually begin to let your hair down and share what's going on in your lives. Especially around meals, believe it or not, there are remarkable results in reduction of stress and burnout.
Donald Berwick (00:14:35):
There's a project that I'm involved in called Bongo. You can get on the website for bongomedia.com, which is using this idea of conversation in very small ways within organizations to help people simply talk with each other. Very simple change. Dr. Christine Sinsky at the American Medical Association, by the way, has picked up on all of this and that's why the AMA now has the steps forward tutorial. This is the tutorial on commensality.
Donald Berwick (00:15:02):
The third of the four areas in the Swensen and Shanafelt models, they call job crafting. It's a little harder to explain, but it has to do with an observation that one of the most important aspects of that triad of meaning in your work and agency, coherence, camaraderie, is that people are able to do in their jobs things that mean something to them, instead of nonsense. Job crafting is the senior management undertaking to do as much as you can to restore elements of work in the job descriptions and opportunities that workforce has to do the stuff that means something to them.
Donald Berwick (00:15:49):
Clinicians that spend at least 20% of their time doing what is meaningful to them, have half the burnout rate to those that say they do not. Twenty percent of your time, one out of hours. If you can invest in a workforce that says at least one out of five hours I'm able to do work that means a ton to me, you get far lower burnout rates.
Donald Berwick (00:16:11):
The fourth of the four categories is leadership behaviors. This has been very well documented by those Mayo Clinic researchers and by Tait Shanafelt now at Stanford University. There's a more complex story here I don't have time to tell you, but there was major research done originally at Mayo Clinic, validated now elsewhere, studying the relationship between specific leadership behaviors and burnout in the workforce. At Mayo Clinic, the study was originally of 41 department chairs. They expanded to 3,300 care leaders in the Mayo Clinic system, overseeing 65,000 staff.
Donald Berwick (00:16:48):
The question was, what do leaders do that reduce burnout? The answer is five things. This comes from very systematic research which you can access in the book. But when leaders engage in behaviors that are inclusive, treating everyone with respect and nurturing their culture, where everyone feels welcome. When they're informative, they transparently share what they know with the team. When they constantly inquire of the team how things are going. When they invest in professional development and aspirations of staff, and when they just express gratitude.
Donald Berwick (00:17:19):
Five simple, almost obvious leadership behaviors, but highly variable in the Mayo Clinic data. Even among the original 41 department chairs, enormous variability in the degree to which they engaged in these behaviors. The association between those behaviors and burnout levels was profound. I've hardly ever seen correlation coefficients of the magnitude that Swensen and Shanafelt reported in this study.
Donald Berwick (00:17:44):
The scale that they used involves just five questions, which elicit these five behaviors. The maximum score you can get is 60 points. The leader with the highest possible score on all those behaviors gets a score of 60. A one point change, one point out of 60 in leadership behavior on those five variables: recognition, inquiry, information, developing and inclusion, increases fulfillment scores 11% and decreases burnout scores, that Maslach scale, 7%. This is profound impact of very specific leadership behaviors on burnout levels. Again, the American Medical Association steps forward module has ways for you to dig more deeply into the research here.
Donald Berwick (00:18:32):
This all goes back to one of my mentors, W. Edwards Deming, who focused heavily on these issues framed in terms of joy in work. Said people are entitled to joy in work and said, "Management's overall aim should be to create a system in which everybody may take joy in their work." In the work of leaders like Steve Swensen and Tait Shanafelt and the pioneering work now going on at the American Medical Association and at the National Academy of Medicine, you now have a scientific foundation for persuing and reducing burnout and increasing resilience.
Donald Berwick (00:19:04):
Thanks for the chance to share these ideas with you and I look forward to the specific comments we're going to get from Mona and Tom and to your questions. Thanks a lot, Kathryn.
Kathryn Santoro (00:19:14):
Thank you so much Don, for sharing these insights and research that help inform health stakeholders across the healthcare system, can support clinicians and their wellbeing.
Kathryn Santoro (00:19:25):
Next we will hear from Dr. Mona Masood, founder and chief organizer of the Physician Support Line. Board certified in general adult psychiatry, Dr. Masood is an outpatient psychiatrist in the greater Philadelphia area and a board member of a non-profit community mental health organization, Muslim Wellness Foundation, which provides mental health educational services to the community. Physician Support Line has been a key peer to peer support for providers and we're so please she is with us today to share some lessons learned as we approach the one year anniversary of the launch of the support line. Mona.
