Webinar
Systemic Racism, Disparities and Health: The Impact of COVID-19 on Latino Health
Time & Location
The COVID-19 pandemic has highlighted the synergistic effects of systemic racism, combined with other factors, on the health of Latinos in the United States. Long-standing and ongoing social and economic inequities–including health literacy barriers, disproportionate employment as essential workers, and limited access to employment and insurance benefits–leave Latinos at increased risk of contracting COVID-19 and having more severe cases of the disease. Latinos account for a disproportionate number of cases, are over 4 times as likely to be hospitalized than White Americans, and their share of COVID-19 related deaths is increasing.
The second part in our Stopping the Other Pandemic: Systemic Racism and Health series, this webinar highlighted effective strategies to address the negative impact that systemic racism, the challenges of immigration, language barriers and other factors have on the health and well-being of Latinos. Experts shared actionable, solutions-based approaches that can make a difference at the state and community level, including:
- An overview of the health equity challenges and disparities impacting immigrant, border and Latino communities in the U.S. and increasing their risk of COVID-19
- Grassroots and community efforts and effective methods of supporting uninsured Latino populations, including challenges around mental health and access to care
- A health plan partnership to improve care delivery and their commitment to addressing health access and literacy among Florida’s Latino communities through community workers and outreach
Sheree Crute (00:00:00): Good afternoon, everyone. Thanks for joining us. I'm Sheree Crute, Director of Communications at the National Institute for Health Care Management Foundation, NIHCM. On behalf of NICHM, thank you all for coming to the line today to explore a critical topic at a time when millions of people are facing so many unprecedented challenges to creating a safe and secure life. Our goal today is to offer information and insight on the impact of systemic racism, inequality, and other factors on the health and wellbeing of Latinos living in the United States, especially as those issues relate to the pandemic. Our expert speakers will then offer some actionable paths for change. This webinar is the second in the NIHCM series exploring the links between systemic racism and health inequity among Black, Latino, and other underserved communities in the United States.
Sheree Crute (00:01:00): While every community in the nation is at high risk for COVID-19, Latino people make up just 18.5 percent of the U.S. population, but have 29.5 percent of COVID-19 cases. Latino people from all different parts of the world are enduring a COVID-19 hospitalization rate in the United States that is 4.6 times that of White Americans, with Latinas comprising 44 percent of pregnant women with the virus. We know at least some of the factors contributing to these crisis level disparities. Poor access to care and health insurance coverage, racism, poverty, medical system bias, language barriers, immigration status, and over-representation in dangerous front line worker jobs all play a role.
Sheree Crute (00:01:54): The challenges to making meaningful change are significant, but the prestigious panel of speakers we have with us today are going to make the connection between understanding and exploring these issues, and effective, actionable solutions that can be implemented at the community, state, and health industry level, while discussing methods policy makers, advocates, and healthcare providers can use in the communities they serve.
Sheree Crute (00:02:22): But before we hear from them, I want to thank NIHCM's president and CEO, Nancy Chockley, and the NICHM team who helped convene today's event. In addition, you can find biographical information for all of our speakers, along with today's agenda and copies of their slides on our website. We also invite you to Tweet during the webinar, using the hashtag #latinohealth. We will also take as many questions as time will allow after all of our presentations.
Sheree Crute (00:02:55): I am now pleased to introduce our first speaker, Dr. Lisa Cacari Stone. Dr. Cacari Stone is an Associate Professor of Health Policy at the University of New Mexico, and the director of the Tree Research Center, an initiative dedicated to behavioral health equity. She has worked decades in public health to advance health equity for diverse racial, under-resourced, rural, border, Latino, and immigrant populations. She is going to share an overview of how racism and other forms of inequity affect health among Latino people living in the U.S. and key policy issues.
Sheree Crute (00:03:35): Dr. Cacari Stone.
Lisa Cacari Stone (00:03:38): Thank you, Sheree. Thank you, NICHM, for organizing a much needed conversation and event. I also appreciate to co-speakers on the call today. Mostly, thanks to all of you who have joined. You are on the call and webinar because you do care. You care about our Latino populations and racial inequities.
Lisa Cacari Stone (00:04:01): I wanted to just mention briefly that we have a National Research Center of Excellence. It's taking a second for the slide. Transdisciplinary Research, Equity and Engagement Center. Want to acknowledge the National Institute of Minority Health, Health Disparities, who have funded our center, as well as 12 National Research Centers of Excellence in the nation. Together with our diverse communities in the Southwest, African American, Latino, American Indian, Alaskan Native, Immigrant, Border, we are working to find solutions together.
Lisa Cacari Stone (00:04:37): I just want to mention, Latinos are a diverse population. I also want to acknowledge inclusion. I know the last seminar was dedicated to African American Blacks and COVID. That we are a multi-racial population of peoples. The fastest population growth with U.S. Latinos is from Venezuela, Dominican Republic, and Guatemala and Honduras. Four in five Latinos are U.S. citizens. As Sheree mentioned, while we make up just over 60 million of the population, we represent 18.5 percent of the U.S., but we have a disproportionate impact of 30 percent of the Coronavirus.
