Webinar
The Challenges of Aging During COVID-19: Long-Term Care, Vaccination and Isolation
Time & Location
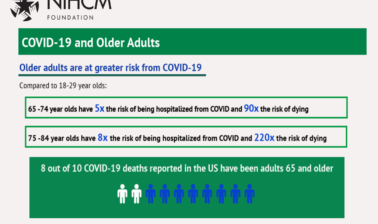
Since the beginning of the pandemic, the danger COVID-19 poses to older adults and people living in long-term care facilities has been of great concern. COVID-19 has claimed the lives of more than 125,000 long-term care residents and staff and 8 out of 10 COVID-19 deaths reported have been among adults aged 65 and older. Now with two authorized vaccines and the CDC recommendation of older adults for early vaccine access, there is hope, but there are still challenges with distribution. It is also necessary to address the pandemic’s mental health impact on older adults, particularly loneliness and isolation. While older adults have reported less loneliness than their younger counterparts during the pandemic, about one in four report anxiety or depression due to the pandemic. Speakers discussed:
- Overview of COVID-19’s challenges to long-term care and the future implications for nursing homes
- Vaccination and vaccine distribution challenges for older adults
- A health plan’s efforts to address pandemic isolation and loneliness
Caitlin Ellis (00:00:00):
Thank you and good afternoon, I'm Cait Ellis program manager at the National Institute for Health Care Management Foundation. On behalf of NIHCM thank you for joining us today to explore this important topic. Our goal is to share information on the unique impact of the COVID-19 pandemic on older adults. And to share actionable strategies to address challenges around long-term care facilities, vaccine distribution, and increased levels of loneliness or social isolation. Throughout the pandemic we have seen the older adults are at a heightened risk for COVID-19. Approximately 8 in 10 COVID-19 deaths reported in the US are individuals 65 and older. And a disproportionate number of deaths are in long-term care facilities. Less than 1% of the population lives in long-term care facilities and it accounts for nearly 40% of deaths from COVID-19. Recognizing the risks, vaccine distribution guidelines have prioritized long-term care facilities and older adults. Yet the rollout has been met with challenges, including staffing shortages, scheduling issues, and vaccine hesitancy among older adults, but also among facility staff.
Caitlin Ellis (00:01:12):
This expert panel will provide insight into the ongoing physical and mental impact of the pandemic on older adults. And outline some key steps and strategies for addressing the challenges of the pandemic and future implications.
Caitlin Ellis (00:01:26):
Before we hear from them, I want to thank NIHCM President and CEO, Nancy Chockley, and the NIHCM team who helped to convene this event. You can find biographical information for all of our speakers on our website, along with today's agenda and copies of slides. We also invite you to live tweet during the webinar using the hashtag agingCOVID-19.
Caitlin Ellis (00:01:48):
I'm now pleased to introduce our first speaker, Dr. Tricia Neuman. Dr. Neuman is a Senior Vice President and Senior Advisor to the president at the Kaiser Family Foundation. She has a widely cited Medicare policy expert and serve as executive director of the foundations program on Medicare policy, where she oversees policy analysis and research pertaining to Medicare and health coverage and care for aging Americans and people with disabilities, Dr. Neuman brings extensive experience and expertise to this topic, and we were so grateful she is with us today to share her work and perspective. Dr. Neuman.
Tricia Neuman (00:02:26):
Thank you, Cait. And thank you everybody at NIHCM for convening this panel on a really important topic that affects each of us directly or indirectly, professionally and personally. I'm so honored to be here to be with Vince Mor and Paul Kaplan. And I look forward to hearing their remarks in a few minutes.
Tricia Neuman (00:02:51):
Can you turn to the first slide, please.
Tricia Neuman (00:02:56):
As you've just heard COVID is taking a disproportionate toll on the older population. COVID-19 cases and deaths are now raging across the country affecting all of us in all states. But from the beginning, the pandemic has hit older adults fairly hard, not just because they're at increased risk of serious illness and death, but also because of the collateral damage that comes from social isolation and all the lifestyle changes that have adverse effects on older adults, as we'll hear a bit more about later.
Tricia Neuman (00:03:35):
Looking here at this first figure, what you can see is that older adults accounts for about 14% of all cases, but 81% of all deaths. This is an issue that clearly affects older Americans and presents challenges for those with and without the virus and their families. And within this older population, some are clearly affected more than others, people of color for example, account for disproportionate share of cases and deaths. And as we're going to focus on today, people in long-term care facilities, mainly older adults and the people who care for them, have been ground zero since the first outbreak.
Tricia Neuman (00:04:23):
Can I have the next slide please.
Tricia Neuman (00:04:28):
KFF has been tracking the spread of the virus in long-term care facilities since it started last spring. Where are we today? As of last week, more than 130,000 deaths have been clocked in long-term care facilities. This is both residents and staff and as you heard earlier, when Cait was doing her introduction, long-term care residents and staff account for 6% of all cases, and now it's about 38% of all deaths. This is down from the spring when it was about 46, 49% of all deaths, but it has not fallen much below where it is today. And in more than a dozen states long-term care facilities account for half or more of COVID-19 deaths. This is a true issue for people who are focused on the long-term care population and for all of us who may have friends and family members, parents, and grandparents who are in nursing homes or assisted living facilities.