Mona Masood (00:20:07):
Good afternoon everyone. Thank you so much for having me. Thank you for the kind introduction and thank you for welcoming me into this space.
Mona Masood (00:20:16):
We were lucky to talk about the objective evaluation and data regarding physician burnout and I'm hoping what I can lend to this conversation is what it's like to be on the "front lines" of the pandemic and ongoing lived experiences of a physician. I titled this short talk Doctor "Burnout." Burnout being in quotes because it is something that we colloquially use and we talk about. I wanted to take us a little deeper than the term itself and discuss the concept of moral injury. I'll explain in a second what that is.
Mona Masood (00:21:12):
I have no financial disclosures and I will return to this slide in a little bit, but I did want to just disclose that I am the founder and chief organizer of Physician Support Line. We are a peer to peer support line made up of over now I think 1,000 volunteer psychiatrists nationwide. We're all US licensed psychiatrists and we provide free, confidential support to our physician colleagues throughout the United States. It can be on any subject and it's usually on every subject that most human beings are going through during COVID. But with a understanding of a shared experience of being a physician during this time. This is our hours and this is our phone number and this is how you can follow us. I'll get back to this in a bit.
Mona Masood (00:22:10):
All right, what's in a name? I'm a psychiatrist, so words are my thing and we talk a lot about that words matter and what we say matters, especially in my field. What we're going to be doing, is we're going to be redefining burnout, the concept of self-care and moral injury in order to better apply it and to understand it.
Mona Masood (00:22:36):
Burnout, as we were just discussing, another definition of it is this constellation of symptoms. Malaise, fatigue, frustration, cynicism, inefficiency that arise from making excessive demands on energy, strength or resources in the workplace. The thing is, the definition, if you're looking at these different symptoms here; malaise, fatigue, frustration, all of these are internal states of being. This is an individual's internal state and what they're experiencing. That's what burnout indicates, that there's a problem with this person's ability to cope.
Mona Masood (00:23:20):
I want to explain why taking a closer look might tell you why that's a problem. Burnout indicates that there's an internal problem of regulating emotion. If there's an internal problem, then the impetus is on that individual to come up with a solution. Then that then leads to suggestions of self-care. Maybe you need to take a break, maybe you need a vacation, maybe you need to use that PTO, have comfort food, take spa days. All of these kind of things where superficially we're finding and these are things that we hear on the support line regularly, is that okay, I did that. I just came back from this vacation or I came back from doing this or I took my time off and I am already dreading going back to work.
Mona Masood (00:24:19):
Because the thing is that even if you do these things and you take yourself out of the work environment it becomes like you have to return back to that same environment that was creating the burnout to begin with. Even though these ideas of self-care practices that we generally suggest are well meaning, they superficially tend to address the pain, but not the cancer. What I mean by the cancer, is this concept of moral injury.
Mona Masood (00:24:48):
Just a little bit of background. Moral injury was first described in the armed services returning from Vietnam. What was happening when these soldiers were going in for treatment for their PTSD and talking to psychologists and psychiatrists, is that we were noticing yes, there's a deep emotional residue from the war. But it wasn't really following PTSD criteria. What PTSD criteria is, is things like being hyper vigilant, reliving or re-experiencing events or feeling like there's an imminent threat to our mortality. That at any second our mortality is in danger, we could die. That is generally what we see for PTSD.
Mona Masood (00:25:40):
But what we were also seeing in veterans and what I continue to see when I have veterans in my practice, is that it was beyond just this imminent anxiety about mortality. But there was an anxiety about morality, about the things they saw while they were in war, the things that they did while they were in a war zone, which deeply compromised their moral compass. This became an imminent anxiety about their morality. You would hear things like, "We were following orders and I did things you wouldn't believe."
Mona Masood (00:26:16):
The reason I'm bringing this up is because I think we've all noticed how COVID is being described. It is being described as a war zone. Who's on the front lines of this war zone? Literally, that's what they're calling us, our physicians and they're on the front line. These are our heroes and people are celebrating the heroes. They're doing all of these kind of things. This very much is taking on this metaphor of being in war.
