Webinar
Long COVID: New Research and Supporting Patients
Time & Location
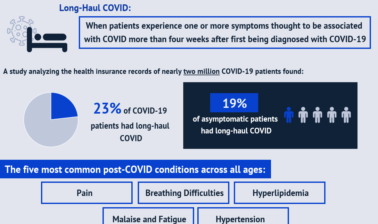
As the COVID-19 pandemic continues, there is an increasing need to understand and respond to long COVID. More than 45 million confirmed coronavirus infections have been reported in the U.S. and more than half of COVID-19 patients experienced long COVID, called Post-Acute Sequelae of SARS-CoV-2 infection (PASC), six months after recovery. Long COVID conditions such as pain, difficulty breathing, hypertension, and fatigue can be debilitating. Living with long COVID has upended daily life for millions of Americans and it can be difficult to get support and care for symptoms. Vaccination against COVID-19 can reduce the likelihood of developing long COVID and can even help people with long COVID feel better.
This webinar brought together experts to discuss the latest research on long COVID and strategies to support individuals with the conditions. Speakers discussed:
- The national effort to understand, treat, and prevent the long-term effects of COVID-19
- New and emerging data on long COVID in different populations broken down by demographic factors
- Strategies to address the impact of long COVID on the health care system through federal policy recommendations and payment models
- A health plan’s efforts to connect individuals suffering from long COVID to care and other resources
0:05
Hello, everyone, and welcome to today's webinar, Implications of Long coven for Patients In The Healthcare System.
0:12
Before we get started, I would like to go over a few items. So you know how to participate in today's event.
0:17
You may have joined the presentation listening Using your computer's Speaker System, by default.
0:22
If you'd prefer to join over the telephone, just select phone in the audio pane and the dial in information will be displayed.
0:28
You'll have the opportunity to submit text questions to the presenters by typing your questions into the questions pane of the control panel.
0:36
May send in your questions at any time during the presentation.
0:39
We will address them at the end.
0:41
I would now like to introduce Kathryn Santoro.
0:45
Hello, I'm Katherine Santoro, Director of Programming at the National Institute for Health Care Management Foundation. On behalf of ..., thank you for joining us today for this important discussion on Long co bed.
0:58
As the covert 19 pandemic continues, there's an increasing need to understand and respond to Long coven.
1:05
More than 47 million confirms Corona Virus Infections have been reported in the US, and up to 50% of cover 19 patients experienced along coed symptoms six months after recovery.
1:19
Non covert is a major public health problem as patients live with debilitating and long term health problems.
1:27
Today, we will hear from a prestigious panel of Experts to discuss the latest research on Long coven and strategies to support patients.
1:36
Before we hear from them, I want to thank Nick Adams, President and CEO, Nancy Shockley, and the ... team who helped to convene today's event.
1:44
You can find full biographies of our speakers, along with today's agenda and copies of slides on our website.
1:52
We also invite you to join the conversation today on Twitter using the hashtag ....
1:59
I am now pleased to introduce our first speaker, doctor Walter ..., the Director of the National Institute of Neurological Disorders and Stroke at the National Institutes of Health.
2:11
We're so honored to have him with us today to share an update on NIH's research to understand, prevent and treat lung ..., doctor Courtland.
2:22
Well, thanks so much, Kathryn, and it's a pleasure to talk to the group today. I think this is a very important discussion.
2:31
Because the implications for so many people are so great.
2:35
And just to start off by saying that we're unfortunately dealing from a position of real lack of knowledge.
2:44
And so I'm going to talk primarily about the program that NIH is launching to better understand the difficulties that people are suffering with many weeks and now months after they've had their acute acute infection.
3:05
See, you guys see the slides.
3:09
I, I don't see slides now.
3:17
Do you see the slides?
3:22
Yes, we can truly do.
3:24
And now I said, OK, OK, now at this, C, Are they, yeah, When I hit the arrow, the slides disappear.
3:44
OK, there's a little bit at the top, I can launch that.
3:52
one second.
3:59
Hmm, OK, maybe I'll try something different.
4:06
Um, OK, so, uh.
4:12
Do you see this slide now that has the NIH mission showing? I do not answer questions.
4:21
Let's just hop trudi.
4:22
Why don't we have security advance, and you just say, next, OK, OK, trudi, can you bring the slide back up?
4:30
Here we go, thank you, OK, next one, please.
4:36
Next slide, yeah, OK, so, yeah, just to say that the NIH mission is, this kinda twofold.
4:43
one is to understand the funnel knowledge about, know, how the body works, and, and the second is to use that knowledge to enhance health.
4:53
And so, I think in the covered experience right now, we're really trying hard to understand, really, what is the biological basis for the problems that people are experiencing and hoping to get some answers very quickly that can then be moved to to help patients. Next slide.
5:16
And the problem is that there are so many culprits out there because covert affects so many different organ systems in the body and, and I guess the big surprise in covered.
5:30
Oh, was that the people who have quote unquote, mild disease can have persistent symptoms.