Tricia Neuman (00:05:38):
Can I have the next slide, please.
Tricia Neuman (00:05:44):
The surge new cases nationwide that we've seen this winter is having spillover effects in the long-term care community. We're not done with this yet, not by a long shot. After dip in the summer, what you can see in the top portion of this slide is there is now yet another increase in cases among residents in nursing homes. And if you look at the bottom part of the slide, you can see there's also an increase among staff. So we are seeing a reflection of what's going on in communities across the country, where cases are rising rapidly and this is now once again, entering the doors of nursing homes and assisted living facilities. Tragically, but not surprisingly, this surge in new cases is leading to a surge in deaths.
Tricia Neuman (00:06:41):
Next slide please.
Tricia Neuman (00:06:48):
This next slide, this slide that you're looking at now, comes from a new analysis put up by my colleagues at KFF just yesterday. Where we were looking at new deaths per week over the course of the pandemic. And what you can see is that after a lull that took place in the summer, where new cases started to level off, we are now seeing an increase in deaths in longterm care facilities, just as we are seeing an increase in deaths nationwide. And unfortunately, while we don't have new numbers yet for January, we have every expectation that the green line, which is the line for new deaths in long-term care facilities, will continue to tick up in the early part of 2021.
Tricia Neuman (00:07:44):
Some states peaked earlier in the year in April when the pandemic first hit, others are peaking now. And we're also tracking where these peaks are occurring and they're occurring mostly in the South and a bit in the West. As you might imagine, since you've been following press reports I'm sure of the surging cases out West.
Tricia Neuman (00:08:13):
Can I have next slide please.
Tricia Neuman (00:08:18):
So it's no surprise in response to sort of the tragedy that's taking place in nursing homes across the country that CDC, the Centers for Disease Control, put long-term care facilities at the front of the line for vaccines, including residents and healthcare workers. The initial priority group that's 1A includes this population followed by people 75 and older and other workers and people 65 and older. Earlier this week, HHS revised its recommendations to give priority to people 65 and older, significantly expanding the priority population, remembering that there are 50 million or so people in this age group. So far, this announcement seems to have generated at least as much confusion as optimism among older people, as they try to navigate the systems that are sort of in place, trying to figure out if they're eligible, when they can get vaccinated, how they can sign up. And based on what we're reading in the press and early reports from others, this confusion is contributing to underlying fears and anxiety because people are eager to get the vaccine and not knowing how to do it. And there are also real questions about suppl not being adequate to meet the demand.
Tricia Neuman (00:09:46):
Next slide, please.
Tricia Neuman (00:09:53):
This is a map that shows the significant variation across states and where they are in their priorities when it comes to older people. And you can see that states are pretty much all over the place in terms of what age group they're starting with. The greens states are currently administering to seniors and the blue states are sort of next... seniors will be coming soon. This is a tricky map to look at, because what we do know is that within states, there's a lot of variation county to county. And we also know that even though people may be eligible for vaccines. They're not necessarily getting them because of supply constraints.
Tricia Neuman (00:10:42):
So again, you may be picking up in the press, we're certainly picking up many stories about a lot of confusion out there in terms of people wanting to know if they can get the vaccine, when they can get the vaccine, how they can get the vaccine. Having heard that it's now available to people 65 and older. And I think there's some fair amount of miscommunication in terms of who do they call in their state to get to find out.
Tricia Neuman (00:11:14):
Can I go to the next slide, please.
Tricia Neuman (00:11:19):
In some ways vaccinating the long-term care facility population should be a lot easier than vaccinating the entire 65 and plus, 50 million people in the United States. Federal and state governments pretty much know how to find long-term care facilities and the residents that live in them and long-term care facilities know the staff that are working there by and large. So to meet this highest priority the federal government set up a new partnership with national chain drug stores, Walgreens and CVS for starters, to distribute vaccines to nursing homes and assisted living facilities and get vaccines into the arms of residents and staff as quickly as possible.
Tricia Neuman (00:12:05):
This is a program that is aiming both at skilled nursing facilities and assisted living facilities and actually other residential facilities. Although states, again, have some discretion in terms of whether a skilled nursing facility has come before other types of facilities. But the idea is to create a nationwide distribution channel to get the vaccines out quickly. In many parts of the country, this is exactly what's taking place. Some states like West Virginia has gone in an entirely different direction, not using this partnership. And I think Vince Mor's going to talk a little bit about the issues around the partnership and what's working and what could be made to work better.
Tricia Neuman (00:12:56):
Can I have the next slide please. Here's where we are now and translate. This is a slide that can change every day and has changed every day because the numbers keep ticking up. When I first started looking at the numbers that were posted on CDC, these are going to be the first two bars sort of on the left side, you can see that as of January 2nd there were 282,000 or so vaccines that were given, the first doses, out of 2.2 million that were distributed, that was roughly 13%. And there was a lot of concern expressed at the time that that's just a very small number and things weren't happening very quickly. Truthfully between January 2nd and January 13th the numbers have ticked up very rapidly. In fact, I just checked the website today and the numbers on this slide, which I think I sent in yesterday are out of date. As of yesterday, at least there were more than 1.2 million doses that were given out of 4.7 million doses that were distributed, that's roughly 26%. So over this period of time, we've seen an increase from 282,000 doses given to 1.2 or so million doses given. By any standard this is really good news. This is going in the right direction. It's a big increase. But we still have a way to go.