Mona Masood (00:26:46):
With moral injury in healthcare then, if we apply the concept, it occurs when we perpetrate, bear witness, or fail to prevent an act that transgresses our moral beliefs. Like we said before, I had to make decisions and these are calls we get on the support line. I had to make decisions that I never thought I'd have to before. Such as, who do I decide to give what resource to? Who gets the vent? Who gets my time? Who gets anything? All of these things that are transgressing our moral beliefs.
Mona Masood (00:27:20):
We cannot deny that being a physician has a very deep ethical and moral contract. Our contract is not just our usual job contract that other professions have. We have the Hippocratic Oath, which is a very deeply ethical and moral document. When we're all taking this we really are believing that we're doing some sort of moral or ethical service towards people. That's the job that we're in. But healthcare has never been just a job or a profession. We are in a very unique role where yes, we are being compensated for our services, but we also have a very deep, ethical and moral responsibility. What is happening and what COVID has shown light on, is that we are being very deeply morally injured by the decisions we're having to make during this time.
Mona Masood (00:28:21):
This slide is I'm talking about stakeholders. What I mean by this is that when physicians went into medicine, if we can all remember back to when we decided we were going into medicine, so much had to do with helping people. I think every medical student says that. I want to help people. I want to save lives. I want to do something important and have purpose. That is something that gets compromised as we build our careers. We realize that it is not just about the doctor patient relationship.
Mona Masood (00:29:01):
To be in medicine in America, we have many stakeholders and it is not only the patient, which we knew and which we signed up for. But we also have EMR, we the insurance companies, we have pharmaceuticals, we have [inaudible 00:29:16] authorization. We have the hospital system, we have the federal and the state healthcare system. We have financial issues, such as the loans that we took out to become physicians. Now we have to pay back. With COVID, the stakeholders have been time, because it is a race against the clock, as we find every single day. It is the uncertainty of the direction of this virus and this pandemic and even our own mortality.
Mona Masood (00:29:47):
This is a lot for things for us to be dealing with. Those are the stakeholders and the physician ends up becoming the scapegoat. What I mean by that is when the physician is in the room with their patient, oftentimes the patient's not seeing everything else that is going behind the scenes. They're not seeing all the work that the physician is doing in order to make sure that they get the standard of care or the quality of care. Or the time that the patient feels like they need.
Mona Masood (00:30:18):
The physician inadvertently starts representing all of these many stakeholders to the patient. And often, they can't get what the patient needs or deserves. All the way from a vent to not being able to get a medication because it's too expensive. All of these are seen as somehow the physician has failed the patient. The physician then starts internalizing this. That they have somehow failed their moral obligation that they signed up for to take care of their patient in the way that they wanted to. They feel like their moral compass is compromised. They're not able to heal their patient.
Mona Masood (00:30:58):
This concept, moral injury, you may know that Dr. Wendy Dean and Dr. Talbot are the pioneers of the more modern interpretation of moral injury in healthcare. Dr. Wendy Dean said, "Moral injury describes the challenge of simultaneously knowing what care the patient needs, but being unable to provide it due to constraints that are beyond our control."
Mona Masood (00:31:31):
To understand it after hearing all of this, the takeaway is that burnout the term, refers to a broken individual. That you are not cut out to be a doctor. Moral injury says that it's a broken system. That the work that we're doing is not doing us or the patient what it set out to do. It is doing us essentially a disservice.
Mona Masood (00:32:04):
How do we do this? How do we problem solve through something this major where we're feeling the strain of something compromising our morality? First, there's managing psychological injury. The guilt, the shame, the anger, the resentment. All things that get often brought up on Physician Support Line. Then also managing systemic injuries.
Mona Masood (00:32:32):
Our psychological injuries; the guilt, the shame, the anger, the resentment, all those things that we feel, the role of the individual really is to accept that these are normal reactions to being put in a helpless situation. The normal reaction to being put in not only in the helpless situation, but we're often feeling that we were scapegoated or that we're not able to be guided by our moral compass. Accepting that this is normal to feel those things because in the end, we're human beings that we want to do the right thing. I often remind my patients, as I remind physicians that I speak to and even my physician patients and myself, that you feeling difficult emotions tells you that you care. That you want good outcomes for the people that you're serving and that the opposite of having these emotions is apathy. Absence of emotion is apathy. An apathetic doctor is a worse doctor than someone who feels things, even if it is uncomfortable things.