5:40
We knew that people going into intensive care units and developing acute respiratory distress syndrome or viral pneumonia would absolutely have to have a very long recovery period.
5:52
I think, you know, I think even that year, 75% of people with RDS are unable to go back to work because of their health issues that are remaining.
6:04
So that was not a big surprise, but the big surprise was that the code can affect all these different organs, and, and even people who were never hospitalized, never an intensive care unit complaining and experiencing trebles weeks, months out.
6:23
So initially, clinics started around the country to take care of people after coven, and they were started primarily, by people who were in intensive care unit. Working with intensive care units.
6:36
Because of this, as I mentioned, the expectation that people coming out of the intensive care units, we're going to need special care.
6:44
And but then what happened is that many of those clinics became completely overloaded with people coming, but were never even in the hospital.
6:54
So now, and around the country, we are, you know, we're really learning how to take care of people with this problem of the post ....
7:07
Some People call it Long coven Syndrome.
7:11
And but it's kind of starting out new. And then it's something that I think has to grow and mature.
7:18
And because of the numbers of people who are, who are suffering. Next slide.
7:24
Uh, and I want to say right off the bat that at NINDS and NIH, we've been working on another condition called ..., this chronic fatigue syndrome.
7:39
And that has been very difficult to understand, but the, the point to make here is that the overlap with the symptoms reported in people to have had Cov, it is extremely high.
7:52
So a lot of the neurologic symptoms show with memory, word finding concentration, executive function, sleep disorders.
7:59
Hayne, multiple joints, skin, muscle, abnormal sensations, headache, partial, was static tachycardia.
8:08
Are all very, very common.
8:11
In people with ME CFS and and pretty much read this, this list came from reports from people with Post ... syndrome.
8:23
There's also shortness of breath, dry cough, chest pain, exercise, and tolerance, palpitations, myocarditis, pulmonary fibrosis that are potential down stream from viral pneumonia.
8:41
But the characteristic of chronic fatigue syndrome is an exercise intolerance and something else which I hear on the top is called post exertional malaise.
8:53
That's very peculiar to ME CFS.
8:56
And it could be described as, know, people have fluctuations in how well they do. And on a good day. They may, you know, go out to the store, do kind of normal things.
9:08
But But then for the next two days after that, they completely wiped out this. That's this post exertional malaise. And that's a signature of the ME CFS.
9:18
And we're trying to see how frequent that is in chronic fatigue syndrome. I'm sorry, in the post ...
9:24
cases, and then, of course, anyone who's experienced, know, in intensive care unit, or there's been sick, and, you know, may have even passed on the virus to a parent or a loved one.
9:37
Um, and it's been through the viral illness, with all its all, its concerns potential for, you know, even even death, that that's a, that's a real traumatic experience.
9:52
And then, not getting well afterwards, you know, the normal reaction to, that is, also comes into play in terms of the symptoms.
10:04
Certainly, you know, anxiety could affect sleep, sleep, good effect fatigue. So lots of interacting factors that are likely going on in this group of folks next side.
10:19
So we don't really have the data to try, to inform, You know, how would you take care of?
10:30
Ovid person, the law uncovered person at this point in time, because we're still learning, but I would point it out to the, the UK's National Institute for Health Care and Excellence.
10:43
The nice they have put out a couple of guidelines for management, and to just cut to the chase, They're basically symptomatic management.
10:53
It's identifying, you know, just as a good doctor will do, identifying what the patient's problems are.
11:01
Develop that problem list, and then try to attack as best we can.
11:07
So, for instance, experienced physicians can work on helping people with sleep a number of non pharmacologic and pharmacologic managements of sleep disorders because they're so common in the population that people have experience with that.
11:25
And that potentially could be of help graded exercise, certainly coming out of intensive care units. That's the general path forward.
11:35
And so getting the exercise level up with great Excising makes a lot of sense.
11:40
But as I mentioned just earlier, when would have to, you know, be careful about this potential post exertional malaise that, some people with ME CFS can not tolerate that kind of graded exercise.
11:54
And I should've said, I didn't.
11:56
I'm sorry that many people think that the ME CFS, even prior to Covert, was related to some kind of viral infection.
12:05
I'm really I'm unidentified.
12:09
viral illness that led to the symptoms and people, so, again, another similar pattern, what we're seeing in the Law and Code cases now. Next slide.
12:21
And then we'll go to the one after that.
12:25
And I just wanted to then talk about the recovery program that NIH is launching to understand the recovery issues in coven. Next slide.
12:36
Um, so this is a program that is funded generously by the Congress to the tune of about one point one five billion dollars.
12:45
And it's just being launched, I think, the first patients were enrolled two weeks ago, and it came out of a lot of background work.
12:54
Next slide, then included as extensive listening tours, with the people who are affected, as well as with the docs taking care of folks in the clinics that I mentioned.
13:06
And next slide.
13:08
And the goal of the program is to understand what is the spectrum and the underlying biology, um that goes on and people as they recover from sars, coby to infection. So we have the opportunity, because, unfortunately, the people are still being infected.