Lisa Cacari Stone (00:05:22): This slide illustrates the diversity in geography. As we consider actionable paths moving forward, Latinos make up an increasing portion of COVID deaths in particular state hot spots, Arizona, California, Texas, and Florida. As you see, the increase in deaths were mostly in July. I want to also point out my colleague, Blake [Frazar 00:05:52] with our Tree Center, ran some data for us as part of a new grant we received to do analysis and determine the impact of policies on diverse racial and ethnic minority communities in the U.S.
Lisa Cacari Stone (00:06:10): This chart and slide illustrates... took the top 102 counties in the United States that comprise the majority of Latinos, and then did an analysis of confirmed cases. Here, the strongest predictors of confirmed cases in these cases was obesity, uninsurance, unemployment, percent immigration, and limited English proficiency. As we look at the number of death rates, similar predictors, including poverty and a high percent immigrant and limited English proficiency.
Lisa Cacari Stone (00:06:48): I want to mention here, Latinos in three of our four states in the U.S./Mexico border region had a high percentage of COVID cases and deaths, well in excess of the proportion of the state populations. Again pointing to the importance and urgency of considering State policy and geographic inequalities. As you see, if you look under Arizona, Latinos represent 32 percent of the population, but are well over 40 percent of the cases. Same is true with California, with a large percent of Latinos, and then almost 50 percent of the cases in Texas as well.
Lisa Cacari Stone (00:07:31): I want to highlight this slide of what accounts for this? As we're thinking about actionable steps moving forward, why are Latinos so disproportionately impacted by COVID? In fact, racial inequalities that are preexisting, that represent broader, underlying structural and systemic barriers, include racism and discrimination. This impacts not just individuals, but multiple generations of families and their health and wellbeing.
Lisa Cacari Stone (00:08:05): How do we define and think about structural racism because how we name and frame a problem is how we move forward in terms of actions. racism in an intersectional connection system of oppressive forces that determine health outcomes, including historical, cultural, institutional, interpersonal. They advantage certain populations, including non-Latino White, and produce putative and chronic adverse outcomes. We look at this at the structural, institution, and individual level.
Lisa Cacari Stone (00:08:42): I'm going to highlight just a few predictors of these intersectional vulnerabilities. As we think about structural, I'm going to be talking a little bit about what we need to think about in terms of policies, health, welfare, and immigration policies, institutional forces, including poverty, wealth, employment, and housing, and discrimination.
Lisa Cacari Stone (00:09:07): Here, this slide shows from the Urban Institute the significant importance of not just poverty, but of wealth, by race and ethnicity. Both measures of both average and median wealth are important because it's how Latinos are able to prosper compared to other groups. What it shows here is that African Americans are ten times more likely to not have at least... or Whites are ten times more likely to have wealth than African Americans. And on the right here, as we think about Latinos families, White, nonHispanic families are eight times more likely to gain efforts from wealth. This is important in the time of COVID because your assets and any savings you have could be immediately depleted.
Lisa Cacari Stone (00:10:00): The next slide illustrates the share of Latinos who are lost their jobs due to COVID. As you see, Latinos who are non-citizens, almost 70 percent have lost their jobs, and Latinos who are members or citizens, just almost 50 percent. What does this mean for the daily lives and the generational families? The chart on the right, again from the Urban Institute, shows that almost... that 47 percent of non-citizen Latino family members have had to cut back spending on food, and 40 percent of Hispanic citizens. You'll see other impacts of financial impact on Latino families, including savings, household purchases, and credit card debt.
Lisa Cacari Stone (00:10:53): This next slide shows that Latino workers are essential works, are vulnerably exposed in their front line jobs at grocery stores, cleaning and sanitation services, food delivery. So, these exposures matter. In a 21-state study, with almost 10,000 workers in animal slaughtering processing plants, Latinos represented 50 percent of the new COVID cases.
Lisa Cacari Stone (00:11:27): We also want to consider the vulnerability of crowded and substandard housing conditions. A quarter of Latinos live in multi-generational households. This could also be a resiliency factor, but as we look at economic impact, more family members and adult children are moving back into the household, making it more difficult to isolate after they're exposed in their working conditions.
Lisa Cacari Stone (00:11:52): I want to mention the Border Colonias in the Southwest. These are unincorporated areas that have crowded and poor housing conditions, and inadequate water and sometimes sewage. We also have the influx and increase of both deaths and cases of COVID at ICE detention centers. These make it dangerous for families who have no choice to be exposed.
Lisa Cacari Stone (00:12:19): Finally, I want to mention our current political and policy environment. Latinos, in a research poll by Pew Center, have indicated and reported that they see their conditions in the U.S. have gotten worse. We can see that structural violence that occurred in El Paso last year, as well as an increased incarceration of migrants and families, impacting the stressors and lives of Latino populations. Moving forward, I want to just mention ongoing... this ongoing discrimination, financial stressors, anxiety, has had an influx in exasperating preexisting mental health conditions. I want to mention the importance of street race, those who would say they're discriminated against because the color of the skin has also impacted many reporting that their mental health conditions are worse, those who are Latinx and Arab. And for Mexican women, it's associated with lower physical health.