Mona Masood (00:33:50):
Understanding that having hard emotions serve a purpose. That it reminds us that we have a moral compass. And understanding that when we're uncomfortable, that's when things change. When we again, we're apathetic, or we are fine with the status quo or we're content, why would there be any need for change? All of these studies that we were just speaking about, all the data that was collected, all of this work that is going behind the scenes, it is happening because of discomfort. It is happening because we see that there's a problem.
Mona Masood (00:34:29):
Then forgiving ourselves. Forgiveness of the self is an inner reconciliation where one acknowledges and makes amends for the harm that was done, while also accepting the self as a fallible person engaged in continued moral growth. When this happens is when doctors start seeing themselves as human beings. When we get rid of the expectations or of the hero archetype, where we start seeing ourselves as that even though we are experts, but we are also at risk of the same things that affect our patients. That somehow we are not removed from having the human experience. When we understand that, we're able to forgive ourselves, we're able to see ourselves as having the possibility of growth and being able to get through difficulties. It needs time, it needs deliberation, it needs reconciliation of what has happened and acceptance of ourselves as human beings.
Mona Masood (00:35:42):
In terms of systemic reform, which is really the crux of moral injury, I want to tell you a little bit about two projects that we are doing right now in collaboration with other foundations. Many of you may have heard of Dr. Lorna Breen who was a physician who died by suicide early on in the pandemic, April of 2020 in New York. Her family has done incredible work with the Dr. Lorna Breen Heroes' Foundation. They are pushing some legislative initiatives that really fund access and support of medical professionals seeking mental healthcare, including hospital credentialing barriers.
Mona Masood (00:36:21):
We're also working with the Humans Before Heroes Initiative. This is a collaboration with American Medical Woman's Association to reframe the mental health questions on state medical licensing applications to distinguish illness versus impairment in order to encourage help seeking behaviors amongst physicians.
Mona Masood (00:36:43):
Because the crux of moral injury is that if we feel stuck, if we feel like we are individually or internally failing, that we are more at risk of suicide, of bad outcomes for our patients, of perpetuating the same thing in our future generations of colleagues. So admitting that we're human and admitting that we also deserve help and we need help, and by removing the systemic barriers around help seeking in physicians, we're able to change that narrative.
Mona Masood (00:37:32):
Finally, lessons from the Physician Support Line. The lessons we're learning through our callers is what physicians expect of themselves, what patients expect of them, what family and friends expect of them and what society expects of them. Which is all to somehow have all the answers, to be heroes, to be self-sacrificing. That they are not allowed or to show weakness because if they did, then they are letting down people. That they are letting down not only themselves and what they promised to do, they're letting down their patients, their family and friends and now society. Internalization of these expectations at the cost of our own wellness.
Mona Masood (00:38:19):
I take this time to remind ourselves, the physicians in this audience, that the Hippocratic Oath is about duty towards your patient, but not at your self-sacrifice. I often say this to callers on the line and to my own patients and to myself. That we don't have to set ourselves on fire to keep others warm. In medicine, it was never that wellness is a one way street. We have made it that way and that has been a process of medical culture that has been perpetuated. That wellness is only meant for our patients. But we have to be well to do well. I do hope that the legacy of the work that we're all doing here and talking about here, is that centering ourselves is not being self-centered. It is centering ourselves is important in order for there to be wellness for everyone.
Mona Masood (00:39:33):
Again, this is Physician Support Line. I believe these slides will be made available. I do encourage our medical colleagues here to call us about any subject. It doesn't have to be a crisis. We can help navigate a number of different intersections that happen for physicians.
Mona Masood (00:39:55):
If you want to learn more about moral injury, I do recommend visiting fixmoralinjury.org for resources, literature, toolkits, publications on this subject. These are my references. Thank you so much for having me.
Kathryn Santoro (00:40:11):
Thank you, Mona, for your leadership advancing this conversation on moral injury.