13:28
We can look and follow people as they recover from this virus, and try and determine what's different about the recovery process and people who make a good recovery, versus those who are, who plateau out and still having symptoms three months later.
13:45
So this is kind of a, an experiment, a natural experiment to try and understand what are the differences in the process of recovery, what's what's a normal recovery versus a slow smoldering recovery, something we could never do in ME CFS patients for instance because we didn't capture them in time.
14:09
Then looking at people who still have symptoms weeks and months later, how are they different from people who had kovar have now made a good recovery?
14:18
So the first group I mentioned is the acutely affected group. The second group is people who are now weeks and months out already and trying to compare them.
14:27
Then thirdly, because cov, it has been such a huge hit on the health of our country, that we really need to set up a system to look long term into the health of millions, of people to try to see, Are their effects to cope with that are going to be seen in your propensity to develop X, Y, or Z disease 10, 15 years later.
14:51
And so, we're doing that in a large, electronic health record based system. Next slide.
14:57
So we have these clinical recovery that a cohort, so they told you about, and we're looking to, you know, get up to about 15,000 people.
15:06
We're also trying to shortcut and trying to develop an autopsy cohort of people who have died after they've after they recovered from color coded weeks, months later that they may have symptoms or may not have symptoms.
15:22
We really need to look under the microscope to try and see if there are things ongoing like persistent viral proteins being made or persistent.
15:33
Stimulation, the immune system thinks that you would be very difficult to detect in a living person, but but this tissue examination could potentially get us to a shortcut in a very quick time, so that is built into the new program.
15:49
And I mentioned the electronic health record and the real-world data set up to look at, you know, tens of millions of people. Next slide.
15:58
And, so, the next slide just shows that we, we are have, we have set up this really, quite impressive infrastructure.
16:09
We're hoping to, to collect the data across these thousands, tens of thousands of people, in a common way, collect samples, collect the data, So, it's available to others to look at.
16:23
And.
16:26
And, and there are now centers that have been set up, for each of these components of the study.
16:34
Next slide.
16:35
And, here are the centers that are collecting or developing the cohorts and the adults. We have pediatric cohorts that are going to be developed.
16:46
We're also developing cohorts of women who were pregnant at the time, of ..., following both the women and their children, the pathology studies I mentioned, and the electronic health Record Studies. Next slide.
17:05
So we're hoping to get no two answers quickly, and then as soon as we have some ideas on what the trouble is, we're hoping to, we will bring in clinical trials to determine and test different treatments. These may come out of the biological studies.
17:23
They may come from, you know, the people who are taking care of patients, If they think that they found something that's helpful in their patient population, we can test it in the larger population.
17:35
And the good news is where we really have an army of people working in this problem. Now.
17:41
And next slide.
17:42
There are a number of trials, if you go to clinical trials dot gov, that are being tested around the world, these are not funded by NIH at this point in time.
17:54
And, but just to give you a sense of what's out there, at the current time, in terms of clinical trials, what we might be seeing, and then finally, the last slide, I just wanted to mention, that this big problem, the big problem that is, usually the biggest one in people.
18:12
Suffering from code, is there fatigue.
18:14
And we really know a lot of things can cause fatigue, but we don't know exactly how that happens in the body that we get to. Our sense of fatigue actually develops a lot of things that trigger it.
18:29
We don't really know how to, how to prevent it, but actually studying that in kind of the general aspect, too.
18:36
So the basic science of the T would be really help us now, I think, as we're facing this problem of the Post coven situation. So, with that, I'd like to thank you for your time, and happy to answer questions.
18:54
Thank you, doctor ... for NIH's Leadership on that Recovery initiative. And we look forward to continued opportunities to share the research findings to inform our response.
19:06
Next, we will hear from doctor Bratcher are a distinguished visiting Executive partners, former Assistant Secretary for Health, Number of the White House Coronavirus Task Force and Admiral US. Public Health Service. We're so honored to have him with us today to share the important work of the covert 19 Patient Recovery Alliance.
19:29
Well, thank you very much. It is an honor to be here with all of you.
19:33
Um, I, of course left the Administration when the administration changed, but one of my interest was, of course, not only on the acute coded and ending the pandemic, but the consequences long term of coded.
19:48
Let me clarify one thing.
19:50
Although you've seen the numbers of 43, 47 million people having covered in the US, let me correct that because those are the numbers reported to the CDC.
20:00
The actual estimated numbers of patients who have been infected and survive coded in the United States is more like 140 million people.
20:10
There was a tremendous underestimate of reporting that's supported by serological assays.
20:15
So, if you look at the estimates that 30 to 50% of people have some issues with law encoded, you're talking in the range of 30, 40, 70 million people in the United States that have persistent symptoms greater than 28 days.
20:30
So, while the NIH performs the absolute gold standard studies that you just heard, we have to realize that there are tens of millions of people right now who need help, And we need to organize that, albeit with an insufficient and an exact knowledge in order to provide care and prepare the health care system.
