Webinar
Addressing Rural Health Needs: COVID-19, Equity and Access to Care
Time & Location
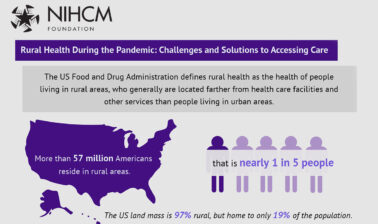
Rural communities have been hit hard by COVID-19. These areas are home to one in five Americans and have seen an increased risk of COVID-19 infection, lower vaccination rates, and additional health care access challenges. Access to care is lower in rural settings due to factors such as travel distance, broadband, and provider shortages. Additionally, these communities report poorer physical health compared to those in large urban areas.
In this webinar, we heard from leaders in the field of rural health who are working to improve the health and well-being of these communities. Speakers discussed:
- Federal health policy focused on improving access, quality, and financing for rural health care and their role in the response to COVID-19
- The pandemic's impact on health care services and steps to ensure digital health equity
- Efforts to address health disparities in rural areas, including establishing equitable COVID-19 vaccine access across Arkansas
0:04
Good afternoon. I'm Cait Ellis, Director of Research Programming at the National Institute for Health Care Management Foundation.
0:10
On behalf of NIHCM, thank you for joining us today for this important discussion on addressing rural health needs.
0:17
Nearly one in five Americans live in a rural area, and these communities can face barriers to accessing care.
0:24
People are generally farther from health care facilities and other services than those living in urban areas.
0:29
And rural communities also report poor health.
0:33
Poor physical health due to factors such as older age and higher rates of poverty.
0:38
COVID-19 has disproportionately impacted rural communities and widened health disparities.
0:43
Rural communities experienced a high death toll due to COVID-19 and have seen lower rates of vaccination.
0:49
As a result of vaccine hesitancy and reduced vaccine access, the pandemic has also exacerbated challenges around accessing care, including through staffing, shortages, and hospital closures.
1:01
Today, we'll hear from a prestigious panel of experts to learn more about rural health challenges and some strategies to improve health and well-being in these communities.
1:11
Before we hear from them, I would like to thank NIHCM’s president and CEO, Nancy Chockley, and the NIHCM team who helped to convene today's event.
1:19
You can find biographical information for our speakers along with today's agenda and copies of their slides on our website.
1:26
We also invite you to join the conversation on Twitter using the hashtag rural health.
1:32
Am now pleased to introduce our first speaker, Tom Morris. Tom serves as the Associate Administrator for Rural Health Policy in the Health Resources and Services Administration of the US. Department of Health and Human Services. In this role, he oversees the Office of Rural Health Policy, which administers a range of research and capacity building grant programs that serve rural communities. We're so honored to have him with us today to share her vision for rural health. Tom?
2:02
Thank you very much, and thank NIHCM for hosting this conference and for focusing on rural health. Really appreciate it.
2:09
Um, with the slides, we'll be using, I'm going to focus a little bit on the federal perspective on rural health, taking a pretty broad view, and then offering a few examples.
2:18
And then, I'll also touch on some of the, saying, a context for rural health, and then, some of the key issues that we're tracking. So, next slide.
2:28
So, I'll start with my office. The Federal Office of Rural Health Policy, is located in HRSA, but it has an interesting role.
2:34
And it says that were charged in the Social Security Act with advising the Secretary on rural issues. And they have a department wide focus on rural health issues. But at the same time, we operate a number of programs, as Cait noted, that are around capacity. Building, that are very much fit into the fabric of HRSA.
2:50
And so, it's a natural home for us to be there.
2:55
So we really try to work both across our agency, and across HHS, in the governmental partners, because given the challenges we know about in rural communities, you know, we're not going to meet them just with our budget.
3:06
So, one of our approaches is to really work with as many of our partners as we possibly can to leverage more resources on behalf of rural communities. And that's what's great about us being part of HRSA, is to get so many of the ...
3:18
programs really do benefit rural communities, either directly or indirectly. And so, I'm talking about programs like the Community health centers, Area Health Education Centers, National Service Corps, the home visiting program. Just to name a few, But we also have other collaborations going on with CMS, CDC, with the National Cancer Institute, and USDA Rural Development Programs there. So, next slide.
3:43
So, as we think about the federal role in rural health, it sort of takes on a number of different shapes in terms of how it's done. There are, obviously, a couple of policy levers that are really critical to supporting rural health care.
3:57
A lot of those are related to payment mechanisms under Medicare.
4:00
So you'll see special designations under Medicare two, take into account the unique challenges rural hospitals have and use reimbursement methodology in order to make sure that they're open. They're financially viable and that they can provide access to care for rural communities.
4:18
At the same time, CMS through its innovation center has also had a number of demonstrations and payment models, like one going on right now in Pennsylvania that looks at a global budgeting system, all with an eye towards, you know, what might the future hold and what's the best way to sort of figure out how to finance and support health care in rural communities.
4:38
Similarly, public insurance programs, Medicare and Medicaid, the Children's Health Insurance Program, are critically important in rural communities.
4:45
And if you look at the patient, mix up your average hospital, your average rural health clinic, they're much more dependent on those public payers.
4:54
They RSA on private insurance, and so that means any change we make in Medicare, Medicaid, or chip policy, has a disproportionate impact on rural communities.
5:03
With the advent of the marketplaces and the subsidies that they offer, we've seen increases in insurance and beginning to chip away at the uninsured rate being higher in rural communities, since all of these are, or ways that we're going about focusing on increasing access to care in rural communities.
5:19
But we also know that access, a big part of it, is having the workforce there to do it. And this has been a longstanding challenge in rural communities.
5:26
And so, you know, HRSA funds a number of grants designed to train future doctors, nurses, dentist, you name it, train them to go out and practice in rural and underserved areas.
5:37
Then we also have loans and scholarship programs that, if they agree to take those, they'll practice in an underserved rural community in exchange for that support.
5:46
HHS and the states also will sometimes support, aren't trained doctors, who will practice in an underserved community in exchange for not having to return to their home country, and they play a really important role in terms of ensuring access to care.