Tricia Neuman (00:14:31):
Even for this population, that's relatively easy to find, 1.2 million is not enough to vaccinate the two to three million people living in long-term care facilities, both nursing homes or assisted living facilities. This means that many older adults who are living in these settings are still waiting for their vaccine and it also suggests that the three million workers who are caring for residents in these settings are not nearly getting to where they need to be to get vaccinated, based on these numbers.
Tricia Neuman (00:15:10):
Can I have the next slide, please.
Tricia Neuman (00:15:19):
So speaking of these workers, we've learned and heard that hesitancy is a concern and hesitancy actually is a very serious concern. This is based on a poll that was conducted by newly launched KFF Vaccine Monitor Project. And what you can see here, this is a poll of the general public. Overall 27% that they would probably not, or definitely not get the vaccine. The good news is if you look by age, the number's much smaller among people 65 and older, 15%. And what we're hearing is that older people are indeed doing this as much as they can to get in line, to get their vaccine-
Tricia Neuman (00:16:03):
... Doing as much as they can to get in line, to get their vaccine, including in nursing homes. But hesitancy is a real issue and the rates are higher among people who are black, among people who are living in rural areas, and among healthcare workers. And there's also quite a partisan divide in terms of willingness or hesitancy to take the vaccine. So these issues that are affecting people generally in the public are also affecting people who are working in long-term care facilities. We're hearing that people are really genuinely worried about side effects, fast approval and the safety of these vaccines. And I think we need to hear what these concerns are, we need to address these worries directly, and most likely use trusted messengers to deliver these messages so that more people have confidence in the vaccine in order to protect themselves, in order to protect residents in long-term care settings, and to protect others in the community.
Tricia Neuman (00:17:08):
Next slide. The same poll asks the questions about what exactly is that was a concern. And what you can see here are the reasons people said. More than half of all people surveyed said they were worried about side effects. 55% said they don't trust the government to make sure the vaccine is safe and effective. 53% says it's too new and they want to wait and see how it works for others. And 51% cited politics. It's played too much of a role in this development. Now this survey was conducted in December and we will be continuing to track the response of the public to vaccines. And we sure hope that these numbers go down, but in the meantime, they are a signal that more needs to be done to educate, to inform the people who are working in long-term care settings so that there's a greater comfort level.
Tricia Neuman (00:18:05):
We had a briefing yesterday where we heard from the nursing home industry, we heard from the pharmacy industry. And what they're saying is this issue of hesitancy is very real, it's not something that people just say may be a concern, it is a concern and something to be addressed. Again, we hope these numbers will shift and we will be tracking them. Finally, while I've been focused mainly on how COVID affects older adults from this perspective of cases and death counts and the rollout of the vaccine, there is another story to be told. Can I have the next slide, please?
Tricia Neuman (00:18:45):
There is another story to be told and Dr. Kaplan will be talking much more about it. But COVID has certainly had a spillover effects on the mental health of older people. Here we see that this was work that was done in the summer. One in four adults ages 65 and older reported anxiety or depression. This was amidst the pandemic. I imagine if we continue to track this, given the suggestions that people stay socially isolated and the anxieties about getting the vaccine and getting healthy and moving onto normalcy, we could see more of this in the future. And I think this is an issue that needs serious consideration as people begin to recover from what's been a big trauma for all of us, including older Americans. Last slide, please.
Tricia Neuman (00:19:40):
So I think there's some good news, some cause for optimism, but certainly major challenges. The cause for optimism, Operation Warp Speed was warp speed. That's great, we do have vaccines and they're rolling out. And the numbers are rising and that too was good news, but they're not rising fast enough as we've just discussed. And they're not nearly rising at what people would like to see as warp speed for that too. The Biden administration plans to invest significant resources for vaccine distribution, and I think there's wide agreement that that will be necessary. But there are also major challenges. Case counts and deaths are higher than at any time during the start of the pandemic. They're surging now, and they will be surging in nursing homes in the early part of this year. Once the numbers roll in, we'll see that for sure. Serious illness and deaths due to COVID disproportionately affect older adults and among people of color and in longterm care settings.
Tricia Neuman (00:20:38):
And that needs that that is something that can help drive interventions and should drive interventions to lower the death count. Strategies are needed to reach harder to reach populations. This is not something that I've talked about, but think about people who are home bound, think about people with disabilities who may be harder to reach or people who don't have online access so they can't reach the portals in order to sign up for a vaccine on the internet. This is a health equity issue. Targeted education is absolutely needed to make people feel comfortable about safety. And in addition to all the very serious physical health issues, mental health remains a major concern and is one that needs significant attention in the future and now. So thank you very much, this has been a really important topic and it's timely that you've held this event.
Caitlin Ellis (00:21:37):
Great. Thank you so much, Dr. Neuman for sharing those sobering statistics, the recent trends and the state level variation and how the vaccine has a tendency of impacting different groups and communities. Next you'll hear from Dr. Vincent Mor, the Florence Pierce Grant Professor of Community Health in the Brown University School of Public Health and Senior Health Scientist in the Health Services Research Service at the Providence Veterans Affairs Medical Center. He has extensive background researching in evaluating the impact of programs and policies and aging in longterm care. Dr. Mor will continue our conversation on nursing home preparedness and COVID outbreaks in long-term care facilities. We're so fortunate that he can be with us today to add his perspective and expertise to this conversation. Dr. Mor?