20:50
So, why are we concerned about it? I would say, basically, five reasons. Number one is the effect on patients. I'm a pediatric ICU physician. I've taken care of patients my entire life, and we should all be patient centric in our concern.
21:05
Secondly, there are tremendous issues on return to work and disability.
21:09
We see right now that there was a tremendous need for individuals to re-enter the workforce, sir.
21:19
Health disparities are a main concern of ours. We know that covert has disproportionately affected people who are African Americans, Hispanics, American Indians, Alaska Natives, and the history, and the disparities that they have encoded are bound to be amplified and long coat.
21:37
Fourth, is healthcare cost and utilization. We will have tens of millions of people who will be entering the system in fifth.
21:44
The healthcare sector impacts. How do we organize the healthcare sector? Do we have long call the clinics, do we have telehealth triage? How do we care for this 30 to 50% people who have potentially walk of it? Next slide.
22:02
So, to work on these issues, levit partners is a non partisan health policy consulting firm.
22:13
Um, one of the major activities is to build alliances that are absolutely multi sector in nature to attack problems, and to define policies that need to be implemented, both on the near term, the midterm and the long term.
22:32
So we get levit started Patient Recovery Alliance.
22:35
It was started before I joined them in the fall of 2020, with the mission of supporting the multi sector, both government and private sector leaders, as we prepare to care for people with long code.
22:49
Of course, we're looking at gaps, but we're also looking at opportunities, not just on an academic kind of basis, but what really needs to be done, and how to do it, and how to inform Congress and the administration on how to get that done over the various time periods. Next slide.
23:08
We have many alliance partners.
23:11
And what we try to do in our alliances is not necessarily to have every group represented, but have all the major sectors represented in a relatively small agile, but very effective group that works intensely. So what you see on the right side, is their patient advocacy groups, like survivor core.
23:31
There are providers, like University Hospitals of mine, Sinai Health System, Johns Hopkins.
23:37
Um, there are data aggregators like Arcadia, which I will talk about.
23:43
They're also payers, and they're also providers and non-profit organizations. We delivered an interim report in 20 21, and I think the website for that will be on the next slide.
23:59
And it was to provide a background on solutions and interim recommendations, which we did present to the White House into multiple stakeholders in Congress. Next slide.
24:12
The recommendations were organized in really two domains of focus, models of care and payment systems.
24:19
Next slide.
24:23
You see the website at the bottom curve at 19 patient recovery dot org. That will give it to you. So the objectives of the models of care are as listed to inform the development of care models, into identified very specific federal policies, and then second, payment systems.
24:40
How do we develop payment strategies and policies to ensure that individuals with ... receive adequate care?
24:46
And I'm not going to go through all the recommendations, but I will go through a few of them on the next slide.
24:55
Um, so, the models of care, these are individual areas, but I'll just describe them in general, because we really don't have time to look at all of them, first of all, ensuring optimal care for the underserved.
25:10
This is very important to provide if you have 40, 50, 60, 70 million people. You're not going to be able to do this through long covert centers and specialty hospitals.
25:19
You're going to need to get this into the community and we know the community, particularly the underserved community, gets much of their care from FQHCs or community health centers. So, part of the policy is to provide funding for FQHCs or community health centers in order to provide the holistic care and screening that are needed, the same thing for primary care practices.
25:42
We also promoted technical assistance programs much like we did for opioids at a state by state basis that people don't know how to take care of patients with Long Cove it. And it's very important that there's a loop between what is learned by the NIH and other groups. Back down to primary Care with a holistic Technical assistance program.
26:01
Community grants for screening, Very important. People don't know about long coded. I have met so many people, or I've been in contact with people, including very educated people, with very high paying jobs. He said, My know, after I had told that I started having these severe headaches, that have been debilitating migraines 2 or 3 times a week.
26:22
They never even thought they could potentially have Long coven. So we need community awareness so that people who are experiencing these fake signs of fatigue or depression, or sleeplessness, can actually be channeled into the system.
26:35
On the second point, we really need to understand how people are covered by their long code, that, what is the distribution of patients? Not just who has long coded, but are they covered by Medicaid, or they covered by Medicare? Are they private? Do they fall on the gaps?
26:50
And if they fall on the gaps, how do we solve those gaps?
26:54
Then ongoing research and education is, of course, very important.
26:58
Now, in addition to the NIH type of research, we also wanted to create an inter-agency task force on in public awareness campaigns that would, again, promote awareness and the ability for people to receive their care. Next slide.
27:18
Nancy Ann Deparle, who was President Obama's deputy chief of staff for policy and also ran CMS.
27:25
I ran the payment priority workgroup that really looked at a number of very specific issues that should be considered.
27:36
one of them, which would be very interesting, is to create is to allow for long covert patients to be seeing NC snips, the Medicare Chronic Conditions Special Needs Plans, to include them in that. To provide the ability through Medicaid that they can have a meta, they could have Medicaid health homes through legislation.