6:00
Then more broadly, you know, you have block grants like the Preventive Health Services Block Grant at CDC, or the Maternal and Child Health Block Grant, or the Mental Health and Substance Abuse Block Grants that are at the Substance Abuse and Mental Health Services Administration.
6:13
And all of those provide states with tools, and especially for rural states.
6:16
They can have flexibility to target those resources to areas of greatest need.
6:21
Sometimes many of those are in rural communities, and so, all of those are really important.
6:26
And then, I think, as we talk more about social determinants of health, people won't necessarily think of, our programs, or the Administration for Children, and Families, or the Administration for Community Living, as key parts of an approach to rural Health Fact, is they are.
6:38
So, for ACF, you know, programs like Head Start and the Community Services Block Grant really play a very important role in addressing the social and human service factors that affect access to care.
6:51
Similarly, the Administration for Community living through its support for programs for the elderly and the disabled, like Meals on Wheels, and Supporting Area Agencies on Aging is another way to get at this.
7:01
And if you move beyond HHS, you have programs like the Department of Labor that does a lot of employment, support to both direct training programs, and then the one stop job centers.
7:11
Housing and Urban Development also plays a really important role in terms of addressing housing to waivers in rural communities. And then the US.
7:20
Department of Agriculture at the FCC, Department of Commerce are now with the American Rescue Plan. You know, administering a significant amount of money to address the broadband gaps.
7:30
All of this is, there's always saying that the investment in rural health sort of runs the gamut across a range of federal agencies.
7:38
Next slide.
7:42
Alright. So I mentioned some of those special payment provisions, and I think this map sort of illustrates the impact of those. What you see here is a map of all the community health centers that are in rural communities. The rural health clinics, which is a payment designation, under Medicare, and then the critical access hospitals. There are 1500 critical access hospitals in this country, and they play an important role in terms of access to care. And they get special reimbursement. benefits, by being a CH, which ensures that that access is supported.
8:09
The Community Health Centers see people regard as their ability to pay, and 40% of the more than 10000 Community Health Center service sites and rural communities, and you add that in with more than just around 4800 rural health clinics around the country, and they really are the backbone of the Safety Net in rural communities.
8:28
Now, all of this happens in communities where we have fewer practitioners, whether it's physicians or nurse practitioners, physician assistants, or help providers. That is in The law has been, there's just not enough of them out there to really provide care.
8:40
We have a mental distribution challenge in this country, and the numbers on this slide sort of reflect that.
8:46
Um, and while we have a number of programs target on it, it's not something that is addressed no, overnight. I am heartened by a number of new approaches. I'll mention one real quick, we've been supporting that.
8:56
The development of more rural residencies in rural communities through a new grant program we have because we have data that shows that, particularly for family medicine.
9:05
You're twice as likely to practice in a rural community if you do your final training in a rural training track.
9:10
So for the past three years we've been investing and growing the number of rural residencies and taking advantage of some flexibility in the Medicare law that allows new residency programs to be started up in rural communities and not be subject to the cap on. Medicare supported real residencies. State Medicaid programs are also doing more in terms of supporting this. So, this is a one part of a larger strategy, I think, that can help to address these issues.
9:35
Next slide.
9:37
Now, the challenges are even more daunting, I think, in terms of access to mental health care in terms of the number of practitioners out there.
9:44
We have 250 rural counties in this country that do not have a psychiatrist or psychologist, psychiatric nurse practitioner, licensed clinical social worker, or even a mental health counselor.
9:56
And so that means the burden falls on top of primary care providers. Unfortunately, sometimes it falls on behalf of the criminal justice system.
10:04
But it's a really long standing challenging situation to, to address. I am heartened by the fact that of those residency programs I just mentioned.
10:15
six of the ones we've supported so far are per site, new psychiatric residency programs in rural communities, and the hope is that they can be an important pipeline moving forward.
10:25
And then, a relatively new program in our Bureau of Health Workforce at HRSA, the Behavioral Health Workforce Education and Training Program, or ..., is also starting to chip away at this, also. Next slide.
10:37
So, you know, given all that, you know, most people are aware of some of the challenges that rural communities face, and none of these should be surprising to anybody.
10:44
But, obviously, in a rural women, have higher maternal mortality rates. We have higher rates of chronic disease. We have greater distance to care, particularly specialty care.
10:54
All this adds up, you know, to it to us, and structural challenges that have been in place for quite some time.
11:01
Next slide.
11:03
So given those challenges, it's not a surprise that rural people tend to die at a higher rate of affordable or excess death, and the five leading causes of death, whether it's cancer, heart disease, injury, mostly driven by opioids, respiratory disease, and stroke. Next slide.
11:19
And the mortality gap is interesting.
11:22
We had a study a couple of years ago that attempted to look at, well, what was driving the gap between it being higher in rural areas, relative to urban areas. And what they found was that drivers were virtually the same.
11:32
It's just that, for whatever reason, they're more determined than in rural areas.
11:35
And so, you know, the challenge is, what do we do about this?
11:39
I know that, that, when you look at this from a national level, how do you move these metrics?
11:43
It's very, very challenging, yet, I know, from our own, investments, in rural communities, and very modest investments that you can empower local towns and areas to address these issues.
11:53
And, last year, we launched new initiative called Healthy Rural Hometown's, designed around addressing the risk factors associated with those five leading causes of death.
12:02
It's a small step, but we're hopeful that it will show results and then wrap it up more dramatically in the years to come. Next slide.
12:11
You know, I think we also have this stereotypical vision of rural America as being largely white and elderly. And, you know, there are certainly parts of the country where that is true.
12:20
And yet, you know, as we think about health, equity and inequity, we have to realize that there's no monolithic view out here and the fact is, rural communities are diversifying just like urban communities are maybe not at the same rate.
12:31
But they are diversifying, and I think this slide, which is from a Brookings study that was released a few months ago, really details this wonderfully in the sense that the more yellow you get on the slides, the higher the rate of diversity in the population. And the reason I wanted to mention this is, because I think it does factor into how we think about solutions, that we have to think about a more diverse population limited, say, 10 or 20 years ago. Excellent.
12:58
So, let's talk about some of the challenges that are front and center for us. I think number one, you know, obviously, is the opioid crisis.