Kathryn Santoro (00:40:17):
Under the leadership of president and CEO Daniel Loepp, Blue Cross and Blue Shield of Michigan has been a recognized leader and partner in a portfolio of statewide initiatives that support the provider community and improve patient care. Leveraging existing consortiums in place for the last 15 years, allowed them to rapidly respond to the impact of the pandemic on providers and support the healthcare workforce and their members over the past year. To hear more about their leadership on this issue, we are now joined by Tom Leyden, director of Blue Cross Blue Shield of Michigan's award winning value partnerships program. Tom.
Thomas Leyden (00:40:58):
Thank you Kathryn. So happy to be here to speak about the Michigan experience. Next slide please. Actually, I see I can hit it myself.
Thomas Leyden (00:41:09):
Okay, real quick, I'm going to tell you a little bit about Blue Cross and the Michigan experience because we're a little bit different than how most health plans operate. We're the largest single state Blues plan in America. We serve about 4.5 million Michigan members. In the value partnerships program we have about $500 million annually that we reward hospitals and physicians and practice transformation to continue to improve quality of care.
Thomas Leyden (00:41:38):
I've been with the program 14 years now and I've always been really proud of what we've been able to do with the provider community. But this last year, seeing how the provider community has been able to respond to the pandemic has just been incredibly rewarding and I'm so happy to share with you some of the things that we've been able to do.
Thomas Leyden (00:41:59):
The value partnerships portfolio has supported the provider community for over 15 years now through the development of learning health systems. There's primarily two flagship programs under value partnerships. We have a physician group incentive program on the ambulatory side. And primarily on the hospital side we have a collaborative quality initiatives program, our CQIs. There's four primary roles that we serve for the provider community.
Thomas Leyden (00:42:28):
We're a convener of the medical community and through that we routinely get the provider community together and provide ongoing safe forums for hospitals, physician organizations, primary care physicians and specialists to address practice transformation needs. When I say ongoing, I'm talking ongoing. Typically these communities get together on a quarterly basis in safe havens to share best practice information in an unblinded fashion. Practice transformation is the primary focus of these forums.
Thomas Leyden (00:43:04):
We also, as the largest health plan in the state, put significant dollars into value based reimbursement and we also as the major convener of providers in the community, have an ability to engage the providers with regards to information, getting information out quickly. We saw this particularly with regards to COVID. The platform served the state really well in that we had all these existing platforms where the vast majority of the providers were routinely getting together. So when the COVID pandemic hit, it was the natural place for providers to go to get information and ask questions. That really was a great stress relief to the provider community, because it helped them coalesce with their peers and get answers to their questions quickly.
Thomas Leyden (00:44:01):
The value partnerships' view of the health plan role is a bit different than some health plans might view their role. We really feel our opportunity is to assemble competitive hospitals and physicians and offer a mutual ground for collaboration. We also feel that we have the ability to provide resources to reward infrastructure development and process transformation. It's all about sharing data and getting information and support to physicians and the hospitals so that they can do what they are there to do, which is provide the highest quality care.
Thomas Leyden (00:44:37):
This final bullet, a heavy hand prompts the provider community to do the least necessary. Don Berwick talked about it multiple times in his presentation. But really it's all about empowerment. Empowerment encourages the provider community to do the most possible. I cannot emphasize that enough.
Thomas Leyden (00:44:58):
The portfolio, explained really simply, is if you provide the support, the tools, the data, the funding so physicians can engage in what they actually want to do to improve quality of care, it works. It helps change the way that healthcare is delivered, and ultimately, it drives a meaningful impact for the customers, the health plans, the members, by improved value of care. Better utilization of resources and improved quality of care, as well as improved member experience.
Thomas Leyden (00:45:30):
I mentioned there's two of these flagship programs under value partnerships. The PGIP Program on the ambulatory side and the CQIs on the hospital side. The key take away from this slide really, is that these programs are designed in partnership with the Michigan provider community. All these initiatives, they are initiatives that we developed hand in hand with the Michigan providers. These are not initiatives that we developed back of the office and then throw over the wall to the providers and say, "Have at it." These are efforts that we worked painstakingly with the providers developing common goals and working with them to actually implement. We modify as needed to continue to accommodate improvements.
Thomas Leyden (00:46:17):
This is going to sound surprising coming from a fellow who's been leading this program for the last 14 years. While financial rewards are certainly very important, there is really a surprising truth about what motivates us, and I say us, I'm talking about the provider community particularly. Financial rewards are certainly great, but studies have shown better outcomes are found when people are intrinsically motivated. The value partnerships programs have long adhered to many of the principles espoused by Daniel Pink. If you've not read any of Daniel Pink's work, I'd encourage you to do so. There's a link in this to a 10 minute video of his that I highly recommend you watch.