27:59
That would focus as the Director of Care, and a number of other different recommendations, including the Center for Medicare and Medicaid, long code, the demonstration project, since we don't know how to care for patients, well, let's try some projects based on current knowledge and awareness.
28:19
Let me say that, with Curious to know, that came out yesterday after we had briefed the Committee, or multiple times, that five of our policies work directly, put into the ... 2.2, 2 legislation. That includes the sources of Coverage survey.
28:39
That includes a learning collaborative that the secretary would bring together to bring together health systems, patient groups right now.
28:47
So, while the NIH is providing the definitive gold standard study, we can have a national learning Collaborative to promote research in pediatric populations, which we know the NIH is doing, Which is a fantastic to direct the national academies to conduct a study to evaluate the presence and causes of disparities in Long Cove it. And finally, to have national education and awareness campaigns.
29:12
So these are just some examples of how we put the policy ideas into practice. And we're so pleased that five of these policies directly briefed made it to the cure to legislation. And we look forward to working with the White House and Congress on evaluating and potentially implementing more of these policies. Next slide.
29:35
For the last couple of minutes, I want to be a little bit provocative and that is to talk about the role of covert 19 vaccination in the prevention, or treatment of long cold.
29:45
It is, is there a role, Because, I think there are sources of evidence that we can get, albeit not randomized, controlled trials, but that our hypothesis generating, that may really give us a hint at the role of what is causing lung coding.
30:01
First of all, let me say that vaccination will prevent coven, and the best way to prevent getting long code, it is to, is to prevent getting covert in the first place.
30:11
So, getting your vaccines to vaccines, and, for most people, and I would suggest, the FDA will probably approve the third jab for all, getting your full courses of immunization is your best way to prove that long code.
30:25
Now, let's look at the next slide.
30:27
There's a second mechanism.
30:29
And this was pointed out by a study in over one point two million people in the United Kingdom, And if you look down at the graphs, I'll have, you look at this left side, the symptoms lasting, less than, greater than 28 days, This is really long coding.
30:46
And it goes to younger adults and older adults.
30:49
And what you're seeing is if you've had two doses of Copen vaccine, even if you get coke after the vaccine, your chances of getting long cope it are significantly reduced.
31:01
So, this is a second mechanism.
31:02
Number one, vaccines, prevent you from getting code it, but secondly, even if you get covert after vaccines, your long covert chances go down significantly.
31:13
Now, it says, here, which is very interesting, is that, if you only get one vaccine, it's not so good.
31:19
But if you get the full course of two, we don't have data on three.
31:22
You could actually prevent long code.
31:24
Now, why might this be the case?
31:26
one of the leading hypothesis is that there's persistent anuj anemia that has chronic inflammation. We know that you can be positive in your nose for many weeks, or even months after a coven infection. And there are anecdotal data that shows that the viral nuclear material, the RNA can be present in the gut in many other places for many, many months.
31:48
So, it might make sense that a vaccine could help amount sterilizing immune response so it can prevent long cov it by getting rid of all that energy anemia.
32:01
Now, that's a hypothesis, but it's an important one.
32:05
Most recently, the next slide, which was just published last week, and it's not peer reviewed on the next slide, please.
32:12
This looked at a French cohort, again, of hundreds of thousands of patients, but they did a case control study of all people with long cov it, of people who got vaccinated during the course of long coat.
32:25
And what you see on the right side here are the recovery curves.
32:28
This is the rate of complete remission of their long coded, and these are vaccines at least three months after the start of a lot of being infected with ....
32:37
So this is long in advance in the future.
32:40
What you see here is, even three months after coven. If you get vaccinated, the rate of remission of law encoded was double.
32:49
If you were vaccinated.
32:50
So in addition to being a preventative, this study, suggest possible. It's not randomized control. It's not peer reviewed, yet. But that a vaccine, even if you have long code, it could be therapeutic. And this matches some empirical data by patients.
33:05
Finally, the last slide is that, in addition to these studies, as part of the Long coven Alliance, if I can have the next slide, please.
33:18
Arcadia, which is A member of the alliance is an aggregator of de identified clinical data.
33:29
It's doing a study looking at over 150 million patient records that are amalgamated from health systems from practice management systems from claims data eligibility data.
33:41
And what they are looking at right now is one year's worth of covert activity in the United States, predominantly before Delta, because it takes time to evaluate these patients.
33:52
And what they're looking for and looking at, and we'll publish within the next week, is a retrospective analysis looking at whether koven vaccination after the onset of Kobe can actually prevent in this very large database, the development of Long coven.
34:10
And if it can help prevent, are there any time windows, Um, you know, I can't scoop the publication, but their data are highly provocative and will be in every media, as soon as it's out within the next week.
34:24
So, that's it. I want to thank everyone for being here. I think we have to go hand in hand here, This is a time where soft science needs to drive the policy.
34:35
And that's what we've done from the policy side, but as they say, the evidence base, but if you don't have evidence, make some.