13:05
We know that the past year, the mortality rate from overdose death as unique as increased its increase both in rural and urban areas.
13:14
The opioid crisis is particularly challenging in smaller communities, because they often lack the clinical infrastructure to really deal with it, and then geographic isolation can add to it. And we've been lucky, for instance, 2019, we've had 2018.
13:28
We've had a rural community opioid response program, which is giving money directly to communities to create networks of care, to address the opioid epidemic, but there's no doubt that during the pandemic, as people in recovery were in isolation, it made it much harder to provide services.
13:43
So the overdose death rate increase should not be surprising, even as it is disappointing and so well with many of our grantees went to virtual care, it was not a perfect solution.
13:55
By the way, to deal with this challenge and we're hopeful as we move on to the next phase of the pandemic that we can get back to continuing to try to turn the tide on this one in particular. Next slide.
14:07
We mentioned the impact of the pandemic and code 19 at the outset of the presentation.
14:12
And certainly, you know, it has hit rural communities in a dramatic fashion, and already has been noted, You know, lower vaccination rates, higher case rates, higher mortality, all of which, you know, is, this, is a real concern for rural communities. And it's happened at times with less clinical infrastructure, which is overwhelmed, many rural hospitals, and very many rural clinicians.
14:35
And so, you know, to the, to the administration's credit, when the American Rescue Plan passed, it didn't have anything specifically targeted to rural and the HHS budget, but the administration decided to spend almost one billion dollars to support testing and mitigation efforts in rural health, clinics, and small rural hospitals to support a vaccine hesitant vaccine confidence program for rural health clinics.
14:57
And we also began initiatives to directly distribute vaccines to rural health clinics, community health centers, and to do testing supplies to both of those entities also, as a way to begin addressing some of this. Next slide.
15:10
Josh will talk a little bit more about this. I won't go into much detail, but, but I think most people know we've had a rash of rural hospital closures.
15:17
And the reasons for this are multi-faceted. There's one thing that's driving rural hospitals to close. Part of it is loss of population.
15:24
Part of it is a challenging payer mix, some of it may be market consolidation.
15:28
There's no single solution to this challenge.
15:31
We've been tracking it as part of our policy role, pretty actively, But, particularly since 2010, and during that period, we had 138 rural hospitals closed.
15:41
Uh, so, you know, I think there's no single solution to this one either, and yet, we have a number of programs to support rural hospitals.
15:49
Quality improvement and performance improvement. We are also tracking closely on a new designation that the Centers for Medicare and Medicaid Services will do rulemaking on this year to create a rural emergency hospital, which will be basically a rural hospital with no inpatient beds.
16:04
We don't know what to take up, this will be, but we suspect that it's, it'll be an important option for communities for apps that are big enough to support a full service hospital, but they need more than a clinic.
16:14
And so, we'll see what happens with this moving forward. Next slide.
16:20
We're also facing maternity crisis. Obstetric crisis in many rural communities.
16:25
More than half of rural counties do not have hospitals that offer obstetric services and those gaps are particularly pronounced in communities of color and so you look at this map, the darker the red, the more serious the challenge that we have out there.
16:39
And then again, a number of factors are driving this.
16:43
We are trying to fund some new projects to get out. And we have the Rural Material Obstetrics Management Strategies program.
16:49
And we began this as a pilot with the idea of working regionally and linking together community health centers, hospitals, nurse midwives, healthy start Grantees home, visiting programs, rural health clinics with upstream tertiaries, using telehealth. And we require Medicaid to be part of the network approach that we're using here. But the idea being that if we can improve access, and we can improve outcomes, we can also save money on the Medicaid side. As we do that.
17:15
Think about it, if you just avoided one neonatal intensive care, stay in it for in a state, you basically pay for the entire grant.
17:24
So we have six pilots out right now. And when the budget passes, we'll be moving to have this be a permanent program funded at about $10 million a year.
17:32
And so we hope that that will help at least in some communities begin to address this challenge.
17:37
Next slide.
17:39
And then finally, just a quick word about Telehealth and Josh will cover this in more detail, but obviously, you know, it's always been an important tool in rural communities. What I think we've seen during a pandemic is it's an important tool and not just in rural communities but in many urban communities as well.
17:54
And reflecting that, Telehealth programs all used to be in my office, but they've since moved to become a standalone office in HRSA, and they really are a focal point for telehealth activity, HHS wide.
18:05
They led efforts to create a single website point of entry for telehealth issues at HHS.
18:10
And you can see the address for that webpage on this page. There are also tracking very closely and working with the Department of Commerce oriented implementation of a really record amount of money to address or many broad band gaps in this country.
18:23
And so, with that, I've included a couple of more slides of interest. Obviously, I've covered a lot of ground in a very short period of time, so please feel free to follow up with me on any of this, if you have any other questions, But with that, let me turn it over to Josh. Thank you.
18:39
Thank you so much, Tom, for sharing more about the State of Rural Health in the United States, and highlighting some of the key challenges facing rural communities, and really sharing the federal approach to reducing disparities and addressing the workforce challenges.
18:53
Next, you'll hear from Josh Jorgensen, the government Affairs and policy director at the National Rural Health Association.
19:00
The Association provides leadership on rural health issues through advocacy, communication, research, and education.
19:07
We're grateful, Josh is with us today to share more about rural health needs, digital equity, and their efforts to support rural health across the US, Josh.
19:16
right, well, thank you so much for having me this afternoon, Really appreciate being here, and having this conversation today. So we'll go ahead and get started. As mentioned, I'll touch on you know, a little bit following up with Tom said on what the Rural Health Safety Net status looks like, and then some of the work we're doing on digital, equity and telehealth work at in our HA.
19:38
So next slide, um, know, just a little bit more about who NRHAis. NRHA is a national non-profit membership organization of about 21,000 folks nationwide. We make up a large majority of critical access hospitals, rural health clinics across the country. And my job for the Association is do advocacy on work out here in Washington, which is where I'm based right now.
20:01
So next slide, please.
20:04
Just talk a little bit more about the rural landscape. Next slide.
20:08
So quickly looking, Tom did a really good job pointing this out, but when we talk about rural, we're talking about a vulnerable population, going into COVID-19 certainly has been exacerbated, drought the pandemic.
20:20
Additionally, we've seen systemic workforce shortages kind of kind of crippling rural communities and providers for years. But, you know, as with anything in workforce and in health care over the last year or two, it's been exacerbated.
20:33
And you have that scattered population that has no longer drive times to, you know, get the care they need, and, you know, hospitals that are closing out, unfortunately, large numbers, limited resources for providers. And we do have inadequate, you know, Medicare and Medicaid and private insurance coverage. and that lack of Medicaid expansion. And a lot of states as well, still has kind of herb, that Rural Health Safety net and, you know, lead to some unfortunate closures and more hospitals being vulnerable foreclosure. So, next slide, please.
21:03
Tom spoke on this just briefly, But since 2010, in particular, we've seen 138 rural hospitals close, and that's up this month.
21:12
And you can see, really where, where they're located, unfortunately, is in that southeastern part of the United States, in particular, however, you know, good side of things. What we have seen is that in 20 21, we only saw one rural hospital clubs. And, you know, you could kind of look through the reasonings, but the, the real, the real true reason is a lot of the support that came out of Washington, DC over the last two years. Or, things like the cares Act or the American Rescue Plan, is really kind of help lift that rural health safety net. And, you know, part of our job here at NIH is to see that support continued beyond the pandemic and ensure that we kind of see stability in this rural hospital closures crisis.
21:54
So, next slide, please.
21:56
This is the number that I think is particularly concerning when we talk about rural health and that's the 453 Rural Hospital are vulnerable to closure. So, what does that mean? That means they're operating margins that are similar to those who closed over the last few years. And, again, where do you see that? You will see that the overlap is in a lot of states where we already see that high number of rural hospitals and it closed.
22:21
And you know, it's not just closures that are concerning for rural communities. It's services leaving the community as an alternative, right? So to try to stay open, maybe a service will leave a community, and that leads to a lot of the unfortunate situations that Tom was discussing, where you might have no maternal outcome to deteriorate or mental health outcomes deteriorate. So improving that rural health safety Net is really critical, and a lot of the work that we're doing here in Washington to try to, you know, curve that trend. So, next slide, please.
22:53
This just shows the population health disparity that, you know, Tom was discussing, just a little bit more.
22:59
So what we see is, you know, over 65 graphic here. For percentile, you know, rural is higher. When it comes to that population, we have a higher prevalence of chronic diseases, such as diabetes. Additionally, there's a lower household, median income, lower access to primary care and lower access to mental health care.
23:20
So, you know, just kind of that, that whole, that whole situation, you know, breeds, unfortunate outcome for the Rural Health Safety Net at this time, And next slide, you'll see that where the Safety Net is the weakest, is you see it in those hospitals that have a bone or in a community that has a hospital vulnerable to closure. So, you'll see lower access to primary care in those vulnerable communities, Lower access to mental health, You'll have higher amounts of uninsured adults, Higher amounts of uninsured children, and a higher prevalence of premature death, which is no disturbing, but it happens in those communities where you have a hospital vulnerable. Fortunately, as Tom said, you know, there is this new rural hospital designation, the rural emergency hospital that we do hope will be a lifeline for a lot of these.
24:08
Hospitals that are vulnerable to closure are potentially looking at closing their doors to stay open for that community and ensure that we do have that continued access to care.
24:17
Next slide, please.
24:20
And here, just one more slide.
24:22
Just, you know, showing the, you know, prevalence that we've seen in population over 65. We have a higher prevalence of bad trends, child poverty, diabetes, premature death.
24:35
And unfortunately, we have lower access to primary care, dental health, as well as mental health services in our rural communities compared to our urban and non-metro, non or rural counterparts.
24:48
So next slide, please.
24:51
So now I get to talk about what I consider kind of the, the upside about this that's happened throughout Coburn 19, which is the advancement we've seen in telehealth and broadband services largely over the last couple of months. So, next slide please.
25:05
So, telehealth during ..., know, when we talk to providers at NIH, a lot of times what we'll hear is that, you know, they've been doing telehealth for a long time. It just took a while for policymakers out here in Washington to kind of work on it and advance it. So, at the onset of the COVID-19 pandemic, we saw passage of the Cares Act as well as some movement from the administration through the 11 35 waiver process, and that largely expanded telehealth, virtually overnight, you know, eight allowed for telehealth services be provided by a federally qualified health centers and rural health clinics. Through the 135 waiver process, critical access hospitals were brought into the fold as well as reimbursement for things like audio only services, which is critical. Unfortunately, though, almost all notable telehealth provisions are tied to the public health.
25:55
Now, we can debate when the public health emergency, I'll end, but I think a lot of folks would agree that it's probably closer to ending, then it was the beginning of it. Meaning that, you know, we're really starting our advocacy to look at the true silver lining which has been telehealth and what it's allowed for communities.
26:15
And ensure that it's extended beyond the public health emergency. so that way providers and patients in rural communities are able to have that increased access to care moving forward.
26:24
Next slide, please.
26:27
That said, rural utilization of telehealth hasn't always been at the same level as we've seen in our urban and suburban counterparts, so, according to a recent report, blacken rural beneficiaries had a lower utilization of telehealth compared to white and urban.
26:42
So why is this broadly, first of which is broadband accessibility and availability in communities? And then secondly, would be provider readiness and infrastructure there. So next slide, please.
26:56
When we look at the digital divide in rural America, essentially what we'll see is that rural communities have a lower, lower availability and accessibility to broadband infrastructure at this time.
27:09
However, you know, the Broadband infrastructure bill that just passed Congress last fall and was signed, and the President signed into law by President Biden does provide about $65 billion for broadband connectivity and really good nods to rural communities to ensure build out in our communities. But we are aware that that will take some time. So, next slide, please.
27:33
You know, we're really looking at this as kind of a lifeline, but we understand that the lack of broadband access that we've seen over the last few years, you know, does have, no, does her health care health outcomes, excuse me. So, according to the Robert Wood Johnson Foundation's area with limited broadband access also have higher rates of chronic diseases, resulting in a double burden. So, having that broadband access isolation causes no worse health outcomes. So it's really critical that Congress and the administration ensure that it's, you know, built out in a manner to share these communities have access moving forward.
28:14
Next slide, please.
28:16
On the provider readiness and infrastructure side of things, you know, broad bands huge. We don't go, you know, five minutes without talking to a provider until broadband access comes up. But another is hesitation to invest in the infrastructure needed to have Telehealth and telemedicine. Mainly, because all of these provisions are tied to the end of the public health emergencies, so, you know, you have rural providers that are vulnerable to closure or operating on a super thin margins. They might not be willing to invest in something that is simply looking at coming to an end in April or July. So, that's why we're really saying to Congress, you know, Telehealth needs to be here to stay, and we need to make this signal to folks, but also, to the extent possible, ensure that capital investment funding is always is also there.
29:01
So that way folks who might not have wanted to invest right away or who are still hesitant, have the ability to be part of that 21st, 21st century healthcare delivery system and also ensure that audio only language continues that way.
29:17
Beneficiaries who might not have broadband connectivity are also able to connect.
29:22
Next slide, please.
29:25
So, being out here in Washington, I just wanted to quickly touch on a few pieces of a piece of legislation that we're looking at bipartisan.
29:32
There's a ton of them in this space, but a few just to note versus the Connect Act, and this is a comprehensive telehealth bill that provides a lot of extensions of the county cares Act language, but it does so. It includes permanent extension of language for rural health, clinics and Federally qualified Health centers, but it does it at an updated reimbursement rate. So, it allows payment parity between in person and virtual visits, which is extremely, you know, something we're really looking forward to are hopeful that will be included in legislation that gets across the finish line.
30:06
Telehealth Modernization Act is a bill which, you know, essentially copy and paste what was in the cares Act and makes it permanent with no modifications.
30:14
There's a bill called the Protecting Rural Telehealth Access Act.
30:18
This also allows for payment parody for audio, link health services. And it brings folks like critical access hospitals into the old through legislative text.
30:27
So that way all rural providers are able to be part of part of telehealth and moving forward. And then lastly, a Bill that was just introduces, the Telehealth Extension and Evaluation Act. So this is a two year extension of telehealth services. So as you can see, there's a ton of piece of legislation on this and a lot of debate as to what's happening moving forward. As the NRHA are just hopeful that Congress moves, you know, the telehealth extensions beyond the public health emergency and brings all rural providers into the fold at a level and a reimbursement level that's close to or if not on, on the same level as in person care. So that way all rural providers are able to be part of that.
31:07
Next slide, please.
31:09
So, when will telehealth flexibilities be extended?
31:12
Our hope is that this will happen in this upcoming appropriations package going through Congress, currently the Federal Government's operating under a continuing resolution through March 11th.
31:23
So, we're hopeful that it's an omnibus package and will allow for non-appropriations riders to be included. And with that, you know, we're really hopeful that this silver lining, which is telehealth, can be extended beyond the public health emergency out public health emergency. So that way, rural providers in rural beneficiaries are able to continue utilizing telehealth services.
31:45
Next slide, please.
31:47
So here's my e-mail, and we'd be happy to talk with anybody after the call. So thank you again for having me, and I will pass it along.
31:57
Great, thank you so much, Josh, for highlighting the Rural Health Safety Net, the importance of digital equity, and really the role of and challenges around telehealth.
32:06
Next, we'll hear from Dr. Creshelle Nash, Medical Director for Health Equity and Public Programs at Arkansas Blue Cross and Blue Shield.
32:15
Dr. Nash provides leadership on programs to improve health equity and address health Disparities and Arkansas' Most Vulnerable Communities.
32:23
Work to Improve Health for all Arkansas, includes her role in the Vaccinate, the Natural State Initiative, a collaborative effort to ensure Equitable coven 19 access and distribution.
32:34
We're so grateful to have Dr. Nash here today to share Arkansas Blue Cross and Blue Shield efforts to address health disparities in rural areas. Dr. Nash?
32:43
Thank you. Thank you, and thank you to the audience this afternoon.
32:49
Thank you to NIHCM, and thank you to my colleagues on the panel who have set me up very nicely to talk about rural health as health equity, as a health equity issue.
33:04
And since they have done a good job of an excellent job, actually, of setting the context, just, I'm going to be leaning in really to the local effort to talk about our experience at Arkansas Blue Cross Blue Shield. If you would go forward to the next slide, please.
33:21
In terms of the intersection of rural health and health equity.
33:24
And really talk about our activities through multiple lenses, that includes the leadership, partnership, data driven education, and hopefully, in that, my brief amount of time with you this afternoon to talk about implications and takeaways. Next slide, please.
33:42
So, a bit before we begin about the context of Arkansas Encoded in 19 for me, I think my colleagues have done a good job in setting up some definitions, or some terms that we have talked about, and new part quite frequently in the media, and that it's health, equity, and social determinants. And I just want to be clear, before I begin, what we mean by that. And many of you on the on the call know this, so forgive me for repeating the obvious.
34:10
But the definition that I use for health equity is that health equity means that everyone has a fair and just opportunity to be as healthy as possible. And that really means removing barriers, right?
34:24
It means removing poverty, discrimination, powerless, powerlessness, poor access to jobs, all that stuff, in addition to healthcare.
34:34
So with all those lofty terms, what does that mean?
34:39
That really means that when we are talking about improving the health of communities, we also have to give special attention to those who are at the greatest risk of poor health based on those social determinants. And what are those social determinants?
34:53
Well, you know that definition we also hear is where we live work, and play and pray. Well, that means the context of people's lives. That means safe housing. That means transportation.
35:05
That means tackling discrimination and racism, and violence, and education, and all those different things.
35:12
So that's kind of the definitions that I want to be clear on as I start.
35:18
Now in my context of Arkansas, I'm going to share with you a little bit of a personal context.
35:24
I was born at 28 weeks in rural Arkansas shortly after hospitals were desegregated.
35:31
I have many memories of spending summers with my grandparents, in rural areas, in the country, and now with family and a resilient, tight knit community, and I have wonderful memories of a natural environment.
35:48
That's absolutely gorgeous And it still is, and we still have our challenges.
35:53
Our challenges in Arkansas right now, are for state health rankings.
35:57
We ranked 46th in the nation.
36:00
We have expanded Medicaid but we have a long standing issue with racial and ethnic health disparities.
36:07
And as you've already heard from my colleagues previously, the challenges of rural health and healthcare access, and the impact of the pandemic itself before replays, Next slide.
36:21
So, when I think about health, equity, leadership, as I stated, we have a long legacy, not only in Arkansas, but in the United States, as a whole of systemic and structural racism that influences socioeconomic and social determinants of health, Those resources, the distributions of those resources, including health care resources that ultimately result in racial and ethnic, health disparities, and rural health disparities.
36:51
The COVID-19 pandemic, um, has presented a renewed opportunity, I think, to address these in all of its dimensions, and many of you on the call have been working in this health equity space for decades.
37:05
We know what some of the solutions are, and it's just, now, we have an opportunity, I hope, all the way upstream to the policy level, to actually make some improvements, long term, systemic improvement.
37:19
So, in my role, in the leadership, some of the things that I I'm able to do, is champion health equity, across the board, increasing the knowledge across the continuum.
37:33
And, when I say continuum, what I mean by that is, not only within the healthcare system, in terms of health care quality, and healthcare access, but also link to those social determinants of health, All the way upstream, too, programs, and policies that we, as an organization have.
37:53
And partnerships in local communities.
37:56
And, in that, I'm developing, implementing and attempting to evaluate health equity initiatives set, so that we can ensure that all persons have an opportunity to be healthy.
38:06
Next slide, please.
38:09
So, one, my colleague, made a comment about moving the needle, That's a good question.
38:16
All of these issues have been around for a long time. How do we move the needle?
38:21
I think that data is foundational for the identification and measurement to have an health equity impact.
38:32
And what that means right now, for us, is the collection, not only the collection, but the utilization of race, ethnicity, and language data.
38:41
And urban versus rural status as we identify health, equity, or health inequities to address.
38:48
We also have to have an internal stakeholder assessment, so that we can know where we are as healthcare organizations or as organizations.
38:59
In general, um, the, the health equity framework really has to be infused across all internal silos and that's what we're attempting to do. I'll give you some examples of that in a moment.
39:13
And external stakeholder engagement.
39:15
And as you heard from my colleagues, really, a cross sector partnership, you hard cross sector partnerships from the federal level, across the federal government, Well, the same thing needs to happen to address these complex issues in local communities.
39:30
Next slide, please.
39:33
So, Arkansas Blue Cross Blue Shield has a number of priorities that I have listed here, but the point that I want to make is that health equity is not another silo to be addressed. Health equity is actually infused in all of our priorities and some of them you see here in our covert 19 response, through the Blue and you Foundation, we've awarded two rounds of Rapid Response Grants out in local, rural communities.
40:04
And that could be everything from health care providers' offices to food banks to mobile units to providing personal protective gear during the pandemic and media campaigns.
40:17
When we're looking at maternal health, while we are looking at Maternal Health as a whole in Arkansas, and how we, as a health plan, our value add it, not only for our members, but for the community as a whole.
40:30
We also have to address black, women's maternal mortality.
40:35
With the National Blue Cross Blue Shield Association, we are a part of the strategy to reduce the mortality rate by 50% in five years.
40:45
Big, hairy, audacious goal, but equity, that is equity.
40:50
We also have initiatives in behavioral health, and in the rural health space, specifically, the Blue Cross Blue Shield Enterprise donated significant funds to upgrade digital health networks in Arkansas’s rural hospitals.
41:05
Next slide, please.
41:08
So what does this look like if I'm leaning into and trying to describe to you work where the rubber meets the road.
41:18
How do we advance action through leadership, through partnership, and through data driven education?
41:27
First, I will say, as Medical Director for health equity, I'm always at the table at multiple tables, I would say, trying to ask the right questions.
41:37
And, when I say what the right questions are, it's, What are the barriers that we need to address?
41:44
Who are we missing?
41:46
What are we doing to address health equity, specifically, And are we, are we making health equity worse in what we're doing in our policies and our programs, and then what can we do to mitigate that?
42:01
Also, breaking down internal and external silos, and so, for me, in terms of the health plan or a health plan, that means that health equity has to be infused across multiple silos, whether we're talking about utilization management, case management, disease management, quality management, population health.
42:24
In partnerships, um, we've heard about partnerships at the federal level and at in DC.
42:32
Want to highlight partnerships at the local level, those cross sector partnerships.
42:37
And one of those I want to highlight, is the listening sessions that we have been having in local. rural communities.
42:45
Specifically with minority mayors, just had one last week, actually, with some of some awesome African American women who happened to be mayors of their local towns. And we heard, we've heard many, many things from them. In addition to an update from a quote from ..., in what's going on in local communities? We hear, still hear things about clean water or lack of clean water.
43:10
Lack of sanitation, lack of transportation, lack of digital access, and behavioral health services.
43:17
So, when we have these conversations, it's a combination of the elected officials, minority health care providers, federal FQHCs.
43:27
And it's, we're trying to form and build a true partnership where the voices of those who are most impacted are at the table, not only to define the problem, but to define the solution. And these conversations don't stop at conversations.
43:43
As my colleagues said, we have to bring resources, partnerships that bring resources, and empower communities to solve their problems.
43:52
So, the other, I'm giving you a little bit about leadership. A little bit example of a partnership.
43:58
And I want to focus, just briefly, on the data driven education. And what I mean by that.
44:04
We are working, too, collect and utilize race, ethnicity, and language data.
44:12
And urban versus rural status In our quality measures, That helps us determine where those gaps are, where those inequities are, and find with communities solutions to meet those needs. And, one example of how we have done that and I'll give you some information on that, is focusing in the Delta region in culvert 19 in our Vaccinate, the Natural State.
44:37
Next slide, please.
44:41
So, this is what I'm calling a data driven Case study.
44:45
As you know, the pandemic has been a rollercoaster ride.
44:52
For all of us, including the state of Arkansas, right now, we have 800,000 Arkansans plus, who have been diagnosed with 12 at nineteen over ten thousand, have died to date. And right now, we have a vaccination rate that is about 55% fully vaccinated.
45:11
And just as you've heard from the national level here in the state of Arkansas, Black and Hispanic Arkansans are at a higher risk and continue to have a disproportionate impact of covert 19.
45:26
In that context, Arkansas Blue Cross Blue Shield has invested in what we call Vaccinate the natural state, and that was an overall effort to educate and provide access to vaccines and resources.
45:42
There's a business to business component, but there's also a community engagement component, and in that community engagement component, health equity is infused from the beginning intentionally. And with that, intention, came a focus on the Delta regions, rural regions in the state of Arkansas.
46:01
This partnership really is a Community Health Worker Model partnership, where we have partnered with the Arkansas Faith Network with the Arkansas Medical Dental, and Pharmaceutical Association, which is a multi-disciplinary organization of minority health care professionals and the Arkansas Department of Health, Office of faith based Outreach.
46:25
To provide a Community Health Worker service to local churches who not only care for their communities, but for their congregations. But also their communities at large.
46:38
And we do things like Lunch and Learns to provide updated information, having vaccine evinced vaccine efforts, and to foster co-ordination and collaboration and build capacity in local communities. Because there, there are many organizations that are focusing on the delta at this time.
46:56
And we all need to come together and show up collectively, what we can do to address health equity.
47:03
So, if you go to the next slide, what I'd like to show you is something that we have been doing to keep health equity on the agenda.
47:13
Across the board, in health equity. And this is a, what I've, what I've called a data integration dashboard.
47:19
It's a dashboard in collaboration with the Arkansas Department of Health who has stratified vaccine or vaccine uptake by race and ethnicity.
47:31
And, we have integrated multiple databases to look at that by race and ethnicity, by county, by social vulnerability index.
47:40
And that's the CDC's index, but also overlaid on top of that covert 19 treatment sites, and, as you know, that has been a changing, ever changing effort, whether you're talking about monoclonal antibodies, or anti-retroviral and hospital capacity.
47:58
So, all of this is culminating together to help us identify and focus health equity on health equity. And what I want to point you to on this slide is that if you can see the blue counties are the ones that have a 50 to 60% vaccination rate.
48:16
And those are in some of our most rural counties with the highest minority, or black indigenous people of color.
48:24
In an Arkansas, and you can see we've made some headway there. We have the upper delta to go, but we're also pivoting to make sure that we have that equity lens on treatment sites. So if you hover over one of the treatment sites, you have a phone number.
48:39
You have what's available through the distribution of the Health Department for treatment in these areas, and we're using this to get support for collaborative efforts across the state of Arkansas, to, to officially and formally address health equity.
48:57
Next slide, please.
48:59
So, I know that was a lot of information in a very short amount of time, but if I could sum up implications and takeaways, I think I would say that the intersection of bypass or minority health and rural populations is an equity issue.
49:18
It's a personal issue for me because it's where I come from.
49:22
It's what produced me.
49:24
It's an issue, because I'm a health care provider, and I commit to taking care of individuals and communities.
49:31
But it's also a strategic, and it's a business decision, too, because to improve the health of our population and to decrease healthcare costs, equity must be a part of that.
49:45
Arkansas Blue Cross Blue Shield has made health equity as a priority through those multiple lenses that I went through with you very quickly, through leadership, through partnerships, through education, and data, really, to drive and facilitate collective action.
50:01
I think that health plans and health care organizations really have to be a part of the solution in partnership, in true partnership with local communities, and health equity has to be infused across all functions. And this is not only for covert and covert 19, but really, we are pivoting with these partnerships to coven and beyond.
50:25
So if you're talking about maternal health, if you're talking about behavioral health, if you're talking about diabetes, these are the same core things, and we have an opportunity in this crisis to make significant investments across the nation to improve health.
50:41
And we have a lot more work to do, and that work includes all of us.
50:46
So, with that, I'll stop there.
50:49
And so, thank you.
50:50
Next slide.
50:54
Great, thank you so much, Dr.Nash, for highlighting the intersection of health equity in rural health, and how Arkansas Blue Cross Blue Shield is prioritizing health equity using data and really developing solutions in partnership with the community.
51:10
So, we'd like to use the remaining time to engage in a Q&A session with our audience. Please continue to submit your questions in the Q&A tab. We are working our way through those.
51:19
I'll ask our panelists to come off of mute and back onto video, and I will pose our first question. I'll open this up to everyone.
51:29
We had a few questions, actually, come in around the disability community, and how we can better support families with disabilities in rural areas that often have a unique or different set of needs.
51:55
We'll see if anyone is able to take that.
52:03
OK, we can move on to another, another question.
52:07
We did also have some questions come in specific to the older population and really thinking about telehealth and the disparities in digital access. And I know, Josh, you shared a slide highlighting some of those disparities.
52:22
Can you speak to any of the kind of other innovative solutions for helping older adults access digital, digital resources, online resource directories, or different partnerships that you've seen in place to really help those individuals access care in this digital world?
52:37
Yeah, thank you.
52:39
No. I think when we talk about the, you know, the older Americans with, you know, telehealth, I
think first thing that comes to my mind is the need for the continued audio only.
52:49
I do think that you're talking about a population, you just might not have the wherewithal or understanding of using these technologies right away.
52:57
But then, you know, moving forward, what do we look like?
53:00
You know, I think something, and this goes to working with, you know, the local level, it would be digital literacy classes to ensure folks know how to use things like Zoom, or FaceTime. And you know these technologies that are being entwined into our healthcare in our daily lives.
53:18
So, I think it starts with making sure, audio only here for, you know, the foreseeable future, not only for the broadband access, but also for, you know, the folks who might not understand it, but then moving forward, providing teaching opportunities.
53:31
You know, I don't know the exact entity that would want to do that. Maybe it's health systems would be able to, you know, help work with some of their older individuals, who they're giving care to, or its folks in the communities, but I think that needs to be part of it, for sure.
53:47
And I think the only thing that I would add to that is, you know, I have personal experience with this, with my mother, who is 74 years old and had her first tell a visit, Telehealth visit, and I had to be there with her.
54:00
And, what we've learned, and what the digital solutions that we are, are, our Trumpeting are great, and they're there, but, it can't be an either or.
54:10
For example, we have some communities out there that are using community health workers to help people connect digitally, whether you're at a local library or somewhere where you have free Wi-Fi. So, there are lots of ways.
54:27
two to get at this, but you have to be aware of where the gaps are.
54:33
And I think that, that's one of them and a community health worker model, and we're going to, it can't be either or it's going to have to be a part of that, to support communities at risk.
54:45
Great, thank you, Dr. Nash. We actually had some questions come in around community health workers.
54:50
I'm glad you were able to raise that as another access point for individuals, on the topic of coding and the pandemic, we had some questions around COVID messaging, and rural communities. And if either of you any of you could speak to kind of any advice, especially as we're transitioning to, kind of we're seeing this major lessening of mitigation measures. We're seeing masked mandates change.
55:15
If you have any advice or resources as people are grappling with some of the messaging challenges.
55:23
Oh, it's been, I'll start out and I'll leave time for my colleagues. It has been a moving target definitely as we move through the pandemic is you know, we're flooded with lots of information and so how do you get a message that cuts through. I think that one of the key tenants that I will say is that the messenger matters in local communities that I deal with, we have to be willing.
55:49
The person that's going to deliver the message to look has to look like the community, that we're trying to reach, and actually speak the truth of what we know, and what we don't know, and be willing to answer and talk about the hard questions, which, you know, is lack of access, which is, in some cases, discrimination, and not trusting the healthcare system. We have to be able to have those tough discussions, and be ready for those.
56:21
Yeah, I can't agree more. I think one of the most important things is what you said, which is the messenger really matters, and it needs to be somebody who's trusted by that local community. And that needs to be, you know, defined and folks who are out here in Washington, or in state capitals across the country, who are trying to, you know, increase this vaccination rate need to work hand in, hand with those, you know, trusted local leaders.
56:48
Great, thank you. And that includes minority health care providers if you're trying to reach minority populations.
56:56
Yes.
56:59
We did have a specific question come and I believe this was a map, Josh, that you pulled up, showing kind of the closures and the closures. This individual wrote the closure seem to be closely related to states that have not expanded Medicaid. Has this been evaluated?
57:14
Can you share just some of your thoughts on, or any information you have on the research around that, or if you think that is accurate?
57:24
Yeah, I'd give a quick stab at it. And if anybody wants sales wants to speak to it.
57:27
You know, I think it certainly, you know, I, when we look at the 453 hospitals that I showed where, you know, there's the ones who are vulnerable to closure. You know, we often talk about, you know, the, you know, higher uninsured rate being part of that reason for vulnerable to closure and, and closing. that coverage gap would certainly help, and a lot of these states, and you do see, you know, the states that have an expanded. Medicaid. You know, do have that higher number of hospitals that have closed in rural communities and they also have a higher prevalence of, you know, hospitals vulnerable to closure. They've done some really great research at this with UNC, North Carolina has done some research as well as chartists, and I'd be happy to share that with you, we can just, you know, disseminate that after the call.
58:15
Great.
58:15
That would be fantastic, and we're happy to put up additional resources for many of you on our website, so that people can access that after the event.
58:25
one question, I'll kind of open up to everyone, it seems like there is no single solution to improve health equity in rural America.
58:34
We're seeing questions coming around, LGBTQ health, Native Americans Disability, a lot of subpopulations And so people are really grappling with this challenge.
58:43
So, kind of, in your opinion, what, what do you think is the most critical or urgent to do?
58:48
Or, What would you kind of send our audience off with, kind of as something they can start tackling immediately?
58:59
I'll start big, big question. I'll say, it's not an it's. You know, it's not a single, as you pointed out, it's not a single solution for me.
59:10
It's about, it's about championing equity across the board, even when the spotlight goes away. Because the spotlight is going to go away again, Right?
59:20
And how do we maintain this effort go forward?
59:22
It's got to be partnership cross sector, partnership, the health care system, as we know it, can't do it.
59:32
The things that make you sick have an outside the healthcare system, so we have to have unique, new, public, private partnerships that can get upstream, upstream to the policy level.
59:43
And finally, we have to evaluate what we're doing, so that we can scale up quickly.
59:49
I'll fail quickly and move on.
59:54
Yeah, I think that's absolutely correct. And I think one thing that Tom said, you know, early on, is that, you know, rural America is not just, you know, elder individuals who are white, You know, there's, you know, folks who are African American, Hispanic, LGBTQ, etcetera, and all these communities, and throughout all the different ages.
1:00:16
So, you know, understanding that there's a really big population cross-section between both, you know, health disparities, as well as those ethnic and racial disparities in our rural communities. And first, looking at the data, as Dr.Nash said, and understanding what it is, and then, you know, creating those partnerships, all the way up to Washington, into the various state capitals.
1:00:38
Yeah. I would agree with all that. I think the Brookings study that I referenced is really informative, because there's less current data.
1:00:44
And, you know, even in our small communities, we have divides where sometimes all the people at the table.
1:00:50
And until we have all the folks at the table, you really can't begin to address these.
1:00:55
Know, we can, So often, I think we fall into that trap with looking at disparities and look, yeah, we're happy.
1:01:01
We’ve been happy when they just look at, you know, that it's a national or state level, but they include a rural urban cut, but that, even as far enough.
1:01:07
If we don't then go down and look at sub rural and look at different racial and ethnic populations, we could miss an entire dynamic and then come up with a solution. That only benefits one portion of it.
1:01:18
So, I think the solutions start locally, but we've also got to encourage folks and create incentives to bring everybody in, and to look at the full range of population to serve it.
1:01:30
Great, Thank you so much. Unfortunately, we are out of time today. I'd like to thank our excellent panel of speakers for being with us, for sharing their work, and for our audience joining us for this important discussion.
1:01:42
Your feedback is important, so please take a moment to complete a brief survey that will open at the bottom of your screen after the event, and check out our website for additional resources, including our recent infographic on rural health, And we'll be sure to link to other resources that the panelists mentioned during their presentations. Thank you, all for joining us today.
Presentations

Tom Morris, MPA
Federal Office of Rural Health Policy at HRSA

Josh Jorgensen
National Rural Health Association

Creshelle Nash, MD, MPH, CHIE
Arkansas Blue Cross and Blue Shield
More Related Content
See More on: Health Equity | Coronavirus | Rural Health | Social Determinants of Health