Thomas Leyden (00:47:04):
Dan really focuses on three themes. Autonomy, the urge to direct our own lives. Mastery, the desire to get better and better at something that matters. And purpose, the yearning to do what to do in the service of something larger than ourselves. I really do believe that these three principles really help providers, particularly in times of great strife. Again, I cannot encourage you enough to watch his video. It's a great 10 minute video and it really hopefully will change the way that you think about how to engage and reward providers.
Thomas Leyden (00:47:44):
Through our PGIP Program, particularly through the last year, we tried to do quite a bit to help our provider partners through the COVID pandemic. At the very start we had lots of concerns amongst the provider community. Lots of concerns about patient testing, lab operations, protocols, how to get tests, what the results meant, et cetera. There were also incredible concerns about funding and sustainability of providers. In Michigan, half of our providers are independents and those providers are often one to three person providers. So we worked tirelessly to make sure that we were changing funding streams and getting funding to independent providers and all providers frankly, to make sure that they had funding available to them to put in place telehealth systems. To rapidly evolve the way that they delivered care.
Thomas Leyden (00:48:38):
We also assembled weekly meetings with our provider partners to get information flowing. We invited the State of Michigan and they would routinely attend our meetings. We invited our lab partners, we invited the state medical societies. We also wanted to make sure that our provider partners understood the CARES Act and all the various regulations, so we continue to provide educational opportunities to our partners to help them to dissect and understand all the various legislation and what it meant it to them. I can't over emphasize the importance of educating people because it's great that there's a lot of information out there, but it's hard to rapidly understand it in crisis times like this.
Thomas Leyden (00:49:22):
I mentioned the work that we did in telehealth. In two weeks we launched the telehealth initiative within COVID hitting the State of Michigan. Within four to five weeks, we had over 80% of our providers offering telehealth services. That's down from 10% four weeks previously. When I say providers, I'm primarily talking primary care physicians and behavior health providers.
Thomas Leyden (00:49:48):
I'm going to switch over to our second key program and that's our CQIs, which are our statewide improvement programs that are centered around clinical registries. Our CQIs again, are hospital programs for the most part. These are programs that are clinically rich databases. Cardiac surgeons, radiation, oncologists, emergency medicine physicians, trauma surgeons, et cetera. These programs have been around 15 plus years, long standing programs where the locus of control is with the providers. That's incredibly empowering to the physician community. There's solid confidence in the integrity of data, which is also very meaningful to the physicians, as well. The data is shared freely at the meetings. It's often unblinded so no one's hiding behind letters. Hospitals are freely sharing where they're succeeding, as well as where they're failing. You'll have hospitals from one part of the state sharing their successes and their failures and helping one another get over some of the failures that they've had.
Thomas Leyden (00:50:54):
Evidence based medicine typically takes 15 years from the time that a new best practice is discovered until it's actually in place. Through our CQI model, we've discovered best practices where we've been able to implement across the consortium the best practice in as little as a year. The reason we've been able to do that is because there's such strong confidence in the integrity of the data.
Thomas Leyden (00:51:20):
Another one of the key learnings and one of the key supports to the provider community is peer to peer review and coaching. There was a study that came out of the CQIs about four years ago. It was in the New England Journal of Medicine and basically we had bariatric surgeons who allowed themselves to be videotaped and we found through the data registries that those surgeons who were videotaped and had their peers assess their technical capabilities often had less than optimal outcomes when their peers thought that their surgical techniques was less than optimal.
Thomas Leyden (00:51:57):
When we offered peer to peer review and coaching, the surprising thing was often those surgeons who had surgical technique that was considered optimal were the ones raising their hand, asking to have their peers help them improve their techniques. So again, surgical competence doesn't necessitate that physicians want and crave additional support. It's all about providing resources and support for the medical community to help them to continue to self-actualize and improve.