34:42
We're trying to make some here by looking at the sources we have. Again, while we anticipate greatly the tremendous gold standard research being done by the NIH as outlined to you in the previous presentations. Thank you very much.
34:58
Thank you, doctor ... for your leadership both during the pandemic response and also helping to lead these efforts to collect data and develop new models of care for patients living with ....
35:11
We, one follow-up question we had that came in for you, if you could give a quick comment, um, you know, why?
35:23
What are you seeing? Or what data would you like to see in terms of the recent news with the emergency use authorization for the anti viral **** and the potential for that in terms of preventing long Cove and symptoms?
35:39
So, first of all, I could not be more excited about more tools coming on hand, both the Rich back Merk drug, potentially, and the Pfizer drug. What I'm encouraging everyone to do in the monoclonal antibody trials, as well as in these trials, is to not only look at the acute resolution, but look at one company.
36:00
You know, these trials normally stop at 30 or 60 days to look at the resolution of the acute illness, and it would not be much money.
36:09
And if they need money, I hope the NIH will do this, is look at the Incidence of Long coven, and those that were treated, um, with the drug versus not.
36:18
The second point is, yes.
36:21
If there is persistent viremia, even at a low level, which is causing long coded. And if you believe vaccination during long kogod helps, that certainly suggests that there is a possibility. This needs to be tried in a randomized control trial, that patients with long Cobain, potentially early on, might respond to antiviral medications or monoclonal antibodies.
36:44
Now, let me say, this is all speculum, the only data for vaccination is what I told you about. These are not randomized controlled trials. But again, in the midst of a pandemic, we often don't have the advantage of no waiting three years for a controlled trial. We have to look at some of the best data from unusual sources, including these massive claims data and databases that have 150 million people in them and look at that. They're not hypothesis proving, but they are hypotheses generating.
37:13
So great question needs to be looked at.
37:17
Right now, we could do it just by looking at the long term effects after treatment. And in the future, I would say, a very early randomized trial of people with long cov it being treated versus not treated.
37:30
Great, Thank you.
37:32
We're having some technical issues, getting our last speaker back on by, while we wait for her, doctor Corey said, Did you want to weigh in on that and how that might impact some of the research that you're doing?
37:48
Give me about the antiviral.
37:52
Yeah. I think I think Fred's got it right?
37:54
That, you know, an easy answer could be persistent virus.
38:00
And an antiviral could be the answer.
38:04
That being said, there's a lot of assumptions that go into that statement, which we don't know the answer to.
38:09
So, I think the first thing we need to do, I think those autopsy studies are going to be crucial.
38:17
You're kinda OK, how can we?
38:20
The autopsy studies are very crucial in looking at tissue to see where if there is virus, whereas at hiding.
38:28
And but then, yes, there is evidence of viral replication.
38:34
Then I think an antiviral would be a real first thing to try.
38:42
Great. Another question. Are there other health systems from other countries? I know, you know, some of you, doctor Tamara, presented some data from other countries.
38:53
Are you are you, what are the other countries that you're monitoring for, insights on their Long coven research that we should be thinking about or looking for going forward?
39:06
Yeah, I think for sure, you know, because covert is Global and so, the problem we're talking about is global, and so there are a lot of people trying to study this, this problem, now, And I think, you know, the UK.
39:24
Because they have a national health care system in terms of moving to treatment.
39:29
That's why, you know, I showed their slides because they're, they're already got to that kind of a level where they're developing guidelines for practitioners and then and then yes, I mean, I think in terms of if there is persistent viruses, I suspect those groups around the world trying to understand that now.
39:51
So we, we, we really monitor everything that that we can find that they give us clues.
40:01
Thank you. I think doctor ..., are you back with us?
40:07
Can you hear me?
40:08
Yes, we can.
40:10
OK, we're going to Switch now to hear from doctor Heiss, Florida Blue Senior Medical Director. She oversees the company's health equity strategy and has also been a clinical lead for their cover 19 response. So please share with us today to share their efforts to address that 19 ... doctor tastes.
40:37
Yeah.
40:50
Yeah, ... stayed with us.
40:58
Kathryn, I believe that doctor size was just disconnected and again, I apologize for the technical difficulty with her phone line continues to be disconnected. I apologize.
41:08
That's OK.
41:11
We can switch back to the Q and A and if she just let us know if she's able to to call back N.
41:22
So for doctor doctor ...
41:25
instructor jaguar, know we've we've talked a lot about the workforce issues that we've been facing with the pandemic. We had a few questions come in about, What are you, what are you thinking about as potential health care workforce issues? We should be concerned about related to treating long covert and are there are you seeing any sort of emerging roles? Yeah, or a community health workers or other types of workers that we might need to really kind of sustain sustain the workforce going forward.
42:02
So, let me just take a first shot at that.
42:04
Um, I think we have a workforce issue across the board, particularly in underserved communities, um, for a holistic kind of provision of services, as doctor ... said.