Lisa Cacari Stone (00:13:35): Policy matters. As we saw with the Affordable Care Act, we saw a decline in uninsurance rates, particularly the biggest inroads with American Indian, Alaska Native, and Latino communities. We went from 32 percent in 20... we went from almost 33 percent in 2010, down to 19 percent in 2018. However, I want to mention a recent study conducted by Georgetown University. The number of uninsured children now exceeds four million, wiping out a sizable share of the gains in the coverage we made with the ACA. And you can see a decline, especially an increase in uninsurance rates especially after 2016.
Lisa Cacari Stone (00:14:19): Moving forward, policies do matter. State mitigation policies, as well as local policies that require social distancing, closed businesses keep people being safe from spreading exposures. Here it just shows the timeline of the four border states, and we've conducted an analysis. And you can see that the policies implemented by Arizona were not as consistent and regular, as well as in Texas, and have impacted a consistent high, and here in Texas a flux. New Mexico has the most consistent social distancing and mitigation policies, and has been able to keep their Latino COVID rates and cases low.
Lisa Cacari Stone (00:15:05): Finally, I want to move towards why policy matters in terms of immigration. We have a current public charge issue, where Department of Homeland Security and Department of Health and Human Services have moved to include [inaudible 00:15:20] and other social benefits as part of the public charge issue, creating a chilling effect on access to care. The Deferred Action for Childhood Arrivals was upheld recently by the Supreme Court, but how those are being determined is not following the law. We have a new Section, 1557 of the ACA, that undermines the Title XI of the Civil Rights Act around language access. All this has increased barriers to access to care, and increased fear of Latinos, especially Latino immigrants, seeking healthcare services.
Lisa Cacari Stone (00:16:01): How do we move about this solutions moving forward? I want to highlight... well, so there's time for other speakers and my colleagues, but we need to think about universal coverage for all children at the State and the Federal level. Children is the place where we can prevent, and keep children safe and health over the lifespan. Medicaid buy-ins should be an option for all, and unauthorized immigrants, with State policy and actions, could be allowed to buy into Medicaid. We need to continue to protect the gains we've made with the Affordable Care Act, rescind the public charge rule, and make sure there's protections for DACA.
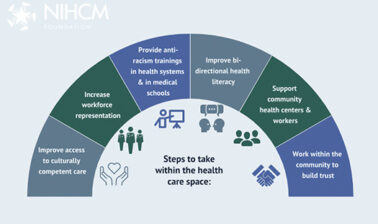
Lisa Cacari Stone (00:16:44): If we think about the role here on the right box of the healthcare system and hospitals, Federally qualified health centers, and the safety net, they have the option to tackle implicit bias and antidiscrimination. Mobile access points could be implemented for mental health resources, especially in geographically remote areas and areas where's there more ICE presence. I want to mention the importance, evidence shows us that community health workers or [foreign language 00:17:12] play a huge role in improving access to care, especially for the most vulnerable.
Lisa Cacari Stone (00:17:20): As we look in the third box, COVID-19 policies and mitigation are critical here. Assured we have to be able to track equitable Federal assistance disbursements, and also we could gain coverage by covering social determinates of health.
Lisa Cacari Stone (00:17:38): I'm going to end with just communities need to be centric to solutions, inter sectorial partnerships with Latino based organizations are critical. And on the right, we need to continue to have non-discrimination laws at the State, Federal, and local level, and invest in housing developments. Thank you for your time, and I look forward to the discussion. It is important that we continue the fight towards racial and economic justice and our vote counts.
Sheree Crute (00:18:09): Thank you so much, Dr. Cacari Stone for giving us an extraordinarily comprehensive national picture of the issues impacting Latino health and the policies and solutions to bringing about progress.
Sheree Crute (00:18:23): Our next speaker, Dr. Jane Delgado, is the President and Chief Executive Officer of the National Alliance for Hispanic Health. Dr. Delgado is a highly respected and well-known activist, writer, thought leader, and commentator who has dedicated her career to transforming health. Just this week, the Association of American Medical Colleges honored Dr. Delgado as one of ten Hispanic pioneers in medicine. A clinical psychologist, Dr. Delgado is author of more than ten books, including 2020's Understanding Depression and Enjoying Life. She is going to address how a lack of inclusion, systemic racism, poor access to healthcare and mental health coverage affects Latino health and methods for moving forward.
Sheree Crute (00:19:08): Dr. Delgado. Is Dr. Delgado able to join us?
Jane L. Delgado (00:19:26): Hello? Hello.
Sheree Crute (00:19:28): Yes, Dr. Delgado?
Jane L. Delgado (00:19:29): Okay, I'm sorry. I thought... I was talking to myself.
Sheree Crute (00:19:33): That's okay. We can hear you now. Thank you and welcome again.
Jane L. Delgado (00:19:35): Okay. So, thank you Lisa and thank you Sheree. This is a very important time for all of us, and I want to thank everyone who is hear listening to this presentation because this is a time when we can move from what the past was, which was ignore or false assumption, to inclusion. And this is important for all of us. And I think that part of what you need to see is who we are, the National Alliance for Hispanic Health, and you need to understand we're a nonpartisan health organization for research, service, and advocacy throughout the Americas. So, we actually fund programs in Latin America. We also do not accept funding from tobacco or alcohol or sugar sweetened beverages. And this makes us really advocate best health for all.
Jane L. Delgado (00:20:34): Now, you see the name Hispanic in our name. Well, about six years ago, we changed our mission from improving the health and wellbeing of Hispanics to best health for all because we realized in order to help everyone, we had... that by helping everyone, we also helped Hispanics. And what you need to know is that a person's values when they speak to you are very important, and these are our organizational values throughout the alliance that I lead. I also want to note that we have a research arm at USC, and we also focus the Alliance and programs on diabetes, cancer, and are part of NIH's All of Us activity.
Jane L. Delgado (00:21:23): With that, you need to know that what we value are three things, people, science, and culture. Those are the three things that are the underpinning of everything that we do at the Alliance. When we talk about how come we're having such a problems with Hispanics and healthcare, frankly this is not a new surprise for most people. The reality is that we are the group that is most likely to be uninsured. And the reason that we are uninsured... and we are the purple there. You can see for all groups not insured by age, race, and ethnicity. Although the ACA did a lot for us, a major determinate of whether or not we're insured is what state we live in.
Jane L. Delgado (00:22:18): States like Texas and Florida, where there are a lot of Hispanics, where their total number of Hispanics in Texas and Florida combined equal all the Hispanics in California, Texas and Florida did not do Medicaid expansion. And as a result, that really drives down the number of Hispanics who actually have insurance. And some people say, well, I'm not too sure about these data and what they mean. And I said, well, even if you look at it by gender, what you still see is that Hispanics, which are the purple lines, are still underinsured. We have no insurance and it's a problem throughout the ages, for men on top and for women on the bottom.
Jane L. Delgado (00:23:07): And then, of course, people like to talk about, well, Hispanics are so diverse. Maybe it has to do with the country of origin. When we look at those data from the Census Bureau, we found a very important pattern. That the group most likely not to have health insurance are people ages 18 to 64, across whether you are Mexican, Puerto Rican, Cuban, Central American, South American, or other Hispanic. This is the group that is least likely to have health insurance, and yet this is a group where we can have a major impact on health issues.
Jane L. Delgado (00:23:49): Now, one of the things which is most amazing to me is that when people talk about health, they try to think of it from their perspective. But I like this picture with all the windows because, in fact, the window you look out of colors what you see. And one of the things that most people don't realize is the size of the Hispanic population. So, there are 59 million, it's .6... you can say 60 million, but I don't want to exaggerate, so I'll just stick to 59.6, so there we go. And what does that tell you? People say, well, Hispanics are so diverse and they're of multiple races, but you can... all of these groups are diverse. There's no group which is all the same. If you talk to non-Hispanic Whites, they're a very diverse group also. Yet, for the purposes of our current systems, we do aggregate them.
Jane L. Delgado (00:25:01): So, I need to emphasize that our current systems are part of what we're using, but that that system is changing because as we get better data, we can get more specificity about the individual that is sitting in front of you. And that is key because personalized medicine will make many of the current debates about if you're Hispanic, or Latinx, or if you focus on the country of origin, really looking at who that person is. And also, the labels that we use are constantly changing because how people see themselves is constantly changing.
Jane L. Delgado (00:25:48): And a good example of this is that for a long time people used the term people of color. And this was a OpEd piece that recently appeared in the Washington Post, by a former Congresswoman. And what it basically says is, I don't want to be called a woman of color, I am a Black woman, we are Black women. And the reason is because each community has their own heritage, has their own experiences. And those experiences have an impact on their health. And we know that because that's what epigenetics is about, how the things which are around us change the way genes express themselves.
Jane L. Delgado (00:26:39): When it comes to the Hispanic community, in fact, one of the problems that I see is that most people have very little knowledge of our history. The culture sort of forgets that arrival and acquisition is part of the Hispanic experience. And most people in the Northeast, I'm sorry to say, are not aware of the U.S.- Mexico War or the Treaty of Guadalupe Hidalgo in 1848 and what that meant. Most people do not know that Puerto Rico was annexed in 1898 as part of the Spanish-American War. That history, or even that Florida was first founded by the Spanish, a lot of people don't know our history.
Jane L. Delgado (00:27:29): So, our history is very diverse. Which, in a way, is different than the African American community that can trace themselves to a common event that brought them here, which was the horrific slavery. So, I think part of it is understanding the how people became part of the U.S., what that history means, and how that impacts their lives today.
Jane L. Delgado (00:27:58): The next thing that I always say is when you're talking about what's going on in institutions, you really have to talk about how accurate is it what we know? And frankly, it's not very accurate. For a long time, what we used to do is use something in health called Reference Man. And this was... Reference Man was used for looking at estimation of radiation does, and was first used in '75. In 2010, they were still looking for a modern Reference Man, but that was used for all sorts of things besides radiation. Cancer, the effects of toxins, and all sorts of things like that. So, really those data weren't very good.
Jane L. Delgado (00:28:45): But needless to say, even with bad data, we always made assumptions. So, when these data came out that Hispanics live longer than... whoops... than non-Hispanic Whites, it was people doing cartwheels trying to say that this could not be possible because of all the vulnerabilities that people know are part of the Hispanic experience. But, somehow, we live longer. And it was contrary to a minority model or myth about minorities that we actually live longer.
Jane L. Delgado (00:29:22): Hispanics became even more controversial in how the health system would treat us when our rates of heart disease mortality also showed that we did better than non-Hispanic White. And one of the problems I always see is when people look at what the goal should be for health, they say, well, let's do what... let's go to the non-Hispanic White standard. And my response is, no, in rates of heart disease mortality, let's go to the Hispanic standard. Everyone should be better than the best, and in this case we're the best. It's a similar situation when it comes to what we know about population pregnancy-related mortality ratios. Across all ages except 35 to 39, Hispanics actually did better than non-Hispanic Whites.
Jane L. Delgado (00:30:15): So, what does this mean? Well, it means that as Hispanics we live long and suffer. And the problem with that is that our conditions, depression, diabetes, arthritis, and liver disease, are things that are not looked at as carefully as they should. As a result of that, what you have is artificial intelligence and decision making tools which create a system that does not include information about Hispanics. And that damages the outcomes for people who go in there, but also is really not a tool for the clinician. I want to add that it's not just having good data, it's also the analysis. You have to also go beyond the numbers.
Jane L. Delgado (00:31:05): So, when NIH first announced that from 2009 to 2016 they now had many more data on Hispanics... I mean on non-Hispanics, it went from 4 percent to 19 percent, people were thrilled. But when they really looked behind the data, and they said what is going on here, the data increase was for Asians. For African-Americans, it only went from .57 to 3, and for Hispanics it went from .06 to .54. So, you really had to look at more than just the big data, but drill down.
Jane L. Delgado (00:31:46): Finally, what happens when people do not look at all the data? A good example is the American Cancer Society Guidelines for the Prevention and Early Detection of Cervical Cancer. These just came out July 30th, and they have their guidelines. Then, at the very end, they talk about the limitations for these guidelines. And who are these guidelines limited for? Black, Hispanic, and lower SCS status women. Why? Because those populations are not optimally represented in randomized controlled trial. Let me say, not optimally is an understatement. Those communities are not represented adequately.
Jane L. Delgado (00:32:37): So, where does that leave us? Well, this leaves us at we have a challenge. If we're going to move from the idea of going from ignore to inclusion, we really have to look at many things. And these things are some things that are critical to change. And it's not just about having a program, it's about having leadership, board, staff, and constituents, that are inclusive about having accurate data, about having meaningful analysis, and a capacity that goes beyond the numbers, like what I showed with the cancer guidelines. And to understand that personalized and targeted is the way to go.
Jane L. Delgado (00:33:27): And I'm sure some of you are thinking, well, she's a psychologist. Isn't she going to talk about mental health? Well, the bottom line is, health is mental wellness, and you can't have health without including mental health. But mental health is something that you can talk to people when there's a trusting situation, when the trust which is earned over time and experiences. When people come to me and says, what can I do gain trust? And I said, well, you have to spend time on it. And they go, oh. Well, that's not what they want to do. You have to... trust is gained over time. Not one moment, but over experiences.
Jane L. Delgado (00:34:07): The role of community health workers is key in mental wellness. They are a big way to get people into mental health services. Cultural and language need to be celebrated, not just acknowledged. And we have to go beyond translation. In mental health, language is more than just what you can ask. You have to be able to listen to the people.
Jane L. Delgado (00:34:36): And with that, I want to say my thank you to everyone who is out there for all you do to achieve the best health for all. That's a real picture of our headquarters, and yes, that's a real rainbow. It's not fake. So, that's about all I can say, and I wish everyone all the luck in all the work that you do.
Sheree Crute (00:35:03): Thank you so much, Dr. Delgado, for that powerful and insightful presentation, and shining a spotlight on some of the inadequacies in research and how groups are counted and assessed and considered.
Sheree Crute (00:35:19): Now I would like to welcome Juan Chaluja. Mr. Chaluja is Vice President of Commercial Markets, Analytics, and Chief Financial Officer at Florida Blue. Mr. Chaluja has more than 25 years of domestic and international experience in the health insurance industry. Under the leadership of Pat Geraghty, Florida Blue's President and CEO, Florida Blue has become a leader in providing culturally relevant high-quality care to the Latino population in Florida, specifically through the Sanitas Medical Centers, as well as programs that support economic, social, and health causes in Latino communities. Today Mr. Chaluja is going to talk more about Florida Blue's innovative strategies.
Sheree Crute (00:36:05): Mr. Chaluja.
Juan Chaluja (00:36:09): Thank you very much. I first want to thank the National Institute for Health Care Management for allowing me to participate in today's webinar focused on the Latinx population, which is really important to me, of course. I also want to thank Lisa and Jane for their contributions that were very insightful. So, I appreciate that. I learned a lot during the last half an hour.
Juan Chaluja (00:36:35): To that, I wanted to start my presentation by providing solutions... what we're doing at Florida Blue, solutions to address the needs of the Hispanic community within Florida. First and foremost, at Florida our plans cover population in Florida only, so I'll be discussing our solutions for the Florida populations only and not outside of Florida at this time.
Juan Chaluja (00:37:06): And as you can see, Florida's Hispanic population is very diverse and it's growing three times as fast as the rest of the population in the state. Out of the 22 million people that live in Florida, about six million are Latinos, 25 percent, and they are mainly located in central and south Florida. And the origins of the Latino population mostly, again, of Cuban descent, South and Central American descent. About 15 percent of those are Mexicans, about 21 percent of those are Puerto Ricans. So, we [inaudible 00:37:53] we say that we're pretty diverse. We do see the different nationalities have a little bit of a different feel within the Latino population, but overall we're pretty diverse. And as you can see in Florida, it's mainly... 27 percent Latino. So, pretty populated [inaudible 00:38:16].
Juan Chaluja (00:38:16): We, at Florida Blue, are in the local community. We have 30 Florida Blue Retail Centers across the state, some of which are embedded in a YMCA or Walmart or paired with a clinic. We have Spanish speaking associates in person and on the phone, and all of our materials are in Spanish. Also, we have Hispanic member care specialists and sales agents who can help people who are uninsured get insurance. Our previous speaker spoke about the issues we're having with uninsured after the Affordable Care Act passed in 2014 and the Hispanic populations specifically affected by that. So, in these retail centers is one of our areas where we can help the uninsured get affordable insurance.
Juan Chaluja (00:39:24): We can also help people who have trouble affording the health insurance, we also are focusing on specific [inaudible 00:39:37] with the highest uninsured rates. Our community specialists in our retail centers provide services to both members and non-members. So, we're there for that population, we're there for the community. We're trying to help people gain access to services and community resources. Sometimes people need assistance with medication, rent, food services, transportation services, et cetera, and we connect them with those resources.
Juan Chaluja (00:40:14): I'm switching slides here. We also do a lot of work in the Hispanic community through our Foundation. Health equity is one of our Foundation's primary area of focus. We believe no one's health should ever [inaudible 00:40:36] of social determinate or economic circumstances. We are committed to helping insure that all of Florida's families and community members have both the access and opportunity to attain full health potential and are not disadvantaged due to environmental, economic, and social conditions.
Juan Chaluja (00:40:57): So, these I'm showing you in this slide, there are three examples of organizations and programs we have supported. The Hispanic Services Council, where we've provided $542,000 in grants in the Hillsborough County. We have the Farmworker Program, where over the last five years we've provided over $300,000 in grants. And the Hispanic Unity, since 2018, we've provided $300,000 in grants for that.
Juan Chaluja (00:41:30): The Foundation also strives to impact food security and mental wellbeing. We want to make sure that all people, at all times, have physical and economic access to adequate amounts of nutritious, safe, and culturally appropriate food, which are produced in an environmentally sustainable and socially just manner. And that people are able to make informed decisions about what they're eating.
Juan Chaluja (00:42:02): That takes us then to our solutions, our primary care solutions. Sanitas Medical Centers are the results of a partnership between Florida Blue and Keralty, which is an international organization headquartered in Columbia, to bring an advanced primary care model to Florida. Medical centers are focused on the specific needs of, of course, the Hispanic population. The primary care model, with native Spanish speaking physicians and staff, allows Florida Blue's Hispanic population to have convenient access to healthcare, while experiencing the wholistic engagement in the same style when I receive care in my country of origin. It makes us Latinos feel we're [inaudible 00:43:01] connected with our doctors. This connected experience allows the Latinx population to feel more comfortable when needing to get care, and provides a culturally relevant experience.
Juan Chaluja (00:43:16): The centers go deep into primary care. We've integrated... we've created specific products within Florida Blue that are integrated with the Sanitas Medical Centers, that provide services to support their patients, which include for example zero dollar copay for primary care and origin care benefits. [inaudible 00:43:41] advantage over other plans, specifically in individual business for Affordable Care Act. The common goal here is to improve health outcomes, patient satisfaction, and lower healthcare costs.
Juan Chaluja (00:44:03): Under one roof we have comprehensive primary care, advanced urgent care, on-site labs and diagnostics, high volume specialists. We offer virtual care, including telehealth visits and chat capabilities, wellness and disease management programs all under one roof, and all in Spanish. Services customized for the cultural and linguistic needs of the diverse Hispanic population, allowing for increased communication effectiveness, which can improve health outcomes and reduce health disparities. Convenient and culturally relevant, the model incorporates community support, including social networks, social services, and integration with social determinate of health initiatives, as well as offers home based care and unlimited telehealth access, which have... and I'll talk about that later... come in handy with the pandemic.
Juan Chaluja (00:45:24): The creation of the Sanitas Medical Centers took place to serve our Hispanic population, while understanding the dynamics of the Affordable Care Act. We started with three centers in Miami-Dade in 2014, and currently there are 35 Sanitas Medical Centers and primary care offices in South Florida, and the Tampa and Orlando Metro areas, serving over 200,000 Florida Blue members. This is an example of a Miami map and where all the clinics are located. Each clinic is strategically located not only in Hispanic areas... most of Miami is Hispanic anyway... but within three to five miles radius driving distance to each of the clinics.
Juan Chaluja (00:46:19): So, the Sanitas Medical Center performance has experienced great success and that's what sets us apart form other providers and other healthcare systems. Patient satisfaction and [inaudible 00:46:35], for example, are above average, and demonstrates the strength of our leadership with our Hispanic population, while providing favorable health outcomes with 50 percent lower utilization... hospitalizations and five percent reductions in emergency visits.
Juan Chaluja (00:46:54): I'm particularly invested in this partnership with Sanitas. I am part of the Sanitas Board of Directors, I am involved on a day to day basis of that operation, and it is something that has created great success among Hispanics. And being in Florida, I think it's very important to be able to offer some kind of solutions for our Latino population. Earlier we spoke about health disparities, whatnot. This is a really good solution that has exceeded our expectations.
Juan Chaluja (00:47:51): So, the impact of COVID and our response. During our prior panelists, they discussed proportionate impact of the COVID-19 on Latinx communities highlight the health disparities that have well-long existed and the importance of addressing the social, economic, and environmental barriers to be able to achieve health equity. So, in June GuideWell, the parent company of Florida Blue, launched a $100,000 challenge to address health and racial inequities. Reshaping health access in a statewide challenge to identify solutions focused on addressing health access and literacy to populations in Florida experiencing high levels of health inequities.
Juan Chaluja (00:48:50): To that end, during the pandemic back in March, Sanitas quickly responded to the pandemic by offering free bilingual virtual care visits via MySanitas mobile app or at their website, through their website. They also responded by designating specific location to see patients who have respiratory symptoms, while having other locations for non-COVID related care. Thus allowing us for an improved opportunity to serve Hispanic and COVID-related symptoms. So, I showed you a map two slides ago. And, for example, in South Florida we have 13 clinics. We designated some clinics that were specific just for COVID patients, and other clinics that were non-COVID patients. That way, we increased the availability of patients with those symptoms to go to the clinic and get care.
Juan Chaluja (00:50:01): We optimized our PPE supplies levels to protect the staff and patients, as well as followed protocols for screening patients, cleaning the facilities, practicing social distancing, handling sick staff. This way, Sanitas was able to provide uninterrupted services during the pandemic and at the beginning when we were in lockdown. Constant communications, outreaching our members and patients, goes out to member via emails, text messages, Facebook, and through their website.
Juan Chaluja (00:50:38): And to that, I wanted to thank you for allowing me to speak a little bit about our primary care model specifically serving the Hispanic population. 15 minutes is not too much to go too much into depth with our model, but I'm happy to host additional questions or emails. You have my contact information. Be happy to provide more information if needed. Thank you.
Sheree Crute (00:51:10): Thank you, Mr. Chaluja, for sharing solutions from the Sanitas Initiative and effective approaches for culturally sensitive care.
Sheree Crute (00:51:18): We have just a tiny bit of time left for questions. We had many come in that combined several topics. One of the topics that came up several times... Juan, you can take this first if you like because I know you have a flu vaccine program going on where you are, and perhaps Jane or Lisa you may want to join in. We have consistent questions about how can... what strategies are being employed to increase flu vaccination rates and then, correspondingly, hopefully deal with the COVID-19 vaccine, in Hispanic communities?
Juan Chaluja (00:51:55): Sure, I can take that... begin taking that question. Thank you, appreciate the question. It begins with education. We continue to offer informational webinars to explain the importance of getting the flue shot. Through our partnership with Walgreens, Florida Blue is planning to sponsor drive-thru clinics as well. Flu shots are available at no cost to Florida Blue members and non-Florida Blue members, regardless if you have insurance. Florida Blue members [inaudible 00:52:28] we have a rewards program where they can earn money for their deductibles and the copays, whatnot. By getting the flu shot, they can earn money through that program as well.
Juan Chaluja (00:52:39): At the Sanitas Centers, there is a marketing strategy going on right now where we're emailing and texting reminders in each of our 200,000 members to remind them to take flu shots. All Sanitas employees and staff, physicians and staff, have already been vaccinated and are [inaudible 00:53:03] the importance of the vaccine. And they're probably [inaudible 00:53:07] on their uniforms to show it. There's also promotions during visit planning, strong social media education efforts at Sanitas, as well as Florida Blue. And for Walgreens there are upcoming events that are flu shot events for the Sanitas patients, and they will include [inaudible 00:53:25] as well.
Sheree Crute (00:53:25): I see. And, Lisa, do you see that as applicable with COVID-19, or Jane?
Jane L. Delgado (00:53:38): This is Jane. I just wanted to say one of the things we're working with is with the science community to make sure that there is good representation of Hispanics, both in the development of a vaccine in the clinical trials, and also there are a lot of treatments that will be coming online, and to make sure that Hispanics are included in those, so that we can make sure that if a vaccine is developed, that it is one that we know has been successful in our community.
Sheree Crute (00:54:07): I see, thank you. One of our last questions is about communication practices. Just knowing that... I'm sorry... communication practices and ways that community health workers and others can help Hispanic families, Latino families, deal with upcoming festivities and opportunities to be close in a safe way with COVID-19 transmission, but in a respectful manner?
Jane L. Delgado (00:54:42): [crosstalk 00:54:42] I think each of the community workers knows the community that they're working in, and what are the options they have for social distancing and still celebrating different kinds of events. The one good thing is that Hispanics are more likely to use a mobile than anybody else. So, how we can do things on our mobile would probably be very helpful for many families to try to incorporate new ways to try to celebrate because we really need to protect each other and maintain that social distancing, and make sure that we wear a mask and also, if you can, to wear glasses. So, the two things are very important. Remember, the virus enters through mucous membranes, that's why your nose, mouth, and also your eyes are important to keep covered.
Lisa Cacari Stone (00:55:38): This is Lisa. I just want to mention that community health centers are the largest safety net network in our nation, serving over 28 million. And community health workers, or [foreign language 00:55:48], working with these health centers in rural areas, migrant health centers in communities, public mental health centers, are all critical to serving our Latino community. Currently just about 33 percent of Latinos get their testing through these health centers.
Lisa Cacari Stone (00:56:05): So, I think as trusted partners and current trusted organizations, it's important that [foreign language 00:56:11] be there, in the community. Also, we have to outreach and get the message out in Spanish language radio and television, and outlets in the ways that our communities get them. And the message is not getting... back in the '80s, our first surgeon Latina general, Antonia Novello, said the problem with the Latino community and our efforts nationally and locally is they're having to do the 9-1-1 because they're not getting the 4-1-1. So, definitely the Spanish language outlets are critical.
Jane L. Delgado (00:56:44): Well, let me just add something to that. I also believe that when people want to reach our community, they know how to reach it. So, I was very distressed this year when I had to put out press releases and do lots of interviews telling people not to drink bleach because that was not going to cure them. So, I think that there are ways to reach our communities. And just like the people who try to sell us and give us bad information reach us, we have to use those very same methods to try to give people the best information possible. Because the internet, our mobile phones have changed everything from the '80s, and we have to amp up our game and do things in a way that really reaches all ages, in every way, repeatedly.
Sheree Crute (00:57:35): Thank you very much, Jane. We have two minutes. I don't know if anyone can address this. We've received several questions about the best way to gather correct data on Hispanics, given that we're using Latino, Latinx, Hispanic, and different terminologies, street race, this term. We have just a minute. Maybe, Lisa, since you used street race?
Lisa Cacari Stone (00:58:01): Yeah. I responded to several questions and written answers. Thank you for those questions. First of all, the question was around what's the term? Well, I think for the Census purpose we have for enumeration Hispanic. But it certainly is acceptable to be inclusive and understand that different Latino communities, whether it be by different distant histories, as Dr. Delgado had mentioned, or by national affiliation, or length of stay here, as well as generational status, might go by Latino, Latinx, Chicano, Hicano, Mexican American, Cubano. I think that we need to honor that people need to be able to name who they are.
Lisa Cacari Stone (00:58:43): That being said, the COVID data is available, I responded, to the CDC COVID Data Tracking System by state and county. Now, it does a general Hispanic variable, but there is not sub-population analysis. And that's something I left out in the past board and the call to action is we need to push our local, state, and Congressional, and at the executive level in D.C., to collect the data by race, ethnicity, and subpopulations. This is critical to be able to understand the impact on our communities. Thank you.
Sheree Crute (00:59:23): Thank you.
Jane L. Delgado (00:59:25): And just to add one closing thing, it's less important what you call people and what you do... than what you do. And always remember, among African-Americans, among Asians, or every sub-group, nonHispanic Whites, what they're called varies by what state they live in and their community. So, call people what they want, but do what they need.
Sheree Crute (00:59:47): Thank you so much, Dr. Delgado, Dr. Cacari Stone, Mr. Chaluja. Unfortunately, we're out of time right now. You've been an amazing panel. Thank you so much for taking time out of your schedules to be with us today, and to our audience. Please take a moment to share any feedback about this event by completing a brief survey that you can find at the bottom of your screen. Also, please check other resources on our website. And in a few weeks, you will receive an invitation to a third webinar in this series, Systemic Racism and Public Health Treatment Bias in COVID-19.
Sheree Crute (01:00:27): Again, please do click on to our survey and don't forget to share your opinions. Thank you so much for your time and have a wonderful afternoon everyone.
Presentations
The Impact of Racism, Inequality and COVID-19 on the Health of Latinos

Lisa Cacari Stone, Ph.D., M.A., M.S.
University of New Mexico
Moving from Ignore to Inclusion

Jane L. Delgado, Ph.D., M.S.
National Alliance for Hispanic Health
More Related Content
See More on: Health Equity | Coronavirus