Thomas Leyden (00:52:39):
There's a longstanding mantra with the CQI Program that quality improvement moves at the speed of trust. I'd say physician engagement also moves at the speed of trust. The CQIs are all about learning, they're all about building an atmosphere of networking, developing shared goals, transforming care delivery. This next quote is a quote that really could be said by pretty much many of the surgeons participating. "My involvement in the CQI is the single most influential and helpful activity that I have engaged in during my entire career." I'll tell you, having attended these meetings for the last 14 years, our urology CQI, the attendees meet on Fridays from noon to 5:00. It is not uncommon for the attendees to still be there at 5:30 on a Friday afternoon on a... If you provide opportunities for the collaborative where they find value and it helps them continue to build their skillsets, they will engage.
Thomas Leyden (00:53:49):
Through the COVID crisis, we have been able to provide resources. When COVID hit we launched a CQI registry around COVID to help them determine best practices and address huge variation in treatment. Then when COVID started to wane, we helped hospitals bring elective surgery volumes back up based upon data that we had collected. Then when COVID started to rear its ugly head again, we started up a 24/7 helpline for ICUs across the state, where they were able to call in and ask their peers for information and help 24/7, to help them provide higher quality care.
Thomas Leyden (00:54:34):
I'm going to skip a slide or two, because I want to share a couple key pieces of information for you about other areas that they've been able to provide support. One more slide.
Thomas Leyden (00:54:50):
Other areas that the CQIs have been able to provide support. We have an oncology collaborative and they actually did something right before COVID hit which was fascinating. They brought in spiritual leaders from across a variety of different spiritual areas. Imams, reverends, rabbis, fathers, Buddhists, spiritual non-religious, to help oncologists have difficult conversations with individuals with cancer. I was there and I can tell you we've had oncologists bringing up cases that they had 15, 20 years prior that had haunted them for 20 years. They were saying things like, "I wish I had the tools that you're providing me now because I struggled so hard with this case and I just didn't feel I had the skills to provide this care."
Thomas Leyden (00:55:41):
Additionally, physician burnout has long been an issue. Our emergency department collaborative continues to provide resources to ER physicians across the state. I've provided links throughout the presentation for you. They provided boiler plate letters that ER physicians across the state could provide. I'm going to ready you just one line from this. This is a letter that they give to ER doctors that they could tailor for family members. The letter says, "The new pressures of my job will make me tired when I'm at home. I might seem quiet or distant. Remaining strong for people that are hurt and sick isn't easy, I need your help. Just knowing that you think about me brings me happiness. A kind word or a hug from you is like rocket fuel to my day." It goes on and on. It's all about providing tools to providers when they need them.
Thomas Leyden (00:56:35):
Again, we've had webinars, we continue to engage providers. We're asking providers about burnout and we're sharing data routinely with the providers to let them know they're not alone.
Thomas Leyden (00:56:50):
In closing, I would just share with you a couple thoughts. We've received additional feedback that people appreciate this. But the take aways for you all is watch the Dan Pink video. Autonomy, mastery and purpose are incredible internal drivers. Think through your programs on how they support daily empowerment of your teams. You'd be amazed when how many people feel ill equipped to have difficult conversations. Provide the resources to help bridge the gap. Look to free up funds and resources during times of crisis, ask questions on how your teams are doing. Benchmark, act on the data and don't assume because the resources are out there that everyone understands the information.
Thomas Leyden (00:57:33):
Finally, I would encourage you to empower, empower, empower. Thank you very much.
Kathryn Santoro (00:57:40):
Thank you Tom and Blue Cross Blue Shield of Michigan for your leadership. And thank you to all our speakers for these incredibly rich presentations today. I would like to close us out with a question for our panel.
Kathryn Santoro (00:57:55):
Mona mentioned Dr. Lorna Breen and we know the American Rescue Act contained several provisions to address suicide prevention [inaudible 00:58:06] and improve access to mental health services for our healthcare workforce.
Kathryn Santoro (00:58:13):
Can our speakers talk about the significance of this? What you hope to see come of this investment or leave us with another key take away that you'd like the health care system and leaders to address as we navigate through the lessons learned from the pandemic and the issues of racial injustice that we've all faced, including the health care system over the past year.
Mona Masood (00:58:40):
Sure, I can take this question. Yes, it's incredibly important that there be legislative action in addressing physician burnout and moral injury because so much of what is going on for physicians is about the permission. Whether it is the permission by the medical culture itself between physicians, whether it's permission by our state licensing entities or our hospital credentialing systems that our wellness matters.