42:20
You know, these are have many different manifestations including depression, mental illness, sleep disorders that require much more than just a pulmonologist. You know, we require social workers. We require behavioral therapy, and all these are in short supply across the country and we we know that already even even before this.
42:45
So, I do think the workforce issues are significant.
42:49
It will be amplified, particularly in primary care for underserved communities, particularly in areas like behavioral health, social work, community health workers. But I think it just magnifies the problem we've had in this country for for decades and potentially with the attention brought on this. We can start solving some of those some of those issues as well.
43:13
Yeah, I would I would definitely agree, right?
43:16
Then, I would just point out that, uh, as I mentioned earlier that we have at NIH been working with the ME CFS community and they have they have been of us, astrocytes, by medical system, unfortunately there.
43:39
Because, you know, I think doctors just get frustrated when they don't understand the problem.
43:44
And and they feel that that unimpaired sometimes to actually help them.
43:53
But, you know, that's what doc is a forest, is to help people even even when you don't have a solution to their problem, to try them manage it with them.
44:03
And then, yes, but that takes that takes a real special doc and, and, and a support system.
44:10
And, and the ME CFS example is what we don't want to see happen, and I'm hopeful actually that that covert is going to bring a large army of people to understand these type of problems that will be helpful to people who suffer from them, independent of Cov it.
44:32
But I would say that this is a weak link in our medical systems, caring for people, with a period of symptoms that are difficult to put together.
44:41
You just have to manage, you know, day by day.
44:43
It's very time consuming, but very important to do that.
44:47
And our medical system is not built, unfortunately, very well, the handle this group. So.
44:53
I think breadths ideas about developing better systems of care are important.
45:01
covitz for sure, but I think they'd have great, positive ramifications in the future as well.
45:08
Right? And let me just highlight on community health centers, I'm a huge fan of community health centers. They take care of, one third of the people in poverty in our country. 30 to 35 million people a year.
45:20
But their reimbursement mechanisms are really on a per patient basis. They do not have the kind of financial resources to take care of these complex patients.
45:29
So if we know the underserved and the socio economically deprived are, the ones who get coded mostly, they mostly go to community health centers. We're going to need to support them financially in order to spend the time to get the social workers, community, health, workers, behavioral workers, to, to work with these groups of patients and to create the referral system, because not all wanko that is equal.
45:54
Some may be able to be treated systematically, some will resolve the ones that really need specialty care and need to be referred to that specialty care, whether at a major academic health center or not. So, these are really the nuts and bolts. It takes a special person to do this. But it also takes time and money.
46:11
And we have to arm, particularly our health centers and primary care practices to be able to build the teams necessary to care for these patients compassionately and hopefully effectively as more evidence is generated.
46:28
Great.
46:29
Thank you, We had a question come and about, you know, we've we've long faced sort of this, this issue of misinformation, disinformation, and how I don't know if this is something that the Patient Recovery Alliance is thinking about, too. But how do we continue to permanent misinformation disinformation, about long code that especially as research continues to emerge?
46:54
So that was exactly part of our recommendations.
46:58
And one of those recommendations was actually put it into cure to zero.
47:04
And it specifically says, directs the Secretary HHS to develop and disseminate information regarding awareness incidents, common symptoms of long code, it, as well as the availability, as medically appropriate treatment options for a long code that requires the CDC to develop and disseminate to healthcare providers regarding long qubit. You know, it's basically just an accountability provision.
47:27
But we really do, we, we've I think we've all learned with vaccines despite everyone's best intent, that misinformation is there.
47:36
And because, again, of the lack of true, you know, there, at least maybe the NIH has one, but there's no diagnostic tests for a long coat.
47:46
It's a symptomatic con. So you can't draw blood tests.
47:48
So whenever there's this nebulous diagnosis based on clinical symptoms, there's always room for misinformation, prejudice, bias, among the population and among healthcare providers. So we do think public awareness is extremely important.
48:06
But it's also extremely important to get the evidence that the NIH is doing, so that the public can be made aware of, you know, what the real facts are.
48:15
Right now, we have a lot of uncertainty, but even that uncertainty.
48:20
The most important thing I say to people as long covert.
48:22
It's real, um, that if you have symptoms after having coded, this is, this is not, you know, quote in your head.
48:31
These are true physiologic inflammatory manifestations of a very severe widespread disease and you deserve treatment for that. Just like anybody with diabetes or cancer. We just gotta get the system geared up to give it to you, and I'd love to hear Walter's comments about about that.
48:51
Yeah, I totally agree and you know, I think that's what the ME CFS community have been fighting for years that people didn't believe them.
49:00
... prove that it's real time, even.
49:03
Now, you can't, You can't, it's just impossible to argue, argue it away.
49:09
So, but that's, and that's the first step towards getting people to take that treatment and the care of these people seriously.
49:20
But we need a lot of people, I mean, as the numbers you've put out there, you know, those are staggering numbers.
49:27
And so we need, you know, primary care physicians who get, know, expert and care of folks who are suffering from this symptomatic condition.