Vincent Mor (00:22:23):
Thanks so much for this opportunity to present research my colleagues and I have been doing actually since last March, when the pandemic first began to hit nursing homes in the United States. I'm so glad that Dr. Neuman had provided all the backgrounds, so I don't have to do all that background material. So it was really great. Wonderful perspective, and allows me to put a more detailed perspective on how the pandemic has affected the nursing home world in the US. So I have lots of acknowledgements. I'm a researcher researcher, so I have grants from the National Institute on Aging, and each of those large grants have widely different supplements that were made available to us as soon as the pandemic became obvious. And I have to thank all of my colleagues. I certainly didn't do any of this work alone, couldn't have done any of it without them.
Vincent Mor (00:23:16):
Thank you. So what I want to do is give you a background to the nursing home preparedness behind this, and then talk about the competing narratives regarding the cause of the outbreak and how people interpret that. Then the importance of having really good, timely data to basically diagnose the problem of who's at fault, as it were, and then prescribing solutions to ameliorate it so that we don't have the wrong solution, addressing a problem that's unrelated. And then present you some study findings about that, and then I'll talk briefly about the most recent things we're doing as it applies to vaccination. So Americans' perceptions of nursing homes have all been quite poor because they've been shaped by periodic scandals that are local, national. The national news outlets thrill the newspaper reporter more than being able to think something scandalous has occurred and it wasn't in my family. So it was just a big problem. It's often seen as a fault of the facility, perhaps the industry that's for profit, and also that there's governmental failures with respect to our regulation. And I personally have always found it very interesting that we periodically have physician scandals like excessive opioid prescribing. But that in the mind of the public, they don't tar all physicians, yet nursing home scandals do seem to condemn all providers. And that's within that background that the first frame of the narrative began in the US. So the first death in a nursing home was actually from the first death from COVID all together in the United States occurred that we can find, was in a Seattle and Kirkland nursing home. They were a big shock, lots of people die very quickly, and there seemed to be some hiding of what was going on in that process. [crosstalk 00:25:20]
Caitlin Ellis (00:25:20):
Dr. Mor?
Vincent Mor (00:25:21):
Yes?
Caitlin Ellis (00:25:22):
Dr. Mor? This is Kate from NIHCM. Can I just ask that you speak up a little bit? It's hard for some of our audience members to hear you.
Vincent Mor (00:25:32):
Oh, okay. [crosstalk 00:25:34].
Caitlin Ellis (00:25:32):
That's much better.
Vincent Mor (00:25:34):
Okay, fine. In any case, so the notion was that the absence of infection control practices or the inadequate infection control practices were blamed on the facility training and under-staffing, and that then was what was thought to be contributing to the high death rate and the fact that people were becoming infected at all, and inadequate supply and use of protective equipment. So the net result was that the newspapers and Medicare CMS reported that more deaths were occurring in low quality homes, and so this was somehow or another all speak to that sense of quality. And If the interpretation, and if a determination of what the problem is is that it's poor quality, one would actually take a different approach in deciding how to do something about this. And yet the real issue was where these effects were occurring. So this was a classic piece for the New York Times called nursing homes death pits as a part of a long article that was written last spring. And I remember having conversations with the authors, the reporters, and I found that not terribly helpful. And of course the editors came up with the title, not the reporters.
Vincent Mor (00:27:07):
But the issue here was trying to understand what were the determinants of having an outbreak in a nursing home? In an effort to answer that and many other questions, we established a relationship with a large nursing home company called Genesis Healthcare that's located in Philadelphia, but had nursing homes throughout the country. We entered into a collaborative commitment, Brown's analytic prowess would actually help Genesis operations processes so we can both be in constant exchange. So for the past literally nine months, we've been meeting on a weekly basis with clinical leadership, their IT staff and Brown investigators, trying to explore challenges that they're facing, trying to understand empirically what was going on. And by May, we'd already begun doing a lot of different analyses, and those I'll be talking about right now.
Vincent Mor (00:28:13):
So the first thing was to try to find out, "So what are the determinants where an outbreak occurs?" And we published that as a paper already, but we looked at the association of nursing facility characteristics and county prevalence of SARS with the probability that a facility had at least one resident with COVID. And the size of the facility, the number of beds in that facility was strongly related to the likelihood of a transmission. Percent of the residents who were African-American had a very strong effect. And at the bottom of the slide, you'll see that the county prevalence, that is how prevalent the local community is about that, was the most important factor. In fact, all of these other things are largely associated with the amount of traffic associated with people coming into the building who are living in an environment where there's high prevalence of the pandemic.