Mona Masood (00:59:19):
The way that we show permission is by not creating punitive barriers to physicians seeking help when they need help. That has been a big stressor for so many people and why we even had to create the Physician Support Line to be unaffiliated with any systemic entity and to promise anonymity and confidentiality and that we would report to no one, was because of these stigmatized barriers that we have in medicine and in the way that medicine is set up in terms of legislation and just in terms of the system.
Mona Masood (01:00:05):
These acts are very important. Not only do they bring it to the forefront and it becomes something that spreads awareness, but it's something that is validating and something that when it is talked about and when we are putting words to what is an internal experience for physicians, it allows a physician to feel like there are outs. That they are not stuck, that they do not have to take extreme measures in order to escape the very real turmoil that so many of them feel in terms of whether it's patient care or their own care.
Mona Masood (01:00:43):
With the Dr. Lorna Breen Act, which just got put through Congress and I believe has been gaining a lot of momentum, the goal is for there to be a normalization of physicians seeking help and also that the system also does not make it punitive. There won't be questions on applications about seeking help and there'll be actually encouragement from health care systems to do so. I hope that answered the question.
Kathryn Santoro (01:01:18):
Thank you. Don or Tom, would you like to weigh in or offer any closing take aways?
Donald Berwick (01:01:23):
This is Don. I would just underline what Mona said. It's a two-step process. Step one is we have to understand that to ask clinicians to be heroes causes trouble. I was trained that it was all on my shoulders and it's a very lonely and impossible task. Of course, we're going to be dedicated but we need to understand that we're frail human beings too. So step one is to create a professional culture, as Mona said. In which saying that is not weakness, in fact, it's strength.
Donald Berwick (01:02:00):
Then the second step is the organizations in which we find ourselves have to create their sources that troubled and distressed physicians who need the help, as I have in my career, can turn to and say, "We're here for you and we're ready to help you."
Donald Berwick (01:02:15):
When we have those we'll see a lot less of the tragic consequences of burnout.
Thomas Leyden (01:02:23):
I would just add, one of the things I've heard on some of the webinars we've had is, I think we underestimate the amount of stress. I get that we need to move the resources where they're needed, but I think we underestimate the amount of stress that it causes individuals to move them to areas where they're not confident or they're not secure or they don't feel like they have the skills to do the job. I think that we definitely need to make sure that they feel that they have the resources and the ability to voice their concerns or get the support that they need.
Thomas Leyden (01:02:57):
Then I would just throw out one final comment. My daughter is actually a Navy nurse and she told me the other day. She said, "It's great to see nurses get the recognition that they deserve," but she says, "I think that lots of people didn't go into medicine to be a hero." She goes, "I knew when I went into the Navy that there was a slight chance that I was putting myself in harm's way, but I don't think the average healthcare provider put themselves into healthcare and put themselves into this to be thought of as a hero." She says, "While it's great that people are recognizing our contributions, there's an incredible amount of pressure that is a double edge sword." I'd just throw that out.
Kathryn Santoro (01:03:44):
Thank you Tom and thank you to our great panel of speakers for being with us today and to our audience for joining us for this discussion. There will be a recording available and slides are available on our website. We'd also encourage you to provide feedback. Please take a moment to complete a brief survey that can be found on the bottom of your screen.
Kathryn Santoro (01:04:08):
We also invite you to join us for our next webinar in this series, which will be on April 8th, with a focus on the role of community health workers and pharmacists. You can find registration on our website. We also invite you to check out our other resources, including our infographic on moral injury and physician burnout and a link to information on the Do No Harm documentary on physician suicide, which is one of NIHCM's journalism grantees.
Kathryn Santoro (01:04:39):
Thank you all again for joining us today and stay safe.
Speaker Presentations

Donald M. Berwick, MD, MPP
Institute for Healthcare Improvement

Mona Masood, DO
Physician Support Line

Thomas Leyden, MBA
Blue Cross Blue Shield of Michigan
NIHCM Grantee Documentary on Physician Suicide
Visit www.DoNoHarmFilm.com to find ways to see the film for individual and group screenings
More Related Content
See More on: Behavioral Health | Coronavirus | Health Care Coverage