Webinar
Long COVID: New Research and the Economic Toll
Time & Location
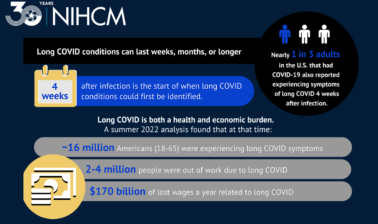
As we enter the third COVID winter, nearly 1 in 3 adults in the US that had COVID-19 also reported experiencing symptoms of long COVID at some point. Emerging research illustrates that long COVID is not just a health problem — it’s an economic one too, disrupting patients’ lives for years to come. Research has found that the economic losses of long COVID could be as high as $3.7 trillion, when factoring in the lost quality of life, the cost in lost earnings, and the cost of higher spending on medical care. Pinpointing the underlying causes of this new and emerging illness has continued to be difficult, and could make treatment costly. Many people fear that the same factors that caused racial and ethnic disparities during COVID-19 may be responsible for driving disparities in the treatment of long COVID. This webinar explored:
0:50
Good afternoon. I'm Katherine Santoro, senior director of programming at the National Institute for Health Care Management Foundation. On behalf of ..., thank you for joining us today for this important discussion on long Covid.
1:04
Recent national data from the Centers for Disease Control and Prevention found that nearly one in three adults in the US that had kind of a 19, also reported experiencing symptoms of ... at some point.
1:18
We also continue to see the impact of health disparities as some people are at increased risk of getting sick from covert 19 and developing Long coven because of where they work, where they live, and their access to health care.
1:32
The urgency of this ongoing threat was highlighted this week when the CDC reported that more than 3500 Americans have died at least in part due to long COVID.
1:44
Today, we will hear from a prestigious panel of experts to learn more about the impacts that long COVID as having on Individuals, Families, and Communities, as well as the economic burden.
1:56
Before we hear from them, I want to thank Nick Adams, president, and CEO, Nancy Chockley, and the ... team, who helped to convene today's event.
2:04
You can find biographical information for our speakers, along with today's agenda and copies of slides on our website.
2:13
We also invite you to join the conversation on Twitter, using the hashtag Long coven.
2:20
Am now pleased to introduce our first speaker. Doctor Walks, her course shots. Doctor ... serves as Director of the National Institute of Neurological Disorders and Stroke.
2:31
He joined NINDS and 22,007 as Deputy Director and has held leadership roles and a number of NIH and NINDS programs, including co leading the NIH's Brain Initiative and Recover Initiative.
2:48
The Study of post acute skylight of Combat 19.
2:51
We're so honored to have him with us today to help us better understand long koven after coercion.
2:59
They are very much, Katherine. It's a pleasure to be here and I'm going to talk to you a little bit about what we know and probably more about what we don't know about this condition.
3:10
And we use the term post acute ...
3:14
as an umbrella term, to cover all the things that are happened to people, because they had covert in the past.
3:23
So, this would include things such as long code, which is what you hear about in the newspapers, condition, Oppose viral condition of people do not get better from their acute infection. But it also would include things like any change to one risk of developing, say diabetes, heart disease, dementia, stroke going on in the future. So, that's the term we use, post acute ... as an umbrella term. As the next slide, please.
3:53
I'm going to talk talking about the issue of long covert, which of these persistent symptoms that occur, usually during the infection and then don't get better.
4:03
Sometimes, they get a little better, and then they and then they plateau, but they can last, for a long periods of time, without exactly sure how long they can actual, alas, going out, but certainly there are people, but when effective now, for over a year, sometimes up to two years now.
4:20
So these symptoms of ... are really cacophony of a whole bunch of different things. They usually occur in clusters. Most people have multiple symptoms, average, 7 to 13 symptoms and they fall into these major areas. So there are some that we call neurologic.
4:38
These are most most troubling our difficulties with the rapidity of your thinking processes.
4:45
Moving from one mental activity to another, very quickly, Goes under the name brain fog.
4:55
There is no such thing as fog in the brain, but as it's this kind of sense that everything is slowed down and everything is harder to do, but there's no loss of function. Like, you don't lose your speech, you don't lose your memory.
5:09
Everything is slower and more difficult, attention is a problem.
5:13
Uh, then, headache is another big problem. Sleep disorder is a big problem. There are also probably this mobility, So most of the people with long ... have this sense of fatigue, which we all understand.
5:29
We've always fatigue, either sleeplessness or say, during, you know, a common cold with a fever.
5:36
Fatigue is very prominent in this cluster, and that limits people's activities. They're also somebody will have difficulty with their pulmonary system.
5:47
Most of these people are people who had infection in the lungs so they have persistent core, persistent shortness of breath.
5:54
Some of them have abnormalities on their scans, but many their pulmonary function seem to have been normalized, but they're still having these symptoms of shortness of breath.
6:07
When it's because when they exercise, there are some people who develop what we call partial or static tachycardia with palpitations and discomfort in their chest. Next slide.
6:22
That's not all. Unfortunately, there's a whole bunch of other symptoms that can occur. Some of them are related to the GI system of Domino paned, decreased appetite a whole bunch of different than a GI disorders.
6:36
Then gentle symptoms like feeling, muscle pain, Different types of pain syndromes. I mentioned that in the chat, some people will develop a painful neuropathy, flu like symptoms, fever, less common.
6:50
Fatigue we talked about then, you know, if you have, if you had coven, we know what the consequences of coal are.
7:01
Certainly, that creates a lot of anxiety.
7:03
And if you're not getting better at the code, that's going to create even more anxiety, it's not an anxiety disorder, primarily, but, secondarily, covered can create an anxiety disorder, particularly, if you have all these other symptoms thrown in and you really worried about, when am I going to be better? When am I going to be back normal again and weeks, and months go by, so anxiety depression.
7:26
Also, are going to be pretty common in this population.
