Expert Voices
Meeting the Demand for Primary Care: Nurse Practitioners Answer the Call
By: John Iglehart, Founding Editor, Health Affairs
Rapidly expanding insurance coverage and a growing and aging population are increasing the demand for health care services and the personnel who provide them. Despite a robust increase in the supply of physicians following unprecedented increases in medical school capacity in recent years, the Association of American Medical Colleges (AAMC) still projects a shortage of 130,000 physicians by 2025, split almost equally between primary and specialty care.1 At the same time, delivery and payment system reforms may already be changing the mix of personnel needed to respond to the rising demand for health care services. In this essay I consider the potential role that nurse practitioners (NPs) can play in supplementing physician supply, describing trends in the profession and developments related to state laws regulating their scopes of practice (SOP).
Nurse Practitioners "On the March"
Nurse practitioners are one of several types of personnel considered to be advanced practice registered nurses (APRNs); nurse anesthetists, nurse midwives, and clinical nurse specialists are also APRNs. The vast majority of current NPs hold a master’s degree (86 percent) or a doctorate (5 percent) in nursing. As of 2012, there were an estimated 154,000 licensed NPs in the U.S., 127,000 of whom were providing patient care. Slightly under half of those worked in primary care.2 Over the past decade, the annual number of NP graduates more than doubled to reach 14,400 graduates in 2012, and continued growth is expected. One study projects a near doubling of the total NP workforce by 20253 while another predicts the number of NPs providing primary care will increase by 30 percent by 2020.4
The shorter and less costly training pipeline for NPs relative to physicians, combined with evidence that NPs provide high quality care and achieve high patient satisfaction,5,6,7 argue in favor of the profession’s ability to quickly and effectively meet growing demand for health care services. Numerous provisions of the Affordable Care Act – including grants for nurse-managed clinics, significant financial support for NP training, and emphasis on team-based models of care – clearly envision NPs as an integral part of the future health care workforce. Recent evidence points to consumer acceptance of NPs,8 and the profession has strong backing from influential consumer advocates, including the AARP and the Robert Wood Johnson Foundation. Major corporations are also relying on NPs to staff their expanding networks of retail health clinics.
Despite this momentum, however, the efforts of NPs have been stymied in some states by laws preventing them from providing all services they are trained to provide and by requirements for physician oversight. Reflecting long-simmering disputes over “turf” and citing concerns about patient safety and quality of care due to the shorter training period, the American Medical Association (AMA), the American Academy of Family Physicians and their allies oppose SOP expansions and advocate that NPs should provide primary care within the construct of a patient-centered, physician-led team.
The Move to Expand Scopes of Practice
SOP battles are playing out across the country. The National Conference of State Legislatures reports that 100 bills related to NP scope of practice were introduced in 22 states between 2011 and mid-2013, with about one-quarter enacted. The combatants spend enormous sums of energy, money and time arguing their cases before state legislatures at a time when, ironically, collaborative care is seen as the goal at the practice level.
Advocates for NPs wield as their battle cry a 2010 Institute of Medicine report that called for state legislatures to eliminate historical, regulatory and policy boundaries that prevent NPs from practicing to the full extent of their education and training.9 The National Governors Association picked up the torch two years later when it recommended that states reexamine their SOP laws for nurse practitioners7 and in a new report this year the Federal Trade Commission agreed, focusing on the anticompetitive nature of physician supervision and collaborative agreement requirements: “Numerous expert health policy organizations have concluded that expanded APRN scope of practice should be a key component of our nation’s strategy to deliver effective health care efficiently and, in particular, to fill gaps in primary care access. Based on our extensive knowledge of health care markets, economic principles, and competition theory, we reached the same conclusion: expanded APRN scope of practice is good for competition and American consumers.”10 Separately, the Department of Veterans Affairs (VA) has recommended permitting APRNs to practice independently in all VA health facilities, even in states otherwise requiring physician oversight of their activities. Though facing stiff opposition from numerous physician groups, this recommendation may enjoy new life in the wake of reported physician shortages across VA facilities.
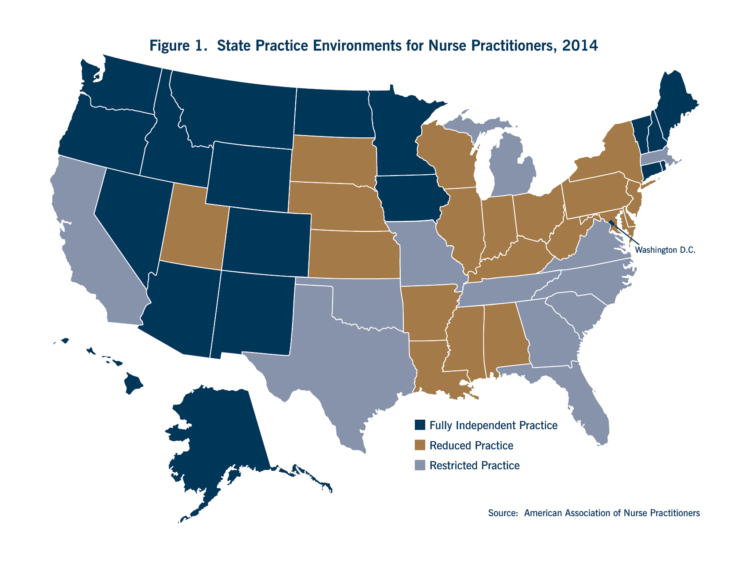
With new laws enacted in Connecticut and Minnesota this year, 19 states plus the District of Columbia now permit fully independent practice for NPs with no requirement for physician supervision or collaboration (Figure 1).At the opposite end of the spectrum, 12 states require supervision, delegation or team management by an outside health discipline (usually a physician) in order for the NP to provide one or more elements of patient care – what the American Association of Nurse Practitioners terms “restricted practice.” The remaining 19 states require a regulated collaborative agreement with an outside health discipline for at least one aspect of patient care (“reduced practice”).
Reimbursement Policy Matters, Too
A recent series of interviews with NPs in six states confirmed the influence of SOP laws but also highlighted the very large impact of reimbursement policies. As the researchers reported: “Payers are in a position to determine what services NPs are paid for, their payment rates, whether NPs are designated as primary care providers and assigned their own patient panels, and whether NPs can be paid directly.”11
Policies governing whether commercial health plans pay NPs directly, the rates they pay, and whether they credential NPs as independent providers in their networks vary by state and by insurer. Some states require direct payment and network inclusion while others leave these decisions to individual carriers.Medicare sets NP direct payment amounts at 85 percent of the program’s physician fee schedule. However, when services provided by an NP are billed under a physician’s name as “incident to” the services of the physician, doctors receive Medicare’s full fee as though they had personally performed the service. Thus, NPs employed by medical practices might be discouraged from billing directly for their services because this generates less revenue for the practice. Medicaid’s NP payment policies also vary by state, with about half of states using the same reimbursement levels for NPs and physicians.
The Shifting Horizon
As nurse and physician organizations wage these SOP battles, there are a few signs that the toxic terrain that divides them may be shrinking a bit in some states and in some pockets of the medical profession. The Connecticut and Minnesota measures passed this year ease the transition by granting NPs more freedom to practice after they have gained experience by working in collaboration with a physician for a defined period of time. This approach has been used by several other states and may be of interest to others. Dr. Steven Weinberger, CEO of the American College of Physicians, told me recently: “The dialogue in the physician community about team-based care and leadership of teams is gradually changing to acknowledge that leadership of a patient care team is not necessarily absolute or rigidly determined. Rather, there is increasing acceptance that roles within a team are often context-specific and driven by the needs of each patient at a particular point in his or her care.” Within the AMA and its network of state medical and specialty societies, physician leaders are evaluating their policies around SOP, concerned that in the face of increasing demand their defensive stance may be losing steam with some legislators. To underscore the unsettled environment, the AAMC’s journal posed as its 2013 question of the year: “What is a Doctor, What is a Nurse?”12 These developments are unlikely to lead to widespread new opportunities for NPs to practice independently, particularly with the growing emphasis on inter-professional and team-based care, but they do reflect an evolving landscape as the health-care enterprise adjusts to the new world of the ACA and restructures the workforce to meet other challenges.
- Association of American Medical Colleges. The Impact of Health Care Reform on the Future Supply and Demand for Physicians, Updated Projections through 2025.” June 2010.
- Health Resources and Services Administration. “Highlights from the 2012 National Sample Survey of Nurse Practitioners.” May 2014.
- Auerbach DI. “Will the NP Workforce Grow in the Future?: New Forecasts and Implications for Healthcare Delivery.” Med Care, 50(7):606-10, 2012.
- Health Resources and Services Administration. “Projecting the Supply and Demand for Primary Care Practitioners through 2020.” November 2013.
- Colorado Healthcare Institute. Collaborative Scopes of Care Advisory Committee. Final Report of Findings. December 2008.
- Newhouse RP et al. “Advanced Practice Nurse Outcomes 1990-2008: A Systematic Review.” Nurs Econ, 29(5):1-21, 2011.
- National Governors Association. “The Role of Nurse Practitioners in Meeting Increasing Demand for Primary Care.” December 2012.
- Dill MJ, Pankow S, Erikson C, Shipman S. “Survey Shows Consumers Open to a Greater Role for Physician Assistants and Nurse Practitioners.” Health Affairs, 32(6):1135-42, 2013.
- Institute of Medicine. “The Future of Nursing: Leading Change, Advancing Health.” October 2010.
- Federal Trade Commission. “Competition and the Regulation of Advanced Practice Nurses.” March 2014.
- Yee T, Boukus E, Cross D, Samuel D. “Primary Care Workforce Shortages: Nurse Practitioner Scope-of-Practice Laws and Payment Policies.” National Institute for Health Care Reform, Research Brief Number 13, February 2013.
- Sklar DP. “2013 Question of the Year: What is a Doctor? What is a Nurse?” Acad Med, 88(1):3, 2013.
More Related Content
See More on: Cost & Quality