Vincent Mor (00:29:17):
And so with that in mind, and other colleagues of ours, it's now accepted that the determinants of an outbreak was mostly community prevalence, that CMS and CDC, actually their facility level data is now interpreted with this in mind. So in some sense, the data will help both in shaping basically the agenda and the interpretation, which is a much more positive perspective than trying to "blame the victim." And I was particularly conscious of that because a large nursing home that I work with a lot, it's a not for profit up in Boston, a spectacular place, had been hit with many outbreaks even though they have the highest staffing levels in the state and so on. And so it's really about volume because it's a very large shortage with people coming in from all over the community. And because they're underpaid staff, they live in the poorest parts of town, and it's the poorest parts of town in almost every part of the country that has actually been hit this. Next slide here. So one of the other things that happened, initially people were screening for SARS, for the virus, in the nursing home, as everywhere else, by looking at temperature. And geriatric patients historically have lower temperature, and yet CDC set the average temperature threshold because whether you're in an airport or you're in a train station or you walk into a building and people are checking you, they're going to look for a single threshold, and it was 101. Genesis data has a screen with temperature and other vital signs literally two or three times a day.
Vincent Mor (00:31:10):
So we looked at that and we said, "Hey, the threshold for when people... Their temperature arises relative to when they're tested positive seems to be at a much lower threshold." We did this both in the VA, which is the lower panel of these two slides, and then the upper panel. And on the upper panel in the upper left corner, that's in the Genesis facilities. And the day zero is the date people tested and tested positive. And you can see there's basically a rise, started three days before that temperature. But the day of testing was basically 37.2-
Vincent Mor (00:32:02):
The day of testing was basically 37.2, so the threshold, what proportion of people hit that temperature threshold. So that meant that standard for what CDC is reporting out for what to look for in terms of screening for people with potential COVID had to be lower in the geriatric population. That's now part of their standard approach.
Caitlin Ellis (00:32:25):
Dr. Mor, this is Kate again [inaudible 00:00:27]. We're just having still some sound issues on our end, so if you could just make sure you're holding the mic close to your mouth, that might help a little bit. It just seems to be cutting in and out a little bit. Thank you. I really appreciate it.
Vincent Mor (00:32:40):
All right. Very good. Is this better?
Caitlin Ellis (00:32:41):
Yes, that sounds clear.
Vincent Mor (00:32:43):
Okay, great. The asymptomatic transmission is complicated by... Makes it very difficult to cohort symptomatic positive cases. Initially, we all thought that if you identify patients with symptoms, you'd put the patients who are symptomatic together, and you try to isolate the people who were not feeling symptoms, assuming they were negative. Particularly early on, when there were fewer testing kits available, this was the strategy that people were using to try to protect the people who are "negative." But all of that ignored the fact that there's a lot of transmission from the people who were positive, but asymptomatic. So Genesis began doing these random sweeps where they tested everybody or most everybody in a, building in a wing, and that made it possible for us to identify the fact that there are a very high proportion of patients who are asymptomatic [inaudible 00:01:41].
Vincent Mor (00:33:42):
Here we see that something like, compared to 40 and 31% of the patients who are asymptomatic, during facility-wide surveys only 22% were symptomatic when they only tested people who were symptomatic in that process. Meaning that it's really important to see that in terms of who's symptomatic. Next we also saw that the proportion who were symptomatic was [inaudible 00:34:13] was a very strongly related proportion of people who had COVID in the community, which is that top 5%. I'm going to change my device here. Can you hear me now better?
Caitlin Ellis (00:34:37):
Yes, that is better.
Vincent Mor (00:34:39):
Thank you. So I'm now holding the phone myself. Okay. So for the next slide, we wanted to look at mortality. What determines mortality. In the community population, as Dr. Neuman showed, mortality is the highest amongst the oldest age, but it's also very high amongst those with comorbid conditions. Now, the nursing home population is both old and sick, and also very frail and functionally impaired. So there was a lot of questions about whether or not their immune systems were able to actually manage that and deal with that. But we still see lots of variation in the mortality rate, even amongst this very old, frail population in nursing homes.
Vincent Mor (00:35:25):
So we published this paper just recently, where did it go? There we are. In JAMA Internal Medicine, looking at the risk factors associated with 30 day mortality. Here's probably the most important take home question, is we see three different panels predicting what is the proportion of people dying at each level. So the panel A, you'll see that the highest mortality rate is associated with absolute oldest people. Panel B, the highest mortality rate is associated with those people who are most functionally impaired before, long before they acquired COVID. But cognitive impairment, with the highest level of cognitive impairment was also very strongly associated with the likelihood of mortality. So it's age, physical function and cognitive functioning, all three together actually are probably far more important than any individual disease. So that's one of the reasons the death rate is so much higher in the nursing home population, because they are that much sicker.
Vincent Mor (00:36:38):
We began to look at this issue of declines in mortality, and we've been working with this again in the Genesis facilities. Here you see that the percent of the 30 day death rate, it's in the third column over, started at 26% in the period around March, dropped to 22, then 17. Now it's back down, as of late September, it was back down to 11. That number has begun to, as Dr. Neuman suggested, turn back up a little bit, but what's important here is this is a real trend that's associated with the level of infection out there. But also this is the mortality amongst the people who were positive. So it's not just because there was a gross reduction in the number of cases. The mortality rate per case was also dropping.
Vincent Mor (00:37:33):
This is not attributable to what we call a change in the mix of patients. Rather, this is attributable because we control for those factors. This is attributable to probably better wearing of the protective equipment, and could be that there was a shift in the genetic characteristics of the virus that was more prevalent last spring versus this fall. What is really going to be interesting is as we extend these data now into January, as we're continuing to do that. Really you have to watch that.
Vincent Mor (00:38:11):
Here we see the top line is for the people who are symptomatic, but even the people who are asymptomatic, at the time of diagnosis they end up with a slightly higher mortality rate than the standard. The average mortality rate in a nursing home population. Again, that is also very similar to the community change in prevalence as it moves forward.
Vincent Mor (00:38:35):
So in summary, vaccinations are now well underway in the nursing homes. The early results suggested about 80% of residents are accepting the vaccine. At least in Genesis, virtually all of the facilities in Genesis have had their first clinic, their first opportunity. The complications that are associated with if the patients test positive for COVID, they cannot be vaccinated. That number of people testing positive for COVID, as Dr. Neuman has shown, has actually begun to rise. Complicating the actual process of administering the vaccine as it goes in the nursing home settings. It is also the case that staff vaccination rates are a real challenge. So far it looks to be about 50%, but really huge variation from one building to the other, with this micro culture of willingness to be vaccinated. We're actually running a large, pragmatic trial now trying to reduce vaccine hesitancy, increase vaccination rates, even amongst residents, but also particularly amongst staff. We're in the midst of doing that in about 140 facilities across the country. We're very anxious to see how that works out, because this is a really important thing. as the pandemic is spreading even more aggressively, with concerns about the more infectious variant coming from Britain to the States, already here, also being of great concern. So I'm going to stop there, and leave open for questions, and for Dr. Kaplan to proceed. Thank you very much for your time.
Caitlin Ellis (00:40:43):
Thank you so much, Dr. Mor, for providing us with another level of detail and understanding of how these facilities and individuals have been impacted, and showing us how data can be used to better understand the problem and identify a solution. Our final presentation will be from Dr. Paul Kaplan, senior medical advisor for Medicare Solutions at Florida Blue. Under the leadership of Pat Geraghty, Florida Blue has provided more than 200 million in COVID-19 support in Florida. This includes waiving cost sharing for COVID-19 testing and treatment, supporting non-profits addressing essential needs in the community, and offering all Floridians free access to a 24 hour bilingual emotional support helpline. We are pleased to have Dr. Kaplan with us today to share their efforts to address loneliness and social isolation among older adults during the pandemic, as well as how they are addressing vaccine hesitancy and supporting vaccine distribution efforts. Dr. Kaplan.
Paul Kaplan (00:41:41):
Okay, good afternoon. Thank you very much, everyone. I'm having technical issues with the presentation on your site, so I'm going to ask you to please advance slides for me. Thank you to the previous two speakers, phenomenal information. I know we are due to end at two, so I am going to go fast, and we'll skip around a little bit. We want to leave time for questions. So if we advance to my first slide with writing the physiological impacts of loneliness, I think it's important to recognize the difference between social isolation and loneliness. Social isolation is you're alone. There's no one else in the physical space around you. Loneliness is you can be surrounded by people, but you don't have that good of a connection with them and you are lonely. Obviously the majority of the concerns that we as a health insurance company had in the past prior to COVID, it was around loneliness, and I'm not going to read these physiological impacts that loneliness has on people, but we'll just suffice it to say that clearly being lonely is one of the major contributors to bad health.
Paul Kaplan (00:42:59):
If we move to the next slide, which is the health effects of social isolation. Again, I'm not going to read the words on the slide for you, but what I want to preface everything I'm going to say, is we took the staff that we had that was working on loneliness and social isolation, and when COVID hit we pivoted the way that they did the work. So they were embedded in the community already, and they just kept working. If we go to the slide titled social determinants of health, or SDOH, I'm not going to read everything on here, but again, we all know in the old days we thought that the determinants of health and your outcomes was, did you have a doctor? Did you have a hospital? What more could you possibly need? We've learned over the years, it's all about economic opportunity and stability. Living in a neighborhood that's safe, having a good built environment with sidewalks, access to food, and not living in a food desert.
Paul Kaplan (00:44:12):
Education is not only about education of young kids, but it's also health literacy for adults. We could talk for over an hour about that alone. Then the importance of social and community relationships, which you've heard something about already today. What Florida Blue does is we do a health risk assessment on every Medicare Advantage person every year. And so we ask questions about these five pillars of the social determinants of health, so that we can identify where it is that we can do a better job of assisting our members. If we move to the next slide, which is community health specialists, we have people that are embedded in the community. We have 27 of them at the moment, and we are planning to almost double that, we hope.
Paul Kaplan (00:45:04):
They work with our Medicare Advantage members. Pre-COVID, they would go to members' homes, help them work through the issues around social determinants of health that were driving them to have problems, with a big emphasis on food and food insecurity, and also loneliness or social isolation. This team is highly trusted in the community. When COVID hit, they pivoted, moved over to doing telephone calls or video chats with our members where they were capable. They've received very, very good receptions from our members that we are doing our best to stay in touch. Similarly, our case managers and our customer service teams stopped what they were doing and did cold calls to our members. An outbound call, there was no script other than, "How are you? Are you coping? Do you have food? Is there anything that you need?" These teams collectively, the community health specialists, the case managers, the customer service representatives, and we'll talk about retail center staff in a second, all are trained to identify any red flags in the social determinants of health and escalate them for additional work directly with our members. If we go to the Florida Blue centers, this is a concept that started in Florida, where we had retail stores in a mall or in a strip mall where our members or potential customers could walk in and have a discussion around health insurance, and what they could or should consider buying. That slowly expanded to having customer service representatives on site, eventually nursing staff on site, and case managers on site. People could wander in and talk to their neighborhood experts in healthcare and health insurance. So when COVID hit, a group of staff also had to pivot and work from home, but they've been doing outbound outreach to our members. Again, it's been very well-received.
Paul Kaplan (00:47:23):
We also have been doing drive-through flu vaccination clinics back in the fall, and hope to very soon, once we are able to somehow secure adequate vaccine supply, do vaccinations either in our retail centers or as drive-through clinics. So work is underway to make that happen. If we go to the slide titled Papa Pals, this is a concept where we've worked with a company that has typically students, and each student is assigned to a Medicare Advantage member. We affectionately call this group-
Paul Kaplan (00:48:03):
... the care advantage member. And we affectionately call this grandkids on demand. These students form a relationship with the senior citizen and are available to help them with anything they need. It could be that they go over to just have a chat, have tea with them, socially interact, play Scrabble, go for a walk with them, and keep them company. If they needed to accompany them to the doctor, if the senior citizen would like that. Pack away groceries. The list goes on and on. And the seniors really like this program. When COVID hit, that also had to transition to a virtual environment with telephone or video discussions. But before the Papa Pals left and went to their own homes, they made sure that their senior citizens that they were responsible for were conversant in how to live in a virtual world so that they would not be alone.
Paul Kaplan (00:49:04):
If we move to the slide ... I should just say one more thing about Papa Pals, and that is that this is a program that is now available statewide, and there's no fee to our members except for our regional PPO members. They pay a slight fee every month and every senior or Medicare advantage member gets assigned a certain number of hours that they can use, like I said, with their pal anyway they like.
Paul Kaplan (00:49:33):
The slide labeled collaboration, the only point I want to make here is we have lots of different staff people in lots of different areas within Florida Blue, who were very focused on loneliness and social isolation, pre-pandemic. And all we have done is pivot our mode of interaction with our members to be virtual, but we have still been very busy and the seniors truly appreciate what we are doing. If we move to transportation very quickly, no big surprise, like most Medicare advantage plans, we offer free transportation for our members to get to their doctors. And during the pandemic, we opened this up to make sure that they could get to grocery stores. We make sure that we have appropriate drivers helping our seniors. We had many complaints where drivers would arrive, wait one or two minutes, and leave impatiently and senior citizens move slower. And it takes them a while to know that their ride has arrived, get out the front door, and to the car. So we're very cognizant of the need to assist any way we can to make sure that this is a good experience for our members. We are going to be using this transportation benefit to get people to vaccination clinics moving forward. Which gives me one more minute. I'll take on vaccination clinics. Florida took its lead, as did every state, from the Governors. And we have been focused on getting health care professionals, and then people age 65 and older vaccinated. That was what our Governor, Governor DeSantis, asked of us to do, and it is working. There've been about 780,000 people vaccinated as of January the 13th. I don't have more up-to-date figures. And despite everything you hear, it's actually starting to improve in terms of the pace with which people get vaccinated. The grumblings that we heard are starting to dissipate. These states, and again, I can only talk for Florida, decentralized everything and allowed every County to decide how they would distribute the vaccine and administer the vaccine. And the question becomes, so what do we, as a health insurance company, as a payer, do with all of this? And so what we've started doing is we've said, "We know a population extremely well. Who's highest risk? Who do we need to get to?" And facilitate getting them to a vaccination clinic.
Paul Kaplan (00:52:22):
We're working with the people who have the vaccine so that we know when they have vaccine. We're working on identifying the people who are willing to get the vaccine. And then we will push information to them saying, "We are aware that there will be vaccine available and we'll give the address, and this is how you sign up to get a time slot." We believe that a partnership with people who have the vaccine or will soon have it, and the people who will administer the vaccine, and as with our data, and the ability to connect with people, is the most efficient way to move people in the population through their vaccination. And we are very, very confident that things will smooth out. I'm going to hand it back to the moderators. I went fast. I do apologize, but this gives time for questions.
Caitlin Ellis (00:53:18):
Great. Thank you so much, Dr. Kaplan, for sharing your experience implementing these community-based strategies to improve the health and wellbeing of older adults. And for sharing health, Florida Blue is supporting people during the vaccination effort. We would like to use the remaining time to engage in a Q&A session with our audience. Please continue to submit your questions in the Q&A tab. I will ask all of our panelists to come off of mute. And I'm just going to start with a question that we kind of, we touched on it a little bit around the fact that there's a lot of state variation and local variation on when and how people can get vaccines. And so I was wanting to ask, is there a place where people can get timely information at a local level about when they can get a vaccine and where? I don't know Dr. Newman, if you'd like to ...
Tricia Neuman (00:54:08):
[crosstalk 00:54:08] Sure. I will jump in on that. No, I wish there ... I mean, I wish there was one answer to that question. I think the challenge here is that there are many, many different answers to that question, which varies depending upon where people live. I've started thinking, "Wouldn't it be great if there was a 1-800-MEDICARE number that people, older people could call to get this answer?" But for now it seems that what most people are doing is calling their doctors. If their doctors happen to know, they're telling them, but really that the it's up to the local governments. So some people are calling their County offices. Some people are calling their city offices. Many people need ... If you Google, you might be able to find, depending on where you live, where it is that you can sign up for a vaccination.
Tricia Neuman (00:54:59):
People who are affiliated with professional organizations might hear through that. So people who are, for example, 65 and older, may not get the same sort of direct email that someone would get if they were a dentist or a doctor or a social worker, who's got a professional organization. So the truth is I think people need to look all over the place. There's not one answer. It's a challenge. Hopefully there will be some sort of consolidated way of getting people information, but for now, I would call state resources, city resources, possibly check with local pharmacies until there is a clear way of getting information.
Vincent Mor (00:55:45):
So this is more-
Caitlin Ellis (00:55:47):
[crosstalk 00:55:47] Great, thanks.
Vincent Mor (00:55:50):
CVS and Walgreens has got, will be starting to go with their customers, at least, and sending out texts to their customers, their pharmacy customers, to try to schedule them to come into the store for vaccinations. They're going to have every store, regardless of whether they have a pharmacy or not, is supposed to be set up to do vaccinations. That is supposed to all come from their pharmacy records structure. That's supposed to start in a couple of weeks. I'm not sure exactly how the triage is working, nor do I know whether it's going to be happening differentially from one state to the other.
Tricia Neuman (00:56:34):
I mean, I also will say, it's not clear how things will change with the new administration, if there will be a more consolidated way of organizing where vaccines are available and communicating to people. I also know that healthcare providers, like hospitals, are reaching out to patients that are in their system to let them know that they may be contacted when they get in the queue. But again, it sort of varies by pharmacy, it varies by healthcare provider, and it varies by where people live.
Caitlin Ellis (00:57:11):
Great. Thank you so much for sharing that information. We had a few questions come in around vaccine hesitancy, specifically around nursing homes or long-term care staff. And questions about how do we address these findings that nursing home staff are hesitant to get vaccinated. And that even during the height of the pandemic, many nurses, aides were afraid to even get tested, given that they didn't have a safety net economically, and that if they were tested positive, they would be sent home. Can you give any insights on what kind of strategies to address this hesitancy going forward?
Vincent Mor (00:57:45):
So this is Vince. Let me just provide some information. So first of all, there are a lot of materials out there for frequently asked questions, et cetera, that the nursing home companies, as well as the associations, are trying to distribute and disseminate, but it's a difficult process reaching everyone who is a worker, and it has to be done in multiple languages because not everyone's all that comfortable with English, particularly on relatively technical subjects. But the disinformation and misinformation that's out there on the various parts of the web is kind of, as usual, shocking and astounding. And some of it has political overtones. It has a religious overtone, but there's a lot of simple concern that is associated with safety and distrust of institutions in general.
Vincent Mor (00:58:40):
With respect to ... So in the analysis we've done so far with regard to staffing, it does not look like that staff who previously tested positive are any more or less likely to get the vaccination now. So it doesn't look like it's an experiential thing, but, and it's also highly variable from one building to the next. And so the key is trying to find influential people who are trusted to deliver the message in a way that people can accept it and where it's, you're doing something positive for somebody else, for your patients or for your family, you're going to get the shot. And that's a difficult message because you have to sort of overcome, not just the hesitancy, but the information based that might be creating the hesitancy. It's complicated.
Caitlin Ellis (00:59:38):
Great. Thank you. Unfortunately, we are out of time today. I did want to note that we are working to make a transcript available, alongside our archive video, in case you missed a portion of the presentation today. I would like thank our excellent panel of speakers for being with us and sharing their valuable work and perspectives. And thank you for our audience for joining us today. Your feedback is important. So please take a moment to complete a brief survey, which can be found at the bottom of your screen. And I would like to add that we do have some additional resources available on our website, including our recent infographic on loneliness, a recent webinar on vaccine distribution efforts in the future of the COVID-19 response, and additional materials from our speakers, as well as their slides. Thank you again for joining us today.
Presentations
The Challenges of Aging During COVID-19: Long Term Care, Vaccination, and Isolation

Tricia Neuman, ScD
Kaiser Family Foundation
Risk Factors Associated With All-Cause 30-Day Mortality in Nursing Home Residents With COVID-19
Temperature Screening for SARS‐CoV‐2 in Nursing Homes: Evidence from Two National Cohorts
Variation in SARS-CoV-2 Prevalence in U.S. Skilled Nursing Facilities
Tradeoffs Podcast: We Need You; Vaccine Hesitancy in Nursing Homes
Patterns in COVID-19 Cases and Deaths in Long-Term Care Facilities in 2020
One in Four Older Adults Report Anxiety or Depression Amid the COVID-19 Pandemic
COVID-19 Data in Long-Term Care Facilities
FAQs on Medicare Coverage and Costs Related to COVID-19 Testing and Treatment
Racial and Ethnic Disparities in COVID-19 Cases and Deaths in Nursing Homes
Key Questions About Nursing Home Regulation and Oversight in the Wake of COVID-19
COVID-19: Who is at Most Risk of Serious Illness (video)
How Many Adults Are at Risk of Serious Illness if Infected with Coronavirus?
Who Didn’t Get a Second Shingrix Shot? Implications for Multidose COVID-19 Vaccines
What Share of People Who Have Died of COVID-19 Are 65 and Older – and How Does It Vary By State?
More Related Content
See More on: Coronavirus | Social Determinants of Health