7:30
Next slide.
7:32
So, how many people are developing this?
7:35
Well, this is a hard question, because it depends a little bit of how you ask the question, and what kind of data you acquire to get your answer, uh, but this is a global look around the world, add the, getting a best estimate of the prevalence of post acute sequelae of covert.
7:57
And you can see here that in younger folks, it's pretty uncommon.
8:02
You know, a couple of percent here and there, Uh, And men age greater than 20, The percentages go up, and these are the different symptoms that people are feeling greater than one symptom clusters in the orange.
8:17
Fatigue is that dark blue, which is, which is pretty common, Respiratory, is that brown?
8:23
And you can see that women in general and most of the studies show a slight predominance, just one more.
8:29
so, as I've seen in other studies, of these persistent symptoms.
8:34
Now of interest in this, in this study, and I don't exact cannot.
8:38
I thought I could figure out how they, where they got the data to get at this. But they tried to estimate duration.
8:44
And they estimated as nine months for those who are hospitalized and four months, for those who are not hospitalized.
8:52
And certainly if you talk to physicians who are taking care of folks who are suffering from these conditions most see that they're on most of the pages are getting better over time. Although some have plateaued and seem to have kind of stagnated.
9:08
Nobody really keeps getting worse, though, so it's not a it's not, like, creating a new disease, It gets worse and worse over time.
9:16
It's either plateauing or getting better as what we've seen so far. But the knowledge is incomplete. Next slide.
9:23
Now, the best evidence that getting at the prevalence and incidence is really comes out of the UK Data and the National Healthcare System, so they can get data, and they've done these surveys, which, And, just to give you an example, of what the issues are and getting at the numbers.
9:42
If you just look at the number of people who have persistent symptoms of, in that class, we talked about 12 weeks, so this is, you know, three months after the acute infection.
9:52
It's 11.7% based on self classification. So just ask people.
9:58
About 11.7% will say yes.
10:02
If you take out, if you take the symptoms, and you ask people, do you have any of these specific symptoms? You get about 5% of people reporting any of the 12 common symptoms that we saw in the previous slides.
10:15
However, if you ask people who didn't get cov it, if they have those symptoms, the prevalence is 3.4% and that Is the key thing to know, is that the symptoms of post covered are not specific to postcode where they occur.
10:29
Very commonly in the population.
10:32
The best estimate is, you ask people, if they have had these symptoms continuously over a period of at least 12 weeks.
10:39
So in the common population, people have these symptoms at any point in time, but they're less frequently going to cover a period of three months, particularly those three months after you got code. That gets you more specificity. It gets to about 3% of the people who've had coven, Arizona 0.5%, in the Control group.
11:01
So, that's why the difficulty there is, in that. And then, you'll see these big differences in estimates.
11:06
But I think this is probably the best data from the UK, which says about 3% of people really have this post viral syndrome. We call log code. Next slide.
11:18
Couple of things about how the infection has changed those change, because the areas have changed, and it's changed, because people are now being vaccinated.
11:28
And, certainly, vaccinations seems to, many studies shows about a 50% lowering risk of developing post acute circlet code.
11:38
So it's all another good reason to get vaccinated.
11:41
Uh, in terms of the variance.
11:46
The thing to know is that the delta variant was the one that got people at the hospitals on ventilators all of those people are going to have long recovery periods with all the symptoms, and they're gonna go on for a year, probably more than a year.
11:59
That's less common now with the, with the, with the auma crime variant.
12:04
But, unfortunately, with our crime, there is still a significant percentage of people who are not vaccinated.
12:11
And even if they are vaccinated, some will develop the symptoms.
12:15
And, again, this is not the most conservative way of approximating but you can kind of see the differences whether your vaccines are not mobile crime versus delta.
12:26
Next slide.
12:28
Uh, maybe go skip that one, go to the next one.
12:32
And so, so the big question is, what's causing this, the problem? The problem is we don't know the answer to that.
12:41
I would say that this is not, the first time we've seen this.
12:45
There are many other infectious conditions where there are some people who develop persistent symptoms and don't get better.
12:53
You may know this is not uncommon when people get Lyme Disease Epstein, Barr Virus infection, mind, and nucleolus and number of other viral diseases, samba less common.
13:04
And there is this condition called ...
13:07
Chronic Fatigue Syndrome, revered As ME CFS.
13:12
Those people generally say that their problem was started after what sounds like some kind of infectious illness, not everyone.
13:18
But the larger proportion of people with ME CFS do give that history, and then they have symptoms that go on, unfortunately, for years or decades. And that can be a very severe disease. So that's the big worry.
13:31
is that post coven May some proportion of people, maybe a small proportion.
13:36
Hopefully, maybe we can stop at this stop at any cost.
13:40
But going on to Develop ME CFS would be a real problem for the country, given the millions of people who have been infected with coven.
13:50
And the people develop post code.
13:53
Now, what's causing it, there's a couple of theories, but we don't really have good evidence.
13:57
one is that there's actually persistent virus in the body, so certain viruses, Epstein Barr Virus is a good example.
14:05
Once you get it, it's a you always have.
14:07
It's hiding and different cells in your body.
14:10
It usually doesn't cause trouble but it is persistent herpes viruses, you know, cold sores, herpes zoster That's that's asked to re-activate a, you know, years and years after the Chickenpox.
14:25
So viruses can stay later than they may, in some instances be active enough to cause the immune system still go after them which were potentially causing symptoms.
14:38
The other thing is there could be viral particles or pieces of viruses that are still in the membranes and they're slowly leaking out.
14:45
There's still an immune response, even though there's no active buyers.
14:49
The other possibility is that you developed auto antibodies due to the co infection as an antibody response, when you have a big antibody response, sometimes it over spills and the antibodies start to recognize normal proteins as viral proteins.