49:38
But I did want to also add one other thing in terms of mist.
49:42
Information is that you have to be careful that that a patient's symptoms, after they've had covered, you just say, Well, it's law uncovered. Nothing we can do about it now. We'll try it.
49:58
physical therapy, but But what you don't wanna mess is, uh, is another condition and hidden, That just happened that occur after you've had cov it, and certainly, we've seen that happen.
50:11
So, yeah.
50:12
So, the first step is always because covered right now, postcode has a diagnosis of exclusion. As Brett said, there's no test for it.
50:20
The diagnosis of exclusion, that means you have to exclude the other things that could cause these kinds of symptoms.
50:28
Know, one of the biggest causes of fatigue is cancer, and you don't want somebody chalking up fatigue, and somebody who has cancer, to the fact, that, well, it's probably post coven.
50:38
So it's it, the misinformation, piece of this is important, even in the medical system, at that point.
50:50
Great. Thank you. And we talked a little bit about mental health, the earlier could you X We had a few questions coming in just about the implications for mental health for patients wetland Coburn.
51:08
It's so.
51:10
So that, there have been studies, looking at new diagnoses, in the psychiatric realm, have to cower.
51:19
And now, as you can imagine, there's a big increase if you compare it to, say, the flu.
51:29
People with cover much higher increases developing anxiety, disorders and depression, and some of it's actually more like post-traumatic stress disorder, as well as I mentioned, people who had a RDS even prior to covered, post-traumatic stress disorder was extremely common.
51:53
So, so, I think we have to consider the person's normal response to an insult as part of the illness.
52:04
And the worst thing I think it can do is, too, no, say, Well, that's just depression. That's in your head.
52:12
I mean, it doesn't make any sense. Medically, everything is in your head. There's no such thing because that in your head, it doesn't exist.
52:20
But here's a great example.
52:21
I think we have a medical condition and infection and you have all these components which are connected to having the has an infection and they have to be seen as, you know, you know, integrative medicine is, is really how you have to attack this problem?
52:40
And that includes the mental health, just as much as it includes a sleep disorder or the pain syndrome.
52:46
And I think it's a great example of how in our country, we've, we've really made the mistake of trying to separate the psychological and psychiatric side from, quote, unquote, the medical side. It's it.
53:03
It really makes no biological sense at all, and this is an example of how, how we have to work with them together.
53:11
I couldn't agree more.
53:12
Can I just ask you briefly about some of the data that potentially links could live with an accelerated, you know, incidence of dementia, particularly in older people? What do you make of that?
53:28
Right, so that, yeah, that also came out from these big electronic health record data, so there's an increased incidence of dementia, and people have had covered, compared to, say, It's the flu.
53:43
Now, I used to run an intensive care units used to run intensive care unit, but you had had kids, and I had older folks, and it was very common that an older individual would develop a severe infection, get an intensive care unit.
54:01
And they would never get back to their baseline mental status.
54:06
We always side, although, you know, we can't say we knew, we always thought that there was a degenerative process in that elderly individual that got no tripped over tipped over the edge by the medical illness.
54:21
And so I think that that is part of the component here.
54:25
The other part of it is that in people who get in the Hospital with coven, um, some of them actually present with a delirium.
54:35
So almost like a psychosis but they are confused and not making memories agitated.
54:43
In the hospital they require extremely high doses of anesthetic agents to maintain, you know, just safety in the bed.
54:53
And those folks, also, when I understand the higher incidence of not getting back to normal mental function again through their normal mental function again.
55:05
So I think the brain actually can take a hit in code.
55:10
The Autopsy Studies show that virus doesn't doesn't kind of attack the brain.
55:18
say, as you would see an encephalitis, but it does affect the blood vessels that supply the brain.
55:25
And it's the most vascular organ in the body. And they become leaky. You can see leakage, and you can see that triggers inflammation around blood vessels.
55:35
You can see's very tiny micro strokes, micro hemorrhages, and that and so these are the kinds of things that certainly could contribute to to an aging process, whether it's all simas, Lewy body disease, vascular disease, so I think that's probably accounting for some of this, right?
56:01
Great. Thank you. Well, we are out of time.
56:04
We do apologize for the technical issues with Chapter Chase, but we, Well, I love to find a way to record her presentation and try to send that out to everyone, and her slides are available on the website. So, I do want to thank our excellent panelists, speakers for being with us, today, and sharing their valuable work and perspectives, and thank you to our audience for joining this discussion. Your feedback is important.
56:31
Please take a moment to complete a brief survey that will open on your screen after this, and then, you will also, we also will be sending out a recording And you can access the slides, as well. So thank you all for joining us today.
56:49
Thank you.
56:50
Very important discussion to have.
56:53
Yeah.
Speaker Presentations

Walter Koroshetz, MD
National Institutes of Health

Brett Giroir, MD
Leavitt Partners

Kelli Tice, MD
Florida Blue
An ASL interpreter is available
More Related Content
See More on: Coronavirus | Health Care Coverage