Expert Voices
The Health Care Safety Net: Community Health Centers' Vital Role
By: Peter Shin, PhD, MPH, Associate Professor of Health Policy and Management, George Washington University
Despite substantial gains in insurance coverage linked to the Affordable Care Act (ACA), 9.1 percent of U.S. residents—or nearly 29 million people—remain uninsured.1 At the same time, rising out-of-pocket health expenses are limiting access and imposing financial hardship on increasing numbers of people who are insured, especially those at lower income levels. Many of these people are heavily reliant on the health care safety net and, in particular, on the care provided by the nationwide network of non-profit community health centers (CHCs).
In this essay, I describe the current status of CHCs and the post-ACA environment in which they are operating. The evidence indicates that even as we continue to expand coverage and improve care delivery under the ACA, strengthening the health care safety net by supporting CHCs must remain a priority.
What Are CHCs?
First launched in the mid-1960s, CHCs’ mission is to provide affordable care for medically underserved and low-income populations in both urban and rural communities. With a history of bipartisan support, the program has grown to over 1,300 health centers serving 24 million patients at over 9,000 service delivery sites.2
CHCs must accept all patients, regardless of insurance status or ability to pay, and they use multidisciplinary care teams to provide a comprehensive set of services, including dental, vision, behavioral health and pharmacy services as well as enabling services such as transportation and translation that are not typically covered by insurance. They are also uniquely staffed to help people with low health literacy, and most have online technology necessary for Medicaid and health insurance exchange enrollment. In 2014, 92 percent of CHC patients had incomes below 200 percent of the federal poverty level and 71 percent were living below the poverty line; 28 percent were uninsured.3
CHCs rely on a diverse mix of funding streams to cover their costs, including enhanced reimbursement from Medicaid, Medicare and private insurers; patient payments based on income-related fees; competitively-awarded federal grants; and other grants and contracts from state, local and private sources. In FY2015, 43 percent of all CHC revenue was from Medicaid and CHIP. Federal grants accounted for 22 percent of revenue and Medicare and private insurance payments added another 16 percent, while direct payments from patients constituted only 5 percent of CHCs’ revenue.4
Studies consistently show that CHCs improve the health status of communities and patients. Importantly, they have also been linked to costs savings through (a) reduced use of emergency rooms; (b) fewer preventable hospitalizations; (c) improved access to primary and prenatal care; (d) enhanced preventive and chronic care management; (e) fewer unnecessary tests; and (f) the more prevalent use of less expensive providers.5
CHCs and the Affordable Care Act
The ACA supported CHCs in several ways, most notably by providing $11 billion in new mandatory funding over five years to increase the number and capacity of CHCs. In 2015, Congress extended this funding through 2017. The ACA also enhanced Medicare reimbursement for CHCs by requiring a new payment system better reflecting their costs of care.6
The ACA’s coverage expansions through Medicaid and private insurance should help CHCs’ by increasing revenue from insured patients. Past experience leads us to expect these new resources will lead to expansions in CHC capacity and services.7
At the same time, the higher patient demand arising from expanded insurance coverage means CHCs—many of which are already straining under workforce shortages—will need to recruit additional staff. To help on that front, the ACA appropriated $1.5 billion over five years for the National Health Service Corps plus $230 million over the same period to support graduate medical education in CHCs and other community-based settings (both streams subsequently extended through 2017). These avenues are proven ways to address CHC staffing challenges.8
Lastly, the law designates CHCs as a type of essential community provider and requires private plans sold in the exchanges to offer a contract to at least one CHC in every county in their service area where a CHC is present. Plans must pay at least the enhanced Medicaid rates to these facilities, and negotiated rates could be higher.
How Are CHCs Faring?
To better understand the experience of CHCs in this post-ACA environment, my colleagues and I conducted a nationwide survey of CHCs and analyzed program data submitted by all CHCs.9 Our results underscore the critical role CHCs are playing in helping the uninsured apply for and get coverage: more than 80 percent of CHCs said they provided Medicaid application assistance during the first open enrollment period, and 90 percent reported providing application assistance for health plans in the exchanges. Recent data from HRSA confirm that CHCs have continued their outreach and enrollment efforts, providing assistance to over 17 million people since ACA enrollments began.10
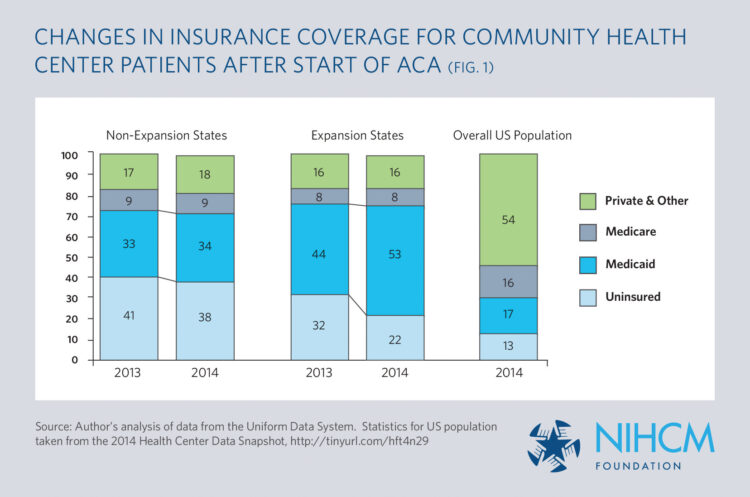
We also found substantial benefits to CHCs from the ACA Medicaid expansion. In the first year of the coverage expansions, for example, the share of CHC patients with Medicaid coverage increased from 44 to 53 percent for CHCs in Medicaid expansion states while remaining almost unchanged for CHCs in non-expansion states (Figure 1). Importantly, these latter clinics were already at a disadvantage due to their states having less generous Medicaid coverage for childless adults, and the gap has grown significantly wider as the expansion states have further improved their coverage of this population. Additionally, reflecting the benefits of new revenue from insured patients, we found that CHCs in Medicaid expansion states were significantly more likely than clinics in non-expansion states to report improved capacity to provide dental and mental health care.
CHCs in expansion states also experienced a commensurate drop in the share of patients without insurance. Despite the gains in coverage, however, the CHC patient population still looks very different from the nation overall. Namely, CHCs continue to serve a significantly disproportionate share of uninsured and Medicaid patients and a much smaller share of patients with private coverage.
Looking Forward
Propelled forward by the Affordable Care Act, CHCs are making a major difference in expanding coverage and access to comprehensive primary care in many of the nation’s poorest communities. However, these providers continue to face major challenges in serving a patient population that is not only much more likely to be uninsured but also at higher risk for more complex health and social problems than seen in other primary practice settings. Sustained and even enhanced support is needed to help them fulfill their mission.
Currently, federal grants cover only about a fifth of CHCs’ operating costs, and several of the major federal funding streams are promised only through 2017. These funds are a critical supplement to the reimbursements received from third-party payers and the modest fees paid by patients, allowing CHCs to serve uninsured patients, provide the enhanced services important to low-income patients, and perform needed outreach and enrollment. The funding also helps CHCs to reduce the cost-sharing burden faced by privately insured patients who cannot afford their out-of-pocket costs for covered services—a contribution that will be even more important if the Administration loses its appeal of the House of Representatives v. Burwell decision determining that funds for the ACA cost-sharing subsidies were not properly appropriated. As a new Administration and Congress make budgeting and appropriation decisions in the coming year, it will be important to consider the evidence showing the many ways CHCs are serving the most needy patients among us.
Future state decisions about Medicaid expansion will also weigh heavily on CHCs. The much larger coverage gains we documented for CHCs in Medicaid expansion states, combined with the improvements in their capacity to provide mental health and dental care, highlight the importance of motivating the 19 non-expansion states to reconsider that choice. Millions of low-income, non-elderly people have fallen into a “coverage gap” in these states. CHCs and other safety net health care providers are crucial for these patients but will continue to struggle to meet their needs without Medicaid expansion. One can only hope that future decisions about state Medicaid programs will be motivated less by politics and more by objective assessments of the benefits to population and community health, which our findings show are substantial through CHCs.
- Cohen RA, Martinez ME, and Zammitti EP. “Health Insurance Coverage: Early Release of Estimates from the National Health Interview Survey, 2015.” National Center for Health Statistics, May 2016.
- National Association of Community Health Centers. “America’s Health Centers.” Fact Sheet, March 2016.
- Author’s calculations using the data from the Bureau of Primary Health Care’s Uniform Data System.
- Heisler EJ. “Federal Health Centers: An Overview.” Report 7-5700, Congressional Research Service. January 2016.
- Heisler EJ. “Federal Health Centers: An Overview.” Report 7-5700, Congressional Research Service. January 2016.
- Heisler EJ. “Federal Health Centers: An Overview.” Report 7-5700, Congressional Research Service. January 2016.
- Shin P, Rosenbaum S, Bruen B, Lu A, Arguello R, and Tolbert J. “Medicaid and Community Health Centers: The Relationship Between Coverage for Adults and Primary Care Capacity in Medically Underserved Communities.” Kaiser Family Foundation. March 2012.
- National Association of Community Health Centers. “Staffing the Safety Net: Building the Primary Care Workforce at America’s Health Centers.” March 2016.
- Shin P, Sharac J, Zur J, Rosenbaum S, and Paradise J. “Health Center Patient Trends, Enrollment Activities, and Service Capacity: Recent Experience in Medicaid Expansion and Non-Expansion States.” Kaiser Family Foundation. December 2015.
- Health Resources and Services Administration, Bureau of Primary Health Care. Personal communication, May 23, 2016.
More Related Content
See More on: Cost & Quality