15:06
And then they'll continuously be reacting against these normal proteins and a lot of autoimmune diseases. due to these auto antibodies, so rheumatoid arthritis are good examples, stomach lupus.
15:20
Another example of an autoimmune disorder, where antibodies are reacting against your body.
15:25
And people with those disorders have a lot of the symptoms that people with lung colon have, because your immune system is hyper activated.
15:33
There could be damage to the tissues, particularly in people who have lung problems, infection caused damage, but there could be damaging other tissues as well and taking time to get over and there could be reactivation of other viruses besides a covert like Epstein Barr Virus. So those are the main theories.
15:51
We really haven't been our nail down which of these is the real culprit and it potentially could be different to different people.
15:58
Next slide.
16:00
Just gonna skim through these, so there have been studies, and there are inklings, for each of these theories.
16:07
So here, you can see in blue, these are the controls, and red are the people who have Long coven.
16:14
And these are the different inflammatory markers. And you can see there's maybe some differences, but a lot of overlap. So it's not nothing definitive yet.
16:24
So this was looking at continued immune dysregulation.
16:29
Some evidence but not definitive. Next slide.
16:33
Uh, this is just studies that looked at auto antibodies. So when you have covert, you do develop a lot of auto antibodies. We don't, we don't know, is whether they are now related postcodes syndrome. But we do know that you do develop auto antibodies when you affected with coven.
16:50
Next slide.
16:52
Uh, and this is just an example of the vascular changes that occur encoded.
16:59
And that sum studies show some evidence that some of these vascular abnormalities are persisting of people with post cove it.
17:07
As you know, the virus effects cells that have this particular receptor called the H two receptor and that is on the lining cells of blood vessels.
17:18
That causes a lot of trouble with plotting in the acute code.
17:22
And so, some suggestions and maybe continued trouble with the vascular system. Even in the postcode state.
17:29
Next slide.
17:30
But, again, not, clearly, it's connected to the symptom.
17:35
Then, there's some papers, mostly from animal experiments, maybe some acute coville brain tissue that coven It can affect the inflammatory processes in the brain.
17:49
We don't.
17:50
This is still on the experimental side.
17:53
You don't have good evidence that this occurs in the old code, but it's another potential trouble that might affect brain function.
18:01
Well, I must say that there are many ways where your flame system can get can get geared up and cause all these symptoms without actually causing something happening in the brain as the circulating factors that go to the brain and cause trouble with concentration, memory and sleep and things like that. Next slide.
18:25
Uh, OK.
18:28
There is a one paper which is in press those claiming to see our active virus and people will die months after the covert.
18:38
So, that's, it's not published yet, so it's still not peer reviewed finish.
18:43
But that's a big question of whether there's some continue viral activity and people with post covert.
18:50
Again, not clear that this is occurring in people, no completely recovered, as well as people have post code, but there may be some evidence of continued virus activation months after the covert. Next slide.
19:06
Now, this study is still not published, far, as I know, looking at signs of the viral proteins circulating in these little particle called exosomes that People post coven.
19:18
Uh, now, some of them are also been seen if you don't have the postcode so, but, more commonly in this study that people had long code.
19:27
So, these are the kind of things we're tracking. Next slide.
19:31
And the way we're doing this is through this study called Recover, which is a large NIH study. It's recruited over 10000 people.
19:40
And we are trying to try and get at these potential different causes.
19:47
We're looking at different conglomeration of symptoms and we're trying to develop clinical trials to try and treat the symptoms, but also clinical trials of things like antivirals on the chance that there is still viral activation.
20:03
So I'm getting short on time, so I'm just going to run through the next couple of slides very quickly, but I think I hit the high points here. Next slide.
20:12
This is just progress in the study over time.
20:16
Lots of work going on all across the country not just in the patients that I talked about, but also an autopsy studies, electronic health record studies.
20:25
And people, trying to look at the biology on this line, will encode the next slide.
20:32
And fluoride findings from the electronic health record is looking at the incidence of people in recent times with people who have a symptom eight to 20%, in the non hospital, and hospitalized in four to 8%.
20:50
And the non hospitalized is what this report came out. The next slide.
20:56
Oh.
20:59
And why don't we go? These are the main things I think I talked about that the higher peaks or in the early part of the pandemic vaccination decreases your risk.
21:08
And.
21:13
Next slide.
21:17
These are the trials that were focusing on different symptoms.
21:22
Whether they be the autonomic, the cardiopulmonary asleep or the neurologic going after, but antivirals for viral assistance and then things that would alter immune dysregulation. Next slide.
21:35
No, I think that's it.
21:38
I hope that was kind of a quick overview, where we stand now, in terms of the numbers and the work that's being done to try and understand this, but still so much to learn.
21:48
So, thanks very much for your attention.
21:51
Thank you, doctor ..., for track sharing this update on the current state of their research, and also an update on the recovery initiative.
22:00
Next, we will hear from doctor Kelly Tice, who is a family physician with a background in public health who serves as guide well and Florida Blues, Vice President of Medical Affairs, and Chief Health Equity Officer.
22:14
And this role, doctor Tice, is responsible for creating solutions that improve health outcomes and address health inequities for guideways customers and communities.
22:24
In addition to leading the company's health equity strategy, she has responsibilities and the areas of corporate social responsibility, and public health surveillance. We're so grateful. doctor ... is with us today, to share more about Florida Blues Efforts on Long copan.
22:44
Thank you, I am very glad to be here and have the opportunity to participate in today's conversation. I think doctor ... has really illustrated that there is much yet to be learned about this condition and certainly I'm pleased to have the chance to share from a payer perspective.
23:04
The truth is where long covert is concerned, there are still a great, many unknowns and from a payer perspective, we are uniquely positioned to see impacts across the health care continuum.
23:20
But we're also uniquely disadvantaged because of the, you know, sometimes the lag and data. And the lack of insight. We might have into how things are being managed, decided considered for instance, at the provider level, but. These are good problems to have, because it has forced us to have to be innovative, in terms of our solution ing. Next slide.
23:49
Next slide.
23:52
You may be familiar with Florida Blue as the health insurance arm of guide, one mutual holdings corporation, and that in fact, is somewhat of a parent company, and we consider ourselves a health solutions company. We are a non-profit, and while the insurance arm covers almost six million lives across every county in the state of Florida, our footprint as a company is actually much larger than that. Now, serving 46 million people in, in 45 states, including Puerto Rico and the US.
24:25
Virgin Islands point out, our recent acquisition of triple S is giving us an opportunity to be involved in indirect the care of a number of people on the Island of Puerto Rico, which further expand in particular our efforts to ensure and promote health equity.
24:46
Next slide.
24:49
So, I wanted to start with a review of how we framed and shaped our response to cope at 19 in general.
25:00
In fact, it was very early in the pandemic that once we had moved our than some 10000 or so employees into remote status that we began to focused intently on what our role as a payer needed to be in terms of supporting our members as well as being having positive influence in our communities.
25:24
On the left side, we see our areas of focus and, and, we met challenges and, you know, significant challenges on that side of things, and one, we were, we were working very hard to keep up with data that was sparse initially, that was difficult to validate.
25:44
Certainly, There was a significant delay until we were able to leverage kinked claims data in any sort of meaningful way.
25:51
We, in the interim, really relied on partners, providers, hospitals, and even public health officials to ensure a good flow of that validated data into our system.
26:03
So that we could determine what needed to be done where and how.
26:09
We worked very, very diligently on not just creating messaging, but evolving that messaging as information changed.
26:17
And being really particular about how, that messaging was being targeted to the audiences that that were at risk.
26:25
We used our partnerships with community organizations, both on the non-profit side, public side, as well as in the private sector, at the local level, at the state level, and at the national level, to ensure that we could, we had contact with in connection to thought leaders who were trusted by various areas of community.
26:45
And then, of course, we know we tapped out on every bit of clinical expertise we have within our organization in order to track what was a rapidly changing pandemic.
26:56
We moved through several phases, you know, talked about information.
26:59
And then as soon as testing was available, vetting and validating the accuracy of testing, ensuring that it was available in an equitable fashion. We actually were members of a White House Task Force that was developed to ensure equitable vaccine distribution and, well, ahead of vaccine distribution, We recognized that.
27:17
There was an opportunity for us to use our relationships with minority serving organizations and institutions to build ahead in advance of a vaccine distribution, the messaging and the relationships necessary to deliver both information and vaccines to those at risk communities.
27:39
We also very quickly identified in our own member population, who was at risk, and how they needed to be managed to reduce that risk, And that focus is going to continue throughout the response.
27:52
Each time there was an uptick, in cases, we brought back to the drawing board in terms of how we needed to the final approach to ensuring so having the appropriate impact. Next slide.
28:08
This is the best example best visual I could provide in terms of outfront.
28:15
This happens to be, but we used as we look to distribute vaccine equitably, we have applied this model through throughout the pandemic.
28:27
And Eric, in fact, continue to leverage it for our overall vaccine strategy, as well as public health and health equity efforts.
28:37
So, what you see is a map that was generated out of a social determinants of health dashboard that we created, really, very early in the demo.
28:47
That allows us to identify, by snooty social vulnerability levels, You're able to map, where I remember population is, within, that the geographic areas, can also place on the map T, For instance. So you see here a sort of a retail centers, which become our clinical stops in our communities, and allow us to deliver services to, to the community, out of sort of a storefront. In this particular map. We also mapped Faith faith based Partnerships, which became key relationships that we leverage torsional, if I'm not saying. This was the tool that we use to determine where we were going to allocate resources, with whom we were going to park.
29:34
Frankly, what we said yes to any little to ensure that we were being good stewards of the resources that that we've had in order to contribute to some of the solutions that were necessary, and we can leverage this over and over again through the pandemic with each iteration, in order to be sure that we are meeting our members have a great essay.
29:56
Next slide.
30:02
Doctor Cornstarch talked about the, the vast array of symptoms that explain long term symptoms 10 development and we certainly wrestled with this very early on. We will get there wasn't a code for long hoping for some time after we knew that Post acute Somalia was even a thing. And we began to report screen is what we're seeing in our claims data to try to understand what the experience was of our members related to this.
30:34
Initially, we had only anecdotal reports, because we were very intentional about gathering information from our members, through all of the available touchpoints by the first sources of information for us, was survey responses that we got at the end of the morgans 30.
30:53
So, the webinars that we did, starting in mid 20th, at the end of each of this webinar, as soon as we knew that, that post acute supply was, was a condition for which we needed to be concerned.
31:07
We actually deploy your questions out to all of our webinar participants, and Registrant's asking if they themselves were experiencing such symptoms. And we actually got quite a bit of rich data.
31:19
Aye.
31:20
We couldn't necessarily string all of those systems together right away, But we certainly need that. What we did hearing and seeing recorded across the country was an issue for a number.
31:32
You see there's the definitions that that we use, and we actually, the data I'll show, which is really directional.
31:41
Here's a number of reasons that our data is still somewhat inaccurate, That we use both suspected or confirmed, because we know that there are, there's a learning curve in the provider community in particular, And what we're finding is that very often, numbers are being seen multiple times for a diagnosis of long term, but it's actually being blind.
32:04
And, in order for us to understand, then we have to be able to look back and, and identifying, you know, planes often, even before they've never begins to carry a diagnosis.
32:18
It's critical that also, that we understand that there are large impacts, cardiovascular pulmonary, behavioral health, impacts of being able to characterize this in detail becomes incredibly challenging.
32:30
Next slide.
32:34
I think in correlation with, with what has been seen, what's been presented already. We're seeing high prevalence in females.
32:43
In claims, as well as those with chronic conditions. In fact, the prevalence for those with chronic conditions is actually more than double those without. We also see a higher prevalence in our members who are over the age of 40.
33:00
And, and definitely, we see correlation with those that are living in areas of high social deprivation.
33:08
Password Enter Introductory remarks actually spoke about the disparities that, that are of concern when we talk about ... infection in general and the same risk factors for disparate impacts exist for long as well.
33:24
I'll take you through some of this data again, you know, with a grain of salt, we have to take some of these. But I want to point out a couple of things. You see the increasing frequency of suspected or long, perfect confirmed as age increases. But, if you look there at the younger population, this correlates with some of the impacts that, Sarah, from parents of some of our youngest mammals early in the pandemic as well.
33:54
Next slide.
33:58
I mentioned that chronic conditions were an issue and an invitation.
34:04
here, you see this vast increase in them, the Prevalence of Law coven, and our members, with more than one chronic condition. It is incredibly significant, and this actually aligns with what we saw with perfect hospitalizations.
34:22
And, perhaps, it is, Then, it's good to know that using our approach, in terms of identifying a restaurant, finer members, we were already doing proactive outreach to many of these members. Because we recognize that, if conditions placed an at risk for health, and then we determined that, it also is there risk as long?
34:51
Just wanted to talk a little bit further, valid, or, or data challenges?
34:56
It is, they have been insignificant, and, as most payers, have, we have found, and need to reside somewhere between, you know, what is validated and publicly available, steady proven, but not specific to our members, and what we can gather from our own never population. We've got to do a number of things. First. And foremost, we have to protect our members, which, in many cases, is, our own employees, or team members, as well. So any learnings that, we can gain from any source, certainly is's response. But we also need to be able to predict the impact of long Soviet on on costs.
35:38
And while these, these current data on this is somewhat directionally accurate only, we are seeing a significant increase in member costs for those who have a history of, of having been infected and dealt with, in fact, thousands of dollars in those cases of additional costs in the months that followed that diagnosis.
36:05
And so that's certainly something, too, to pay attention to, that we'll talk further about the other economic impacts of long serving.
36:13
But one of the reasons that, that's a great concern is because in a system where we know access is an issue, those costs can be more significant.
36:24
If we are worried about access, if we're dealing with providers, for instance, who aren't sure of the appropriate way to evaluate these, these conditions.
36:35
And, what we're finding, in fact, is that many of them are ordering everything in order to be certain that they don't miss anything, which can be, in a rather inefficient for you to utilize our resources. And one of the other things that, that we attempted to do early on, and we are making, continue to make a part of our, supported our members, is to stay abreast of the Centers of Excellence that has, that have been developed in our state, so that we can direct members to those services. Understanding.
37:08
As soon as I say, that the difficulty and challenges that exist when you have no, 4 or five kind of four areas in the state, where you've got expertise, and other areas of the state that may be uncovered from a clinical professional staff checks.
37:30
When we think about our, our members, and understanding their impact, I mentioned that as soon as we thought long code that might have been a thing, we began gathering information. The other thing that we did fairly quickly, was to pull our team together, and mapped the journey.
37:47
A member who had coven subsequently developed long term symptoms.
37:51
That allowed us to see all along the care continuum where the opportunities were and where the needs for support existed.
37:59
We were able to leverage information that we gathered from our own contact tracing efforts for our employee population, in order to understand the implications of the condition, as well as the limitations of the system, in terms of having access to information about one covert much, less treatment and evaluation.
38:23
While we gathered the information clinically, we understood a few things that there were support, that misleading that the impact and long term debilitation required more mental health support. We leveraged the use of our hotlines are multi-disciplinary care teams to do proactive outreach and provide that support, help them feel heard, connected, cared about while we learned what was happening in the clinical landscape, and work to help, sort of, facilitate linkage into care.
38:59
We, we also did, you know, a number of follow ups with members who had these experiences to better understand what it's like to navigate a system that was sort of defining itself real-time.
39:12
Next slide.
39:18
I'm definitely very, very proud of that slide that you saw at the outset that really talks about how we leverage the data that was available to us in order to really direct and target our responses. The other thing I'm really extraordinarily proud of is our care management approach.
39:33
And we have long had a multi-disciplinary approach to care management for our members who have highest needs in terms of chronic illness or, or other social barriers to health care.
39:45
And we have to continue to leverage those teams in order to meet the needs of our patients are members of or identified, as long proving. Our care management teams actually exist across our state to serve our member population by geographic location.
40:02
And those teams include medical directors, clinical pharmacy leader, social workers, and nurses, and, you know, other skill sets, as needed. And in there, that is a very local approach that is, is present for our members. But, we use the same model to actually contribute similar information support, at the community level, Out of our florida blue Retail Centers.
40:26
Again, multi-disciplinary teams, but with including social workers with who was in embedded.
40:32
But with partnerships with local community organizations and groups, and an understanding of what's happening on the clinical side of things, what our hospital partners doing, what clinics may be opening, that, they may be providing these targeted services, so that we can disseminate that information.
40:50
The other thing that is key and that is new is that we've created a team identified pretty early, that there is a need for someone to be tracking this, changing clinical data and interpreting it and then deploying it across our internal stakeholders. And so our Clinical Pandemic Response Team still exists. I think some would say unfortunately, to ensure that as things change and the appropriate updates are made across our organization, we've got a member service center that's taking them because we have a sales team have sales agents, all of whom need to understand and be able to articulate and respond to you to leverage them to ensure that our members and community leaders have lives today.
41:37
That concludes my my presentation for today.
41:39
I look forward to to the question and answer period, and again, embrace the opportunity to share our perspective as a payer. Thank you.
41:49
Thank you, doctor TACE, for highlighting guide. Ron Florida Bill is leadership and supporting long code that I just wanted to take a quick second to ask. If anyone has dialed in and is listening to the webinar, they could make sure to unmute their phones and others a little bit of background noise happening. So thank you. Next we will hear from Katie back and Debug Kotler. Katie is a non resident senior fellow at the Brookings Institution where she writes about long covert job quality and low wage work.
42:23
Doctor Cutler is currently the ..., professor of applied economics, and the Department of Economics at Harvard School of Government.
42:32
Professor Cotler holds secondary endpoint appointments at the Kennedy School of Government, and the School of Public Health. We're so grateful to have both of them with us today to talk about the economic burden of ....
42:46
Catherine, thank you very much for having us, inviting us here, the fire trucks going by outside. So we're gonna do a true tag team here. I'm gonna, we're gonna pass the baton back and forth a couple of times.
43:00
Depending on the size of the player, I made to skip the entire thing to Katie, but if we could start off with this.
43:08
Thanks. And then to the next one, there are couple of things we want to talk about. We'll talk very briefly about the prevalence, because that was covered in some of the other presentations. And just give you a little bit on that.
43:17
Then we'll talk about the Costs of Long coven. And so we'll do it, at two levels, will talk about that.
43:23
Cost to Individuals and families, and then we'll talk about the aggregate social costs. And finally, we'll come back to the policy choices. That influence cancer.
43:30
If I could jump to the next one, please.
43:34
So first off, in terms of overall prevalence, as you heard it to be at the beginning of the webinar, this is not known extremely well, there are different estimates from different surveys.
43:45
There are different institutes in different countries even with relatively similar acute coby burdens in the US based on recent data from the Household Pulse Survey, as people are you currently suffering from, from symptoms that are low-income and symptoms.
44:00
About 6.5% of the adult population currently experienced as long Kobe, that's about seven.
44:05
billion adults.
44:07
Roughly 85% of those That's the 5.4% say that they have any limitations associated with lung ....
44:14
Then about 25% of the 6.4% or 1.6% in total and have significant limitations. So that's about four million adults that have significant limitations from one code. That's obviously a really large number.
44:30
People suffering here.
44:32
If I could jump, jump.
44:35
The next slide. You look a little bit by age, relative to the total amount of lung coven. It sort of peaks in the late Middle Ages. I don't know.
44:45
Maybe I'm getting my my own age is killing my description of this. Roughly 40 to 5050 to 60, then declines from there. I think, in part, Because co-produce more likely to lead to death at older ages. So the Lung covered component is somewhat smaller, thankfully, at younger ages, the tool is not nearly as big.
45:02
So you see a sort of shape in death, in age.
45:06
And then on the next slide shows you a bit by characteristics of the economy. And the law uncovered is higher among people with fewer years of education, people without a high school degree, those with a high score, some GED or a little bit lower. But then those without a college degree without a BA tend to be higher again. So there's a rough divide in long covert as there is with many things now. And the divide is, sort of between having a college degree, or not having a college degree, And the labor force is working that way.
45:35
And, unfortunately, disease is turning that way, as well. So, that's a little bit on just kind of, how many people have it. As they said, what we're gonna do is, we're going to turn to, what is the Net Impact, both on people and families in the economy?
45:48
So, the first thing I'm gonna do is, I'm going to toss the microphone proverbially to Katie, who's going to pick up from here?
45:55
Thanks. Next slide, please.
45:59
So we're starting with the personal costs, so the cost to patients and to their families.
46:05
And, you know, I think the first and probably most important thing to say, and this echoes what we've heard before it echoes what David just said, is the burden does seem disproportionately on people with a high school degree or less. They are likely to be lower income and experience higher levels of financial insecurity to start with.
46:25
So as we think about the financial impact of long coed, obviously it depends as I sat on underlying financial security and on severity. But there are two elements. The first is that patients with Long coven and their households may see their income decline.
46:40
As has been a theme today, we don't have a definitive answer on the impact of long kovac on work.
46:47
But we know from the UK's very good Office of National Statistics work that Working Age Long coven patients are about 35 to 45%, more likely, to be out of work post infection. Than they were pre infection.
47:03
We also know from a longitudinal study that somewhere around a quarter of long kovac patients have either their employment status or their working hours impacted, and obviously, both can translate into a loss of income.
47:19
At the same time, that some patients and households are losing income, as we just heard from doctor ties, their health costs are rising.
47:27
Again, we don't have a good number. The best proxy might be what we see in ME CFS. As we heard earlier, there are overlaps between some cases of Lung coven, and ME CFS.
47:40
And in ME CFS, we see about $9000 a year in household spending associated with the illness.
47:48
Obviously, that is a huge number, given the US. Median Income.
47:53
And as we think about where that number comes from, it's a few things.
47:58
So one, as doctor Case just mentioned, there are no validated treatments for long ..., or these other infection associated chronic illnesses.
48:09
And so, in many cases, patients are bouncing from doctor to doctor from treatment to treatment, trying to find something that works and to rule out Causes that aren't on coven.
48:21
two, in many cases, people don't have insurance. As we said, this is disproportionately falling on people who are less well off financially. In addition, of course, many people get their insurance through their job, So if you lose your job, you can lose your insurance. Then, finally, in some cases, insurance just isn't covering the tests and treatment that some of the more expert physicians who treat long coed and other infection associated chronic illnesses are recommending.
48:50
Final point, I have heard from a number of people who reached out and said, Yeah, I don't have long Cove Ed. But my partner who was not a breadwinner does.
49:03
But because my partner was the primary caregiver for the family, I have had to reduce my working hours and so it's important to remember that household can lose income even if it isn't the breadwinner. Who is impacted by law?
49:18
Next slide please.
49:25
So if we zoom out from the patients to what does the Net Impact on employment, probably the best analysis was done by Gopi Goda and Evidence Altice from Stanford and MIT.
49:38
And they found that after a week long work absence that was due to acute ..., they say they looked at what happens to people's labor market behavior after a week long health absence that was due to acute covered.
49:53
And they estimate that somewhere between half 1,000,000.75 of a million people have fully dropped out of the labor force as a result of having an acute co-pay.
50:03
And that does not include additional reductions in hours worked, for people who are still in the labor force, after having co bid.
50:13
There are two caveats, as we think about this, as a summary of the labor force impact of lancome ed. First, not everyone with long cauvery took a week off from work when they had acute covered. In some cases, the acute covered symptoms weren't more severe, and in other cases, they didn't have sick leave, and they couldn't afford to take any time off.
50:35
On the flip side, this doesn't tell us why people drop out of the labor force.
50:40
It just tells us that many do, they're having acute ..., it could be due to lack of it. But it could also be, for example, early retirement and a fear of getting over it again.
50:52
So, if we can flip to the next slide, I guess the question then is, where does that leave us on the labor market impact? And the answer is that we don't have a definitive answer.
51:04
What we do know is that it is a non trivial labor market impact, which isn't a surprise given that, as David said earlier, somewhere around four million Americans are currently significantly limited by Long coven.
51:21
I think our best estimate standing here today is that it's probably somewhere between half three million full-time equivalent workers. Or out of the labor force. And when I say full-time equivalent, I don't mean half a million to two million people. I mean, the equivalent of half a million to two million full-time workers. So that would include people who are still working but have had to reduce their hours to decode.
51:50
And now I'm going to flip the microphone back.
51:55
OK, thank you, and let me go onto the next slide.
51:59
So, what we've tried to do is add this up to an aggregate cost long code into the economy.
52:04
And so I want to just give you a brief description of how we did that and then present the results to, and then we'll talk about some implications. So at the economy wide level, there are three costs that we consider.
52:16
The first, the first, is the health loss. That is, people are in worse health as a result of co-pays.
52:21
We can measure that in a usual, sort of cost effectiveness banner, which is we know roughly what the utility associated with having symptoms on cope. It is from other related conditions. We then value that. This is not money lost. I want to come to that.
52:36
This is kind of the lost welfare of not living, less healthy lives. And that's one of the reasons why.
52:43
the way we train earned income is to live better lives. So that's the first part, is the health loss. The second and third are really money that's not earned.
52:51
Because people cannot work, That's the second or money that we have to devote to things other than kind of consumption enjoyment. That's the health spending part.
53:00
So, each of those, if you will, is the loss of GDP, either GDP that's not earned because there are fewer people that are working where GDP. That's not available for consumption of things. That we like, assuming we don't particularly like medical care other than the access healthier.
53:15
And so that's the third of those other things that Katie had mentioned that are really important would not show up in a GDP calculation.
53:22
For example, if you took money from me and gave it to someone else, that doesn't change the GDP of the economy, makes me better or worse off than the other person better off, but that's not it. That's sort of a transfer, more than it, is an aggregate impact. So as an aggregate economic impact, we want to think about these three things here.
53:38
So we've gone about pricing them out, and I'll show you the estimate on the next slide.
53:43
Without going into enormous detail, the total cost that I get is around three point seven trillion dollars.
53:49
To be clear, what that is, is that's the cost based on the number of cases of Long coven to date.
53:56
So assuming that case, that people have Long coven today don't do anything different.
54:01
No new cases in the future, And these cases resolved themselves kind of slowly over time, in the way that's consistent with literature, so they don't all go on forever, but they don't know today.
54:12
And so that, there are three parts to that, the three on the previous slide, the biggest one is the reduced quality of life. But there's a very significant, that is roughly trillion dollar impact on earnings that will occur.
54:25
And then, another half trillion dollar impact through medical spending, which we benchmark for people with, with relatively similar chronic, can be chronic fatigue symptoms.
54:36
I will just note one other macroeconomic point, which is that part of the reason why inflation is high, is, because firms can't hire workers part of the workers. They can't hire a low wage service workers. Remember, those are the same workers that have Long coven disproportionately .... And so I actually think part of our current macroeconomic situation. Now, not all of it, but part of it is the result of long overdue and other things. And it reduced the labor force labor supply of workers who desperately need. So I think there's actually even a bigger impact than this, but I haven't tried to quantify that.
55:06
The final two minutes or so, We'll just talk about implications, so in the next slide, I'll just give one of them, and then I won't pass the microphone back. So first is implications for public policy, one is, we desperately need to know more, And in this was sort of broader.
55:23
Earlier on, doctor ..., we just couldn't the amount that we know about it, is just far far below what we ought to know.
55:31
There's an interesting part, which is this could not have a big impact on SSDI and other forms of disability insurance. So far, we have not seen an increase in SSDI enrollment or applications, which is really quite anomalous.
55:43
Many workers with Long Cove it seemed to be working, whether they will be able to continue doing that and what form that will be able to continue doing. that is going to depend on all sorts of things, including their own personal health as well as what employers are doing. So, there are other sort of, implications here. And to talk about those, let me just pass it to the final time, back to Katie.
56:00
And, next slide, please.
56:04
So, when people ask, what do we do to reduce the economic burden of long ..., I mean the obvious answer, if you think back to, to what David presented and where the, where the cash costs are coming from, not the loss of welfare.
56:19
It's, you have to keep people at work, and that means there are significant implications for how employers behave. This matters tremendously to society. Loss of work, and income is devastating for individuals and families. It also matters to employers. As David said, particularly when it comes to low wage service work, employers are still facing significant challenges hiring, which is impacting their bottom line. So employers are highly incentivized to keep people working, if they can.
56:51
Which means we need better information on what accommodations work for Long coven.
56:56
A few.
56:58
A few that we know. Telework. Obviously, commuting is tiring, physically demanding, and people with long covert don't want to risk getting coven again. Flexibility on working hours and deadlines. More frequent breaks, and particularly for low wage service work, think like food preparation or retail.
57:17
Finding opportunities to let people set, instead of stand, if they have orthopedic and tolerance. And finally, Brain Fog is one of the prominent lancome symptoms, and some workers are finding that prompts are making their jobs easier. So, thanks for example, of printing out recipes for food service workers instead of having to memorize them or posting checklists.
57:41
Unfortunately, not all jobs are easily amenable to accomodation.
57:46
The jobs that are easier to accommodate are jobs like mine that can be done remotely, that are primarily asynchronous, I can work sort of when I want, that are not particularly physically demanding.
58:00
The very people, though, who are in the jobs that have to be in person are synchronous and are pretty physically demanding, are often lower wage workers. Think retail clerks, nursing aides in nursing homes and food service workers. So it is critical that we also have a safety net for people whose covert is too severe and whose jobs just can't accommodate.
58:22
Next slide, please.
58:26
Then, finally, the other piece of, you know, allowing people to maintain economic productivity.
58:32
And obviously, reducing the welfare loss is treatment for people who get lancome it.
58:38
There are a few clinicians, not many but a few who do have experience with infection associated Chronic Illness, ME CFS, which has been mentioned a few times.
58:49
And anecdotally, though, we don't have large-scale trials validating treatment approaches, there are treatments that are helping some Long coven patients. Those who have muscle activation issues, those who have parts, as doctor ...
59:03
mentioned, and a few more what we need are long fluid Leverette: PCPs. primary care physicians.
59:11
Because this is, this is the first point of call for most patients and specialists who not only understand these conditions, and are up to date on the latest treatments, but also critically who take insurance. Today, many of the few, many of the few really expert clinicians in these fields don't take insurance, because the reimbursement model doesn't work for the types of tests, treatments, and appointment times that they are that they are spending.
59:42
So that was kind of a whirlwind at the end.
59:45
But thank you so much for the time and we look forward to well, it looks like maybe three minutes of questions.
59:53
Thank you, Katy and David, for sharing your work on the economic burden. We'd like to just take a quick minute or two to engage and Q&A.
1:00:02
So, I'll ask our panelists to come off mute and back on video. And I wanted to just tee off of your comments, Haiti, about the healthcare workforce, and see if any of our other speakers wanted to weigh on. Especially, you know, the pandemic eliminated our Health Care Workforce Challenges. We're seeing that right now with coven Flu and RSVP.
1:00:27
Do any of the other speakers want to talk about how Long Covert is impacting our frontline workers, whether they have code that are struggling with long covered, or treating those patients? Are you seeing requests from providers for education on treatment? And what sort of public health infrastructure, or other changes do we need, for, The Future, to Accommodate Long coven patients?
1:00:54
Yeah, I would say that now, when the pandemic head clinic started to take care of people coming out of ...
1:01:03
that was expected at the RDS.
1:01:06
They started to fill up with people and never in the hospital.
1:01:09
But those have continued, so there has been a whole new area of science and medicine that's that sprung up in the specialized clinics, but as Katie said, some of these have waiting lists of 3 to 6 months to even get into them.
1:01:23
So it's it started, but it's not scale.
1:01:27
On the other hand, I would also say that the people who had ME CFS pre coded, they always had trouble finding a position to take care of them. Many physicians just ignored the issue, I didn't want, didn't want to deal with it, they didn't understand that.
1:01:43
Now, now it's pretty hard to say that anymore because everybody knows this is a Kobi related issue.
1:01:50
So I think PSAPs are getting more experience and take care of these patients.
1:01:55
But I would say it's, you know, it's really, it's really in its infancy.
1:02:00
So anything that can be done to scale this up is going to be helpful.
1:02:08
And I would just add the importance of remembering that hospitals and clinics are themselves employers.
1:02:15
And so, one of the issues that we're hearing is that, for instance, our hospital providers, their costs, the costs of just paying salaries, is going up, in addition to the, the additional health care across, the, the limitations, and the need to use contracting workers. And that sort of thing, in order to fill those gaps, is, is really impacting hospital systems in a specific way, in terms of their, their financials.
1:02:44
Need to pay the Rehab Physician.
1:02:46
The Association of No Desire to Us, has taken this on, and they said they had some really good guidelines to help physicians, but I think that's something else to put on the table.
1:03:00
And now, we are over time, but I'm gonna take one last question from our audience and ask each of you, if you could just leave us with one of your top items on your wishlist or research that you think are needed to continue to advance the discussion of long copan.
1:03:25
Doctor ..., do you want to start?
1:03:28
Matthew, do I need, I needed medicine, fix this problem?
1:03:36
For me, I would say, you know, we noticed that vaccine uptake correlates with sort of surges of illness spray. And so the uptake of vaccine is really morbidly low, It's a dismal. And as the data continues to prove that, it has an impact on reducing the incidence of lung. Totally just, I wish we could get folks be paying attention to that, and really protecting themselves.
1:04:04
OK, so I agree with the, prior to, I'll just add, thinking about how to maximize the productivity of people who are limited, so that we're not wasting valuable time for people really want to work, and we need to work.
1:04:21
OK, I strongly echo that, and I would like a deeper dive and more research on specifically how this is impacting low wage workers. The workers who we know disproportionately bear this burden and who are probably the hardest to accommodate to understand what type of safety net interventions we might need to put into place.
1:04:44
Well, thank you all for being with us today, and sharing your work and perspectives. Thank you to our audience. Your feedback is important. Please take a moment to complete a brief survey that will open on your screen and after the event, you can access the speaker slides and we will make a recording of the event available. Please also check out other resources on our website and stay tuned for our upcoming infographic on Long Co brand that we'll be releasing and January. Thank you all again for joining us today for this discussion.
1:05:20
Thank you.
Speaker Presentations

Walter Koroshetz, MD
National Institutes of Health

Kelli Tice, MD
GuideWell & Florida Blue
More Related Content
See More on: Health Equity | Coronavirus