Webinar
Maternal Mortality and New Risks to Women’s Reproductive Health
Time & Location
0:04
Good afternoon. I'm Sheree Crute, Director of Communications at the National Institute for Healthcare Management Foundation (NIHCM). Thank you so much for joining us today for this important exploration of the maternal mortality crisis in the United States at a time when we're seeing new limitations on access to reproductive health care around the country. Maternal mortality has been increasing in the US for decades, with the US. Having the highest maternal mortality rate among industrialized nations. In 2010, it was 23.8 deaths per 100,000 live births, a 14% increase from just two years prior. Yet, two thirds of these deaths are considered preventable. A new CDC report released just this week suggests that 84% of these deaths may be preventable in most of the United States. And there are significant disparities and rates. The rate for black women is nearly three times higher than white women.
1:03
Today, we are fortunate enough to have a panel of leading experts in reproductive health disparities, high risk pregnancy, and how restrictive laws may affect maternal mortality.
1:16
They will explore these issues as well as local, state, and national solutions to the problem.
1:22
But before we hear from them, I want to thank Nancy Chockley, president and CEO of NIHCM and the NIHCM team who helped convene today's event. You can find biographical information for our speakers, along with today's agenda and copies of two of our presentations on our website.
1:44
We also invite you to join the conversation about today's event on Twitter: using the hashtag maternal mortality.
1:53
I am now pleased to introduce our first speaker, Dr. Ndidiamaka Amutah-Onukagha. Dr. Amutah-Onukagha serves as the inaugural Julia A. Okra of Maternal Health at Tufts University School of Medicine. Her most recent research focuses on the integration of maternal safety bundles and community based do laws to improve outcomes for black women. She is an expert in community driven participatory research and health disparities. As they relate to maternal health, She leads an annual national conference on Black Maternal Health Inequities. She is with us today to help us understand maternal mortality nationwide, and the disproportionate impact it has on some communities. Dr. Ndidiamaka Amutah-Onukagha?
2:45
Thank you so much for this invitation, and good afternoon, everyone. It's a pleasure to be here with you all. I'm going to chat with you today about maternal mortality and the impact of this on women's reproductive health.
2:56
Next slide, please.
3:00
So here's an outline for our time together. I'm gonna start off with an overview of maternal health disparities, Talk about some of the current issues that we're seeing. What does this mean for addressing this in the future? How do we take action, and then we'll have a collective Q&A at the end.
3:14
Next slide, please.
3:18
So, just to provide an overview of maternal health disparities, next slide, please.
3:25
So data is not looking good. It's actually getting worse. I just saw an article that was published this morning in USA Today, that talks about 83% of maternal deaths are preventable over 80%, And so we see that the data is moving in the wrong direction. According to the data that we have available from CDC, 60 to 80%, as we saw today, of maternal deaths, are preventable maternal mortality rate, collectively, was 17.4, which we know is much higher now. This was in 20 18, so the rates have actually gotten worse over the past three decades.
4:00
Next slide, please.
4:04
So, we know that there are multiple factors, multiple reasons, really complex and interwoven that contribute to these disparities, such as variations in the quality of health care, the timely receipt of prenatal care, the access to prenatal care and health insurance, underlying chronic condition, the impact of structural racism, and how implicit bias shows up in the clinical encounter with the patient.
4:26
Next slide, please.
4:31
So this data was released in February of this year from CDC. We know that 861 women were identified as having died of maternal causes, which was up from the data in 20 19 of 754. So we saw a sharp increase in 170 women over a year, which accounts for the maternal mortality rate in 20 20, 23.8 deaths. Which is up from 20-19, and it's also from the data I showed you before. The rates are even more drastic when you look at them by race, ethnicity, black, non hispanic women, or a 55.3 deaths per 100,000 live births, which is almost three times higher than their white counterparts. And this is for the data that we have available now. And I would like to say that I'm sure that if we were to look at 2021 or even anything preliminarily for 2022, the rates would be higher. They're not going to be any lower than what we're seeing here.
5:23
Next slide, please.
5:26
So, quality of hospital care and workforce diversity. I represent 3% of medical school faculty that are black, And we know that this lack of diversity within the healthcare workforce has direct implications for patient outcomes for the quality of care. We saw research that looked at patient and provider racial concordance. And the impact of that on black newborn's black infants.
5:50
And black newborns are more than twice as likely to die during their first year as Y newborns. I did my dissertation on infant mortality over 10 years ago, and the data will start that.
5:59
It's still the same now, and when we saw that black infants were cared for by black physicians, the mortality rate was cut in half.
6:09
So, we know that this physician- patient concordance has direct implications for one, lowering mortality risk and influence, but also, this plays out in the maternal health space, as well. So just highlighting the impact of creating and sustaining a more equitable and inclusive workforce, and the impact that that could have in trying to reduce some of these disparities that we're seeing in black and brown women. And a birthing process as seen in maternal health and maternal mortality. Next slide, please.
6:41
So what is the reality of racism across the lifespan? How does racism play out in health and how do these maternal health disparities really show up in black and brown birthing people? Well, we know that black women are twice or almost three times more likely to experience it. A maternal death experienced severe maternal morbidity, which is a near miss and a current according to the American Journal of Managed Care For every maternal death. There are about 70 near misses, which is just as egregious. But for black women who really sit at the intersection of race and gender, this creates a series of chronic stress conditions.
7:16
We see higher esthetic load, A higher impact of physiologic stress on the body, which cumulatively over time creates conditions that deteriorate or weather, the physiologic and reproductive health care system Health system of black and brown women. Now this type of stress cannot be avoided by higher education, higher socio socioeconomic status, and the intersection of race.
7:41
And gender is really pronounced and creates an opportunity for one racism to show up in the delivery of healthcare and to the physiologic impact of racism on the black body.
7:52
Next slide, please.
7:57
So, understanding some of the issues that we're seeing in racial disparities, and just really driving home the point about the impact of racism and how access to quality care makes a difference in the delivery of health care, frankly, for our maternal mortality rates as a country. Next slide, please.
8:16
So, we know that when we talk about the impact of racism and today's healthcare delivery system, the history of obstetrics and gynecology is steeped in racism. Someone that was considered to be the father of modern, gotta kind of modern gynecology, doctor J Marion Sims, who performed unethically on consented. Really painful procedures on the bodies of black enslaved women. The ones that we know are Betsy, Lucy, and a narco. And that's how we got to really have the techniques and procedures that we experience today. On a server core exam was conducted a pap smear, a speculum. How do we repair a fistula? In a birthing person, these techniques were, were perfect that, frankly, on the bodies of black and slave women, so this historical context as modern day challenges. We know that black and brown women are seen as having higher pain thresholds and are more likely to have their pain or their symptoms dismissed.
9:14
We saw this in the case of our global superstar Athletes Arena Williams, who almost died postpartum from complications with a blood clot that was forming in her lungs. And when she told her provider to her nurse, I believe that she was having these complications. The nurse told her she was tired and confused and that he should lay down.
9:33
What's most interesting about her situation is that she was being treated for this.
9:37
Prior to pregnancy, it was documented in her medical records that she had a history of blood clots and if she had not really persisted and thought she would have died from the blood clots forming her lungs. So we know systematic segregation and racism shows up, based on race and ethnicity. We know the hospitals and clinics that were once designated for black and other minorities continue to experience significant financial restraints are often under-resourced and properly staffed. And more likely to close the obstetric units. In my hometown of New Jersey trend is considered maternity care, don't write the hustle that I was born. and my siblings were born. And no longer provides obstetric care. So for black and brown women who are already more likely to experience health, disparities have to travel further to receive the care that they need.
10:25
A colleague of mine, doctor Lisa McGregor did some research looking at distance to care and what that means for high risk pregnancies and complications. And we saw that this is literally a life or death matter, right? These issues result in inequities in access to inequality and timely receipt of health care, which are major contributors to these racial and ethnic health disparities.
10:50
And while segregation and discrimination are no longer legal, we know that patients, people that attend these clinics are continue to be discriminated against based on their insurance status. I talked to black and brown working people all the time about the type of insurance that they have. We know the majority of bursts in this country are two people on Medicaid, and how they have to wait longer to be seen. The less likely to be referred to a specialist or to get two types of high risk care. They need FM or other professionals, and these things disproportionately impact non white populations.
11:22
Next slide, please.
11:27
So I'm going to talk a little bit about some of the research that my team and I are doing, and really driving home a set of points that a lot of these factors that contribute to maternal health disparities, one warrant further investigation into require collective community engaged approaches to dismantle. Next slide, please.
11:46
So, more than 30% of rural communities of color, or at least 30 miles away from a major obstetric unit compare with 90% of majority white rural areas. This has tremendous implications for black and brown mothers who are in rural conditions, because there's 60% more likely to die of childbirth related causes.
12:05
Now, the American Hospital Association, who has a definition of maternity care deserts, this is based on access and distance to a hospital, right. This variability that we see in geographic location in groups reflects chronic health conditions and reflects access to care. The majority or more than half of rural hospitals actually have no obstetric facility, and this distance is problematic, if people don't have reliable transportation, are not able to actually get there, and get the appropriate care that they need. And so, we see the pregnancy related mortality ratio by urban rural classification. And this is very problematic, as we're continuing to see more and more hospitals and rural settings closed down, particularly with the obstetric units. Next slide, please.
12:54
So what are the implications of this? And how do we address this in research and community engaged practice? Next slide.
13:04
Well, obviously, systemic racism is baked into the entire fabric of our country, right? And multiple society systems, including housing who have access to housing. How much do people's housing get appraised for? What type of access is available to this? That housing to education system equality, the taxpayer base, the labor market, the criminal justice system, the economy, the healthcare system, right? And when we see systemic racism has created tremendously reduced access and opportunity for many marginalized groups, which plays out in the socioeconomic attainment, the quality of life, and the overall health, for us to really mitigate or try to eliminate these disparities.
13:40
We need to create and sustain healthier and more equitable communities, including the public health and clinical workforce. And we call for inclusive research that whole spaces for the voices of black women, that is intentionally inclusive of these culturally representative communities, So, the R oh one that I'll talk about in a minute. I want six principal investigators across the country to have this funding. And I believe I'm one of the few and one of the youngest African American women to have this funding, and we all know that NIH creates an opportunity for tremendous research and investment. But the funding opportunities for black and brown researchers are slim and so, it's a tremendous honor to be able to shepherd a team and do this work. Next slide, please.
14:29
So some of the research that I'm doing on the next slide, please, I'll talk about, there's two projects I really want to highlight. The R oh one is on severe maternal morbidity and maternal mortality. We're looking at creating a more systematic understanding of pregnancy outcomes for black women who are most at risk of experiencing severe maternal morbidity, or as we know a near miss, and really creating a foundation for the development and testing of future interventions to improve maternal outcomes for all people. And we have three main aims looking at longitudinal Linked Hospital discharge data from ..., which is a really amazing unique database. Here in Massachusetts to characterize Preconception Prenatal, postpartum Hospital encounters among women with ... to really identify and highlight key opportunities where intervention should have happened and was missed and how do we intervene for the next pregnancy and how do we try to create environments where the woman and a breadth in person is not at risk for an ... event? again.
15:25
We're also looking at Maternal Safety bundles and looking at the impact of implementing these safety bundles were focusing on maternal hemorrhage, maternal hypertension, and a racial disparities bundle. And looking at how that impacts the receipt of Quality Obstetric care, working with some of the major hospitals here in the area, and their teams of attendings, residents, nurses, obese to really get at the implementation of fidelity of these maternal safety bundles. And then the third aim of the grant is looking at the impact of community based doula support and how that could potentially and hopefully, so to decrease inequities of SLM among black and white mothers.
16:01
Next slide, please.
16:03
Another grant, other have am, the PI of our talk quickly about, is creating a maternal health equity space to collaborative community partnerships. We have a Community Advisory board that is composed of people with lived experience. People that are funders, people, that are doulas midwives, creating a teaming environment of providers, families in doulas to create and sustain birth, equity, and empowerment. And you know, that grant is really looking at the maternal health crisis from the perception of the birthing person. How does that influence their maternity care choices? How does that empower them as a patient? And we're looking at this through both qualitative and quantitative methods with a focus on community engaged research also centering the role of partners and fathers.
16:47
Next slide, please.
16:50
So as I move towards my clothes, I'll talk. Yeah, next slide, please. As I move towards my clothes, I will talk a little bit about the Mother Lab, hopefully you will follow us on social media, but its mother lab dot org, which is a research lab I started about two years ago. The maternal outcomes for Translational Health Equity Research is the largest lab when a country comprises students, 35 students from undergrad, masters, PHDs, MDs, or racial and ethnic backgrounds all over the country really focused on eradicating inequities and addressing issues. Black will face the research, advocacy, and mentorship to dismantle the systems that perpetuate racism for black women who give birth. Next slide, please.
17:32
Here's some of the goals of the mother lab. And I just want to close quickly with, and I know these slides are available online, so obviously, we're here to train and develop the next generation of maternal Health scholars activists from undergrad to resident to attending through creating strong partnerships. Creating an evidence base. A lot of our research that we publish, blog, scientific journal articles, webinars that we do is all on our website. But creating solution focused research and policy interventions for black and brown birthing people, by training the next generation of leaders in this space.
18:06
Next slide, please.
18:10
And then my newest endeavor, which the mother lab as a part of is the Center for Black and Telehealth and Reproductive Justice. Here at Tufts University School of Medicine. The Center was founded and launched in March of this year, and we have six units, as you'll see on the next slide.
18:25
So, the units of the center include.
18:29
next slide, please.
18:32
So, here's our mission: collective action, maternal health research and equitable access. Our mission really is to foster academic and community engaged research supporting our goals with a focus on black maternal health and the elimination of inequities through a focus on policy, research, training, and equity.
18:50
Next slide, please.
18:53
Here are the six units of Mother Lab, which I talked about: my research lab, research development and grant, funding to keep us sustainable, maternal health epidemiology and data, education and training, community engagement, and a focus on maternal child health policy.
19:08
Next slide, please.
19:11
So, in closing, for us to collectively advance maternal health and well-being, there are a few things we need to do. Next slide.
19:20
one, ensure that communities are better off than when the research began. As a community engaged researcher who sits in an academic institution, that's really important to me. And my team is that the community that we're working with and for is actually stronger, more sustainable, has a better handle on research, And frankly, is more able to address issues from the community level by engagement. Continued engagement. Regular intentional deep engagement of communities, patients, and stakeholders as partners in the research process.
19:52
Creating and framing opportunities for research with the focus on reproductive justice and social justice. Asking how when you're designing and communicating health research, How are we promoting justice for communities? How are we centering the role of communities? And these are particularly important questions to ask because we know that there is a deep seated and well understood mistrust and distrust of the health care system by communities of color for a number of historical and contemporary reasons. But these communities are really the key to unlocking the solutions to maternal health disparities and inequities as we see them.
20:27
Next slide, please.
20:30
So, in closing, here's my contact information. I'm happy to engage further in the Q and A session. Thank you again, to the National Institute of Health Care Management for having me. I look forward to a robust discussion.
20:40
Thank you so much.
20:42
Thank you so much doctor Amitabh ... for that very powerful exploration of the scope and the factors that influence maternal mortality. Our next speaker will be Dr. Sindhu Srinivas, a Professor of Obstetrics and Gynecology and the Director of Obstetrical Services at the hospital of the University of Pennsylvania. Dr. Srinivas is also the vice chair of Quality and safety and the physician leave for Women's Health Service for Penn Medicine.
21:16
Doctor ... research focuses on strategies to improve maternal outcomes and understand disparities in maternal and neonatal outcomes. She also serves on the board of the Society for Maternal and Fetal Medicine. She is going to help us learn more about critical maternal health risks and how they may be impacted by shifts in policy, including two barriers and solutions to reproductive health care just before she began. So I just wanted to make notes. We will have a Q and A at the end. and you can type your questions into the chat. Dr. Srinivas?
21:54
Thank you so much, Sheree. Thank you for having me this afternoon.
21:58
I'm really excited to be here to talk to all of you about this incredible show. You can go to the next slide.
22:08
Specifically about maternal mortality and reproductive health.
22:17
I thought I would just start by kind of framing what a maternal fetal medicine sub specialist is, which is what I practice, and, I guess my, I didn't disclose anything.
22:27
But my disclosures are I am a passionate physician and advocate around this space of, as, as our prior speaker, just talked about, just reducing maternal morbidity, and mortality, and the health inequities that we are.
22:42
The crisis that we're so desperately in and a maternal fetal medicine specialist subspecialist is a critical piece in this broader scope of, um, providing healthcare for women who are at high risk in their pregnancy. And I think, when we say that, it can mean a lot of different things.
23:01
But FM's physicians are physicians who have an advanced knowledge and training and medical surgical obstetrical, fetal and genetic complications of pregnancy and their effects on both the woman and the fetus. So we provide consultations, we also provide co management, except transfers of care.
23:18
So we're kind of critical for the health care and healthcare delivery around high risk pregnancies.
23:24
We also perform a lot of research, particularly in the area of reducing maternal morbidity, mortality, and health inequities, and partner, as our prior speaker talked about, with other community providers, other researchers, and are just part of the large fabric, really advocating and really thinking critically from the provider perspective about this space.
23:48
And what a high risk pregnancy is, from our perspective, is one that, in that term, gets thrown around a lot, which is why I thought it would be important to sort of define it as one that threatens the health or life of the pregnant person or her fetus. So sick women. We know we're getting pregnant.
24:02
So people, pregnant people, have medical conditions that may complicate their health prior to a pregnancy.
24:08
And then additionally, patients who come into a pregnancy healthy may get sick during a pregnancy.
24:16
As we heard from our prior speaker, you know, Serena Williams had a known blood clotting disorder and blood clot history prior to entering a pregnancy and that put her at risk sort of in the current pregnancy. So that includes existing conditions, complications from prior pregnancies that we might want to think about in an addition.
24:35
Pregnancies that are complicated by multiple gestations or twins triplets, and things like that. Next slide.
24:44
So when we shift gears, and really think about the causes of pregnancy related deaths in the United States, and this is older data, but this sort of still holds true. And I know the CDC just put out a new report, cardiovascular conditions. And you can see that's the first bar, the third bar.
25:00
And even going further down the line in the last bar, cardiovascular conditions, complicate a large number of pregnancy related deaths as does infection or sepsis hemorrhage, blood clots, strokes.
25:13
And it's just really important to kind of think about and know that these deaths are happening sometimes, during pregnancy, right after delivery. And actually more than half of them from this new CDC data.
25:26
And previously actually happening beyond the one week postpartum and through one year.
25:32
And so that is the group of deaths that I don't think we fully appreciate as a society, that when we think about maternal mortality, it's actually not just during the pregnancy and right during the delivery hospitalization. But more than half of them are actually happening in that first year after delivery. And so we have a lot of work to do to think about how to really critically address that issue.
25:55
Next slide.
25:57
Yeah.
25:58
And we know that there's really significant results and disparities. And I think this visual depicts it really well.
26:04
I want people to sort of, I think you're going to hear this probably from every speaker today. You heard in the introduction, Black, women face three times the maternal mortality risk! As white women.
26:15
It's egregious. It's really unacceptable, and I think we're all here and it's amazing to see the number of people that are attending this webinar. We're all here from different sectors and to really think critically about what our role is in reducing maternal morbidity, mortality, and despair. Next slide.
26:37
When we think about what the factors are that contribute to this maternal mortality and morbidity crisis and the disparities.
26:44
The buckets that are on the left are not meant to be siloed.
26:48
It's sort of a hierarchical representation where you think about patient level factors, community and neighborhood factors, clinician factors and system factors.
26:58
And they all sort of, you know, really intersect with one another in a hierarchical way to contribute to these terrible perinatal morbidity and mortality outcomes that we're seeing.
27:09
And, as you can see on the left, racism and discrimination, as our, as my previous speaker mentioned, really, kind of, is threaded throughout all of it. And it's really important for us to think about how we're going to dismantle that piece and how all of these different factors.
27:25
I think, historically, a lot of research really focused on the individual, but we know that community neighborhood, clinician factor system factors, all kinds of inter, intersectionality of all of those things really impacts maternal outcomes.
27:39
Next slide.
27:42
So, what are some of the policy interventions for preventing maternal deaths? You know, some of the things that have been happening around the country, and the CDC data that was just published yesterday, or that just came out yesterday, was reporting on these maternal mortality review committees.
27:57
They're starting to really help, but really understanding some of them, there are risk factors, the drivers, whether deaths are preventable.
28:06
Those have been established in nearly every state, establishing perinatal quality collaboratives in order to help move the needle on implementing bundles, Extending Medicaid for a full year postpartum, and really thinking about how to increase access for patients.
28:23
Starting to think about how to report our data stratified by race and ethnicity as a standard way of reporting.
28:29
So we're really critically thinking about this issue all the time participating in the Alliance for Innovation on Maternal Health, which is about implementation of bundles.
28:39
And the two that I'm going to focus on over the next few minutes are thinking about how we evolve payment models to sustain and scale innovative solutions?
28:47
And the importance of making the connections between some of the reproductive health new policies are in effect, and how preserving access to contraception and abortion care is a critical piece in reducing maternal morbidity mortality. Next slide.
29:07
So just for a minute, I'm going to share research that we did developing a bidirectional technology based solution called Heart Safe Motherhood. That was very much directed at an issue that we saw as clinicians where patients developed pregnancy related hypertension or pre-eclampsia, which affects about 10% to 12% of pregnant patients. It can happen in patients that already had known chronic high blood pressure, But often in patients who actually didn't have any history of high blood pressure. Next slide.
29:41
And we know that, our Professional Organization, The American College of OB GYN, and our care guidelines suggest that we should be following women after delivery in that first 7 to 10 days post delivery, to see if they develop severe or dangerous, high blood pressure.
29:58
This was super hard to accomplish as clinicians, and this, you can see, dates back 10 years ago, this work, where we really wanted to try to help these patients.
30:06
We kept seeing patients coming back into the hospital, 1 to 2 weeks after delivery, insignificant, cardiovascular compromise with severe hypertension, and it was just so, so, so frustrating as a clinician to really try to want to help your patients. But trying to figure out, How can we best do this? How do we find, how do we get the blood pressures we need on patients after they are discharged in order to be able to take the best care of our patients? And so you can see from this work from 10 years ago, significant disparities in our ability to really follow up on paper with patients after they are discharged from the hospital, and this was for a variety of reasons that were mentioned previously. Barriers to access to transportation, childcare. All sorts of different reasons that we heard from our patients when we asked and tried to figure out solutions.
30:52
We had multiple strategies where we tried to, you know, think about different staffing models, walk in appointments, text reminders. And none of it really kind of improved, as you can see, in some ways, got worse over those couple of years.
31:04
Next slide.
31:09
So, from that, and in partnering with our patients, and I can't stress enough how important it is in all of this work to really partner with our patients and our community based leaders, community based organizations, to really think about how to think about more broad and holistic solutions, to address maternal morbidity and mortality.
31:29
But this program is a startup summarizing, you know, 10 years worth of work, into this one slide, which is from that initial trial of an office based visit, and expansion of that.
31:42
We partnered with our patients. We asked them to help us figure out the solution and said, you know, we really want it. We need to follow you after you get discharged.
31:50
What do you think about taking a blood pressure cuff home and texting with us? And we'll just send you reminders to see if you can send us your blood pressure. It seems really simple, But we didn't know if it was going to work.
32:00
Patients really engaged with us. We went through a lot of iterative approaches to this model with our patients.
32:06
And from that was Born Heart Safe Motherhood, which is a bidirectional automated texting program, where patients who receive a blood pressure cuff, they're enrolled into a platform that's basic SMS texting. And we chose that and a non wireless cuff purposefully, because it made it accessible to all of our patients. And we performed a randomized trial where we randomized patients to be in this new program once we developed the automated technology compared to what our usual standard of care was.
32:33
And you can see on the graph on the left that Mommy, it went to the arm of patients that actually were in the texting program.
32:41
We were able to sort of follow up on their blood pressure within 10 days and way more patients than we were. In our usual Care arm. We eliminated re-admissions and we even improved that postpartum visit attendance.
32:54
And the next slide.
33:00
What we found was that when we did a specific disparities analysis on our trial data, as you can see on the bar, the graph on the left shows our office visit arm.
33:11
I'm stratified by race, and you can see that black patients had way fewer fewer percent of black patients were able to come to the office.
33:21
And what you see on the right is that we actually, the improvement was much more significant for our black patient, but we were able to actually eliminate the disparities that we were seeing and get those blood pressures. And what we know from doing this now, for the last eight, you know, 5 or 6 years at this, has now been our standard of care.
33:39
About 20% of patients very routinely have severe blood pressures after discharge and need an inn prescription, an adjustment of medicine.
33:49
We now know from other analyses we've done that are under review, that we are seeing a reduction in stroke and other adverse complications, even up to six months after delivery, even though this program is very short-term.
34:02
Because we're detecting these high blood pressure immediately. So we've been really excited to have this be the standard approach for care for women who have pregnancy related hypertension after discharge across all of our pain medicine hospitals. There's five birthing hospitals. We care for 20,000 birth birthing patients every year and we also scale it to several of the hospitals in the city of Philadelphia, and I've been working with other institutions around the country to help scale this program.
34:31
Next slide.
34:33
Hi.
34:36
I think one thing I sort of mentioned about scaling is that one of the barriers to scaling programs like this, and you see my second to last bullet, is evolving payment models to sustainable solutions.
34:49
One of the barriers to scale is that programs like this, which have been developed in partnership with patients, and are shown to be successful at addressing an incredibly important cause of maternal morbidity and mortality, have difficulty scaling because of the lack of evolution of payment models to really sustain and scale these solutions. Because they sort of are out of the box from traditional care delivery models.
35:13
And I really want to sort of emphasize the point that if we, if we're going to make some critical strides in reducing maternal morbidity, and mortality and disparities, we have to all work together across sectors to figure out how programs like this one. And this is one of many programs that I know about around the country that are really trying to be innovative in thinking holistically, being patient centered, partnering with patients, and developing solutions.
35:40
We're about, how are we going to evolve our healthcare delivery system or healthcare payment structure to really incentivize and create opportunity around sustaining and scaling these types of programs?
35:55
Next slide.
35:56
Hmm.
35:58
I'm going to shift gears a little bit and talk briefly about maternal health and reproductive reproductive health access.
36:06
We know that, you know, pregnancy is an inherently risky time in a pregnant person's life.
36:11
And this is particularly true of patients experiencing a high risk pregnancy abortion. I can't emphasize this enough as an essential medical care for patients who develop high risk conditions during pregnancy or who have had preexisting conditions that may be exacerbated during pregnancy.
36:27
And a patient is really 50 to 130 times more likely to die of pregnancy related cause, and from complications associated with abortion.
36:35
And although individuals choose abortion for a variety of different reasons, 6% report maternal health as the most important reason for seeking a flourishing.
36:44
And so the intersection of what's going on in the policy world around abortion access and the recent dabbs decision, Um, you know, it really is reading such worsening, potentially, of our maternal.
37:00
We're already starting to see this and I'll show you one piece of newer evidence and showing kind of what the impact is of policies that are limiting reproductive health access, both to so abortion care and the impact that that's having on maternal health.
37:14
Next slide.
37:17
These are just some examples of high risk conditions that can develop during the pregnancy. Infections, early onset, high blood pressure, and pregnancy pre-eclampsia.
37:25
That condition I was just speaking of hemorrhage or bleeding, cancer can develop during pregnancy.
37:30
You have taken care of many patients that have developed cancer during a pregnancy and examples of preexisting conditions that may increase risk during the pregnancy, include, you know, patients with cystic fibrosis, maybe pre existing cancer, and a variety of these other conditions.
37:45
And this is just sort of a snapshot of some of the different kinds of patient care that have had to make very difficult choices, and to think that these choices are not going to be able to be me. They are no longer in their hands and the impact that that has on their health and on maternal morbidity and mortality cannot be underscored.
38:05
Next slide.
38:08
This isn't a paper that was just published recently just in July around maternal morbidity and fetal outcomes among pregnant women at 22 weeks' gestation or less, with complications in to Texas hospitals after legislation on abortion.
38:22
So, for those of you may not know, Texas had prior to the Dobbs decision back and last fall, Texas had passed some legislation that severely restricted their access.
38:33
And these two hospitals in Texas publish this paper just demonstrating the impact on maternal morbidity and mortality with the forced sort of expectant management when pregnancy related conditions developed. So meaning.
38:48
The red bar shows that after this legislation, there was an increase in severe maternal morbidity and mortality compared to those in the blue bar, which are other states that don't have that same restriction, but have patients with similar conditions where they were able to immediately intervene as was medically recommended.
39:10
We know that these laws, maternal health exceptions, and state laws, are really vague. That has faded and both for patients and providers, and is leading to.
39:26
Next slide.
39:28
This is some research that is unpublished, but is under review.
39:32
So just sharing a really interesting gist sort of landscape of when you look at states by how restrictive their abortion laws are.
39:44
And this is particularly in insured patients with known preexisting cardiovascular conditions. You can see that as states are more restrictive, there is lower rates of pregnancies ending and abortion compared to states that have supportive policy. And this is research done by doctor Alice Abernathy who's a fellow in the National Clinicians How.
40:09
It's been, I think, really impactful in terms of helping us understand the impact of legislative restrictions on maternal health.
40:19
Slide.
40:22
These are multiple smatterings of media articles from June and July since the Dobbs decision. I think, just, again, raising the concerns around the catastrophic consequences to maternal and fetal health, that this decision by, you know, making it unconstitutional for abortion. You're putting it into the hands of states. And there's just so many restrictions now out there. And you can go to the next slide.
40:46
At least 17 states have abortion bands up to 20 weeks gestation. Currently are assumed to be in effect, and this is as of early in September.
40:54
11 of these states, and you can see them on the second sort of paragraph, have total bands, and nine states courts are determining if existing or new bands can take effect.
41:04
So you can see just the impact that these restrictions will have, and are already having on maternal morbidity and mortality in the same sort of sentence that we're talking about, trying to figure out how to improve maternal morbidity, and mortality, and reduce disparities.
41:21
We have legislation and policies that are going into effect all over this country that actually are working in the opposite way.
41:36
And abortion restrictions will also impact the workforce, and, in turn, impact the quality of care available to all patients, whether they need an abortion or not.
41:43
So, you know, just training and education around access to these services when they're needed is a real concern as these restrictions go into effect.
41:54
Next slide.
41:58
Are very committed to advocacy, such that state policymakers care.
42:05
Aye.
42:10
OK.
42:16
Next slide.
42:22
Next slide.
42:24
In conclusion, hopefully, I know that was a landscape of both.
42:29
What an MFA is, the impact of, and the needs around innovative solutions along those as well as the impact of all of these restrictions on maternal health and maternal morbidity and mortality.
42:42
I think we need to consider pregnancy in the context of health more broadly.
42:47
You need to develop and evaluate innovative care delivery models. And we need to evolve payment models to sustain and scale these solutions. I hope this multi sector of people that are on this webinar will really think about the role of all of our sectors in this work.
43:00
Because this is a this is a societal crisis that we all have a role to plan and we need to preserve contraception and abortion.
43:08
And I look forward to questions at the end. Thank you.
43:12
Thank you so much, Dr. Srinivas for sharing that exploration of what clinicians can do and also, the risks that women face, increasingly, that are associated with pregnancy and our new climate. Our next speaker is doctor Admires, the Senior Vice President and Chief Clinical Transformation Officer for the Blue Cross Blue Cross Blue Shield Association, a National Federation of 34 independent community based and locally operated Blue Cross Blue Shield companies. Dr. Myers is Board Certified in Family Medicine and served on the Faculty of the University of Oklahoma. Obstetrics and Gynecology Department. Is key to the work that Blue Cross. The Blue Cross Blue Cross Blue Shield plans around the country are leading to address maternal mortality. We're grateful to have Dr. Myers with us today to share insight and solutions from the Blue Cross Blue Shield Strategy. Dr. Myers?
44:08
Thank you so much, Sheree and thank you to my colleagues who proceeded with the tremendous research that you've all shared, and had great strategies about how to tackle this as well.
44:19
one more bit of color.
44:20
I was privileged in a variety of different roles prior to this to have the opportunity to attend the birth of thousands of black and brown birthing people. And it was just a humbling experience, and I bring some of that to this table as well.
44:38
The Blue Cross Blue Shield Association, as Sheree said, is an organization that represents and convenes the Independent Blues plans across the United States, an aggregate.
44:50
We bring to the table 115 million or one in three Americans.
44:57
This work has evolved over the last several years.
45:02
Next slide, please.
45:06
In 20 20, there was a decision to determine what we as a blue system can do to address the inequities that we're becoming very, very real during the pandemic. They existed long before that but they were being amplified during the pandemic. And the health equity strategy focused on the things that you can see here were vaccines ensuring that they were equitably available.
45:31
Data leadership, being able to get real data on, on our members, on patience and on providers as well to ensure that we could have networks that could support that connection.
45:45
We have a national health equity program, which we're going to dive into a little bit, as well.
45:50
And then discussions about our networks, who's in our networks, and how do we incentivize as doctor Srinivasan, and pay for advances in health and health equity? We did. We grouped together industry leaders into a national advisory panel.
46:07
We've made significant policy and advocacy efforts as well, as both of my colleagues have stated, this can only be done in partnership, these pro.
46:16
These challenges are large enough that no one stakeholder can tackle these alone.
46:22
And so, working together is critical as we move forward. Next slide.
46:28
Back in the end of 2020 and early, 2020, 1, based on data that existed at the time, as is the others, prior to this, we realized that the black and brown women were three times as likely to encounter complications of their pregnancy, that classified as SMS.
46:49
And we declared a public goal to reduce racial disparities in maternal health by 50% in five years now.
46:57
This wasn't just for the bluest members. Well, one in three Americans is pretty material.
47:02
We want to be even larger than that, at our impact through partnership with others, such as those on this call. So this was our bold goal, and this was based on data that we had available to us at the time.
47:18
Next slide.
47:21
Then, we also convened a group of health equity champions from across the blues that focused our efforts on conducting cultural competency, training, and inclusive bias education. It partnered with the March of Dimes to that end.
47:40
Supporting the practice of nurse midwives and doulas, expanding access to material support services such as doulas.
47:46
We wanted to expand that care continuum to include greater coverage into the post-partum era, for up to a year, and then also exit assess provider program opportunities for reducing disparities, such as centers of excellence and incentive programs. Next slide.
48:07
In looking at the literature and looking at our data, we determined that these would be 10 maternal health equity actions that we can take across our blue system.
48:19
Each one of our blues plans right now is vigorously working to implement as many of these that they can at pace, given their local resources and the partnerships that they have with providers in their areas, but they focus on the, the strategic pillars that I've, that I've defined before.
48:38
Next slide, please.
48:41
We also just revisited the data early on.
48:46
Others have spoken about the fact that the, the, the data, and, uh, data points that have been described so far have been based on available data up until 20 20. Well, we have dug deeper and have now found data that includes part of 2021 from across our 115 million members, we also added a National Medicaid dataset into our analysis.
49:13
We also surveyed our members and analyzed their experiences based on patient reported data.
49:20
Additionally, we did an analysis of SMN using our definition that the traditional definition of SMN by the CDC oftentimes gets reported based on discharge data alone and given the fact that a significant percentage of of uh, adverse outcomes occur in the post-partum period, we felt like it was important to include those in our analysis.
49:47
So we have advocated too NQF and others to extend that ... standard to going into being inclusive of events up to six weeks postpartum.
49:59
And for the purposes of a research study that we are about to release this week, that's the analysis that we're bringing to bear from across our 115 million members and a national data set for Medicaid.
50:12
Next slide, please.
50:15
What did we find?
50:16
We found that SMS rates over that time period, from where my colleagues had discussed and where we had previously published data, have worsened by 9% in both the commercial and in the Medicaid space.
50:33
That SMS rates are higher among Black Hispanic and Asian women as we have seen.
50:39
And that this holds true for both the Medicaid and commercially insured populations.
50:44
Having commercial coverage, having the financial means.
50:48
And those standing to have commercial coverage is not a buffer against these adverse outcomes. That's really important and underscores many of the things that my colleagues have stated prior to this.
51:00
There are a number of factors that increase the risk of SMN many times over, and those are oftentimes comorbidities, clinical comorbidities that we have found through analysis that exist pre pregnancy that are carried into pregnancy.
51:19
That makes the likelihood of adverse outcomes much, much higher.
51:24
And in our survey findings, we also find that Black and Hispanic women find that they are less likely to be able to make their prenatal visits, and we have two distinctive reasons for that. one would be ease of scheduling, and the other is transportation.
51:37
Let's dig in a bit, Next slide.
51:42
SMN rates amongst the Blue Cross Blue Shield managed Medicaid lives are lower than the national Medicaid rates.
51:50
And the presence, as I've stated of chronic disease burden preceding pregnancy, strongly correlates with higher rates at them.
51:57
one specific risk profile really rose to the top, and we'll see that pulled out in the data in just a moment.
52:04
And that's for women of color, ages 35 or higher with comorbid conditions. We believe, based on these data, that they should be treated as very high risk for ...
52:15
delivered with perinatal support to those end in the type of high surveillance that is necessary to accompany that.
52:24
Compared to white mothers, a significant percentage of mothers of color, again, as we stated, we're not able to complete the recommended number of prenatal visits, a secondary predominantly, self reported data to transportation that scheduling challenges. Next slide.
52:41
So, this shows the arc of worsening of 9%.
52:45
And it has occurred for both the Medicaid population, as well as the commercial data, in our, in our analysis, again, 9% for both for both cohorts.
52:56
Next slide.
53:00
And I want you to look at this one.
53:01
This shows the commercially insured SMN rate for, what, 10000 berths.
53:08
Just look on the right-hand side of the screen and look at that pattern. This is the commercial one, then notice where the absolute numbers are, Go ahead and advance to the next slide.
53:20
What you see there, is that the pattern is absolutely the same, whether they be in Commercial Insurance or Medicaid insurance.
53:29
Again, commercial coverage is not the buffer that many think it is, um, ed, that these outcome trends exist, regardless of payer.
53:39
Certainly, the absolute numbers are a bit higher in the Medicaid population, but that is, do the patterns are the same? Next slide.
53:50
And here's what I was referring to earlier for the commercially insured. Look at the spike there for black women ages 35 who have any sort of co morbidity associated with them.
54:02
There's a huge spike in SMN there.
54:06
And now let's go to the Medicaid data and look at the same.
54:09
Next slide.
54:11
Same spike is observed for that population at that age.
54:16
Next slide.
54:19
And this has to do with the survey data.
54:22
Again, showing the four are the black member surveys, that transportation and scheduling concerns rose to the top as barriers for following through with the recommended series of prenatal visits.
54:35
Next slide.
54:38
So in addition to the top 10 lists that are described earlier, there are certain actions that we propose would be strongly encouraged right now.
54:48
We strongly encourage, and some of this is things that have been known for some time, but it's elucidated by the data that we've presented.
54:56
Management of chronic diseases prior to pregnancy and subsequent to pregnancy is absolutely critical to ensure that women are healthier, and safer to become pregnant as before they move forward.
55:10
Part of that involves extending postpartum care up to a year postpartum, and we're grateful to see a significant movement in the Medicaid space for sure. And we're moving across our PPO coverage as well to include broader coverage for that. It's one of our top 10.
55:29
And if you go to our Blue Cross Blue Shield website, there's a tracker that is published there that shows how this is working in the Medicaid space to move more to come on that We want to.
55:42
Also, we found that women of color are more likely to undergo potentially avoidable cesarean sections and that based on our data and the previously published data as well as this, it leads to an increased likelihood of complications as well.
55:59
We also want to reinforce that that the criteria for plans and providers for what scenarios are high risk for SM, such as that very high risk population of women, of color, who are 35 and older with any comorbidities, really highlights that the data really highlights that as a high risk population and then underscore the that there's significant need for attention to transportation scheduling barriers but we know it's complex.
56:26
As doctor Srinivas said, sometimes even straightforward innovations are not as impactful as we'd hope so. Next slide.
56:37
We come to the area of question and answer.
56:40
I am grateful to say that we will be releasing our Health of America report that delineates this in much greater detail, the update to our dataset and some more about actions that can be taken.
56:52
And as I like to say, none of us can do this alone, but we alone can do our part at. all of this can only be achieved through partnership, so grateful to be a part of this today.
57:02
Thank you so much, doctor Myers, for highlighting the Blue Cross Blue Shield Association's High Impact work, in the national movement, to reduce maternal mortality. We're very tight for time, but we're going to stay on a little bit longer so that we can at least pose general questions to our speakers. These questions came in during the event, and we tried to select two that we think will have, maybe, the broadest interest. The first question is, what can physicians do to help lawmakers and the public understand the quantum, the consequences of restrictive policies on reproductive health? And I will open that to the speakers. I'm not sure who wants to take it.
57:49
I can start a couple of things, and then anyone, you both can chime in too, I will just say use your voice.
57:58
And when I say voice, I mean writing in newspapers like iPads editorials, contacting your local policymakers both at the state and the federal level.
58:09
I think as physicians, we, we are, we don't think of that as being an important aspect of our work.
58:18
Or we sometimes don't think that we have, you know, we're going to be able to articulate what we would like to say. But we have to remember that, as physicians, we are experts in this space, in terms of our, and stories are incredibly powerful.
58:32
Sharing stories of patients and how they're impacted by some of these restrictive policies is just incredibly impactful, and as somebody who's done a fair amount of advocacy work, and does hello visits and has those conversations. They are just so grateful to hear from us. And I cannot encourage people to do that enough, and I think this is the time to really be pretty active in using our voice.
59:00
Yeah.
59:01
Doctor ... on Akaka or doctor Myers suggests something you wanted to add.
59:07
I think that you should have.
59:10
Yeah, she did a great job, it is just that getting the impact of collective efficacy. And frankly, approaching your health care, what the, what, the lens of reproductive justice to mind using your voice.
59:22
And the other question I'd like to ask. But many of the people who attend our webinars are working at the community level, the local, the state level, and they are asking, what are some small wins that we can work towards while trying to achieve the bigger goal of eliminating high rates of maternal mortality?
59:41
Again, I would like to begin. I think small wins are really about centering the role of doulas. In the birthing process, I had to do both of my deliveries, 10 months postpartum and my second child deals are incredibly impactful. And we know the women and breadth of people that have better outcomes and are more likely to initiate sustain, breastfeeding, low, lower rates of C section. So that's a small wind that I would say is really advocating for the reimbursement of doulas and working with ... and labor and delivery process.
1:00:15
Doctor Myers, did you want to add something?
1:00:17
I think I would just echo what you just said. I think that's absolutely critical.
1:00:23
There are so many ways that supporting all women and all birthing people to be able to attend their scheduled prenatal visits both during their pregnancy and then the postpartum period.
1:00:41
You know, anything that we can do from a transportation's standpoint as well, locally, within communities, can be very, very impactful as we've seen.
1:00:50
See, Can I just add one other thing, which is just that 100% agree with everything that was said.
1:00:57
And I would also just kind of say that for community organizations or communities, if you're working in the community, think of partnerships between hospitals and healthcare delivery centers. And the community is so critical. And I think more and more healthcare institutions are trying to figure out ways to have community based advisory boards embedded into their quality and safety work and their health care delivery work.
1:01:21
And I think for community organizations that have the bandwidth trying to kind of initiate, sort of bi directionally those conversations and really trying to integrate a lot of our, a lot of our approaches into, as, as doctor Meyer said, you know, we all have the opportunity to work on this. and have our part to play. But without working altogether, we're not going to achieve the impact that we want. And so, you know, I know that we're in our institution really kind of thinking about how to structure these community advisory boards and really are looking for community partners.
1:01:53
Yeah, I would echo that.
1:01:54
I would just say, we're familiar with the data and the research that shows that about 80% of health outcomes are actually linked to factors called social determinants of health, that are outside of the scope of traditional health care.
1:02:09
So given that, it is outside the, the, the walls, the four walls of hospitals, and the traditional health care delivery system, and that is the realm of the community.
1:02:22
So how do we, within communities, in partnership between the health systems, between community based organizations, work to mitigate that, 80% of health outcomes are really impactful.
1:02:34
That's something that health systems and health providers, and payers cannot do alone.
1:02:39
It takes that partnership outside of our four walls in order to really achieve those outcomes.
1:02:47
To that end, I will ask one last thing. Many, many of our questions ask if there were any on the ground community recommendations, small community recommendations beyond Bath and do as social determinants of health, just different was going to open it to ask if there was anything else you wanted to add in that area before we sign off.
1:03:09
I have two things that come to mind. There's a lot of funding currently available for this initiative and really addressing maternal health inequities to a particular thing the community should be positioning themselves to apply for. one from NIH is the red X community health challenge focused on maternal health, and really geared towards building capacity at the community level. I think that's a tremendous opportunity that's available as part of the larger improvement initiative. And then there's also funding from the Black Lives Matter Alliance and the Birth Justice Reproductive Health Fund, which is geared towards a recurring rolling cycle for funding, so I think there's a lot of resources to help communities who are doing the work. Really Build their capacity and be competitive in this larger grant space.
1:03:56
I think I would ever be, start with your own heart, lead with curiosity, B, um, a good listener.
1:04:05
Oftentimes, when we become passionate and activated to participate in improving things, we lean in and jump in, sort of assuming we understand the problems at hand, and I think it's really important, especially when it comes to issues of diversity and inclusion for us, to learn first.
1:04:26
Listen, first. Seek to understand rather than assume that we do. and that's how trust gets built. That would be my, my only other guiding, guiding force.
1:04:36
Well, thank you. I thank all three of you. Unfortunately, we are out of time. You have been an excellent and wonderful panel. Thank you for being with us today and sharing your very valuable insights on this challenging issue. And thank you to our audience for listening in and joining in our discussion on your feedback is very important to us. So please take a moment to complete a brief survey that will pop up on your screen after the event. You can find other resources on this topic including the BCBS report in a few days and our new infographic on maternal mortality on our website. Thank you, again. And everyone, have a wonderful afternoon. Thank you all. Bye, bye.
The United States has the highest maternal mortality rate among industrialized nations, in 2020 it was 23.8 deaths per 100,000 live births, a 14% increase from just two years prior. For every person in the US who dies because of pregnancy or childbirth, it is estimated that up to 70 more people suffer dangerous or life-threatening complications, yet two thirds of these deaths are preventable.
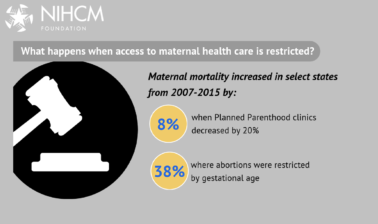
Many experts think the dramatic restrictions on reproductive health care emerging in many states will only increase maternal mortality rates and existing disparities. The rate for Black women is nearly three times higher than White women. This disparity can be attributed to limited access to quality health care, underlying chronic conditions, structural racism, implicit bias, and other social determinants of health.
This webinar explored overall maternal mortality, the impact of changes to reproductive rights, and new approaches and possible solutions that may improve maternal health outcomes. Speakers discussed:
- The state of the maternal mortality crisis, who is affected, and the possible impact of new laws limiting reproductive health care and new approaches to achieving health equity.
- Risks to maternal health, with a focus on high-risk pregnancies and new challenges facing physicians, midwives, and other care providers.
- Supporting equitable, high-quality reproductive health care in all communities.
This webinar is part of NIHCM series: Stopping the Other Pandemic: Systemic Racism and Health.
Speakers

Ndidiamaka Amutah-Onukagha, PhD, MPH
Tufts University

Sindhu K Srinivas, MD
Obstetrics and Gynecology Hospital of the University of Pennsylvania

Adam Myers, MD
Blue Cross Blue Shield Association
More Related Content
See More on: Health Equity | Maternal and Child Health | Social Determinants